1. Pröhl A et al. 2021. In Vivo Analysis of the Biocompatibility and Bone Healing Capacity of a Novel Bone Grafting Material Combined with Hyaluronic Acid. Int J Mol Sci. May 1;22(9):48.
2. cerabone® plus usability test, data on file.
3. Customer survey cerabone® plus including 156 clinicians, data on file.
4. Tadic and Epple 2004. A thorough physicochemical characterisation of 14 calcium phosphate-based bone substitution materials in comparison to natural bone. Biomaterials. 25(6):987-94.
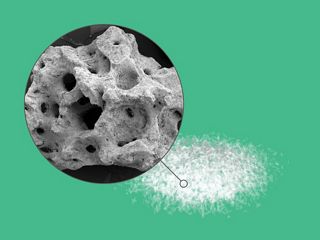
5. Seidel and Dingeldein 2004. cerabone® – Bovine Based Spongiosa Ceramic Seidel et al. Mat.-wiss. u. Werkstofftech. 35:208–212
6. Vanis et al. 2006. Numerical computation of the porosity of bone substitution materials from synchro-tron micro computer tomographic data Mat.-wiss. u. Werkstofftech. 37, No. 6.
7. Tadic et al. 2004. Comparison of different methods for the preparation of porous bone substitution ma-terials and structural investigations by synchrotron l-computer tomography Mat.-wiss. u. Werkstofftech. 35, No. 4.
8. Trajkovski et al. 2018. Hydrophilicity, Viscoelastic, and Physicochemical Properties Variations in Dental Bone Grafting Substitutes. Materials (Basel). 30;11(2). pii: E215.
9. Tawil et al. 2016. Sinus Floor Elevation Using the Lateral Approach and Bone Window RepositioningI: Clinical and Radiographic Results in 102 Consecutively Treated Patients Followed from 1 to 5 Years. Int J Oral Maxillofac Implants. 31(4):827-34.
10. Tawil et al. 2018. Sinus Floor Elevation Using the Lateral Approach and Window Repositioning and a Xenogeneic Bone Substitute as a Grafting Material: A Histologic, Histomorphometric, and Radio-graphic Analysis. Int J Oral Maxillofac Implants.33(5):1089–1096.
11. Riachi et al. 2012. Influence of material properties on rate of resorption of two bone graft materials af-ter sinus lift using radiographic assessment. Int J Dent. 2012:737262.
12. Lorean et al. 2014. Nasal floor elevation combined with dental implant placement: a long-term report of up to 86 months. Int J Oral Maxillofac Implants. 29(3):705-8.
13. Fienitz et al. 2016. Histological and radiological evaluation of sintered and non-sintered deproteinized bovine bone substitute materials in sinus augmentation procedures. A prospective, randomized-con-trolled, clinical multicenter study. Clin Oral Investig. 21(3):787-794.
14. Khojasteh A et al. 2016. Tuberosity-alveolar block as a donor site for localised augmentation of the maxilla: a retrospective clinical study. Br J Oral Maxillofac Surg. 2016 Oct;54(8):950-955.
15. John et al. 2009 Perspectives in the selection of hyaluronic acid fillers for facial wrinkles and aging skin. Patient Prefer Adherence. Nov 3;3:225-30.
16. Stern R, Asari AA, Sugahara KN. Hyaluronan fragments: an information-rich system. Eur J Cell Biol. 2006 Aug;85(8):699-715. doi:10.1016/j.ejcb.2006.05.009. Epub 2006 Jul 5. PMID: 16822580.
17. Kyyak et al. 2021 The Influence of Hyaluronic Acid Biofunctionalization of a Bovine Bone Substitute on Osteoblast Activity In Vitro. Materials (Basel). 2021 May 27;14(11):2885.
18. Rothamel et al. 2012. Biocompatibility and biodegradation of a native porcine pericardium membrane: results of in vitro and in vivo examinations. Int J Oral Maxillofac Implants.27(1):146-54. 19. Brown et al. 2000. New studies on the heat resistance of hamster-adapted scrapie agent: threshold survival after ashing at 600 degrees C suggests an inorganic template of replication. Proc Natl Acad Sci U S A. 28;97(7):3418-21.
20. Murugan et al. 2003. Heat-deproteinated xenogeneic bone from slaughterhouse waste: Physico-chemical properties Bulletin of Material Science Volume 26, Issue 5, pp 523–528.
21. Perić Kačarević et al. 2018 Purification processes of xenogeneic bone substitutes and their impact on tissue reactions and regeneration. Int J Artif Organs. 2018 Nov;41(11):789-800.
22. cerabone® usability test, data on file.
23. Barbeck M et al. 2014. High-Temperature sintering of xenogeneic bone substitutes leads to increased multinucleated giant cell formation: In vivo and preliminary clinical results. The Journal of oral implan-tology. 4110.1563/aaid-joi-D-14-00168.