Surgery
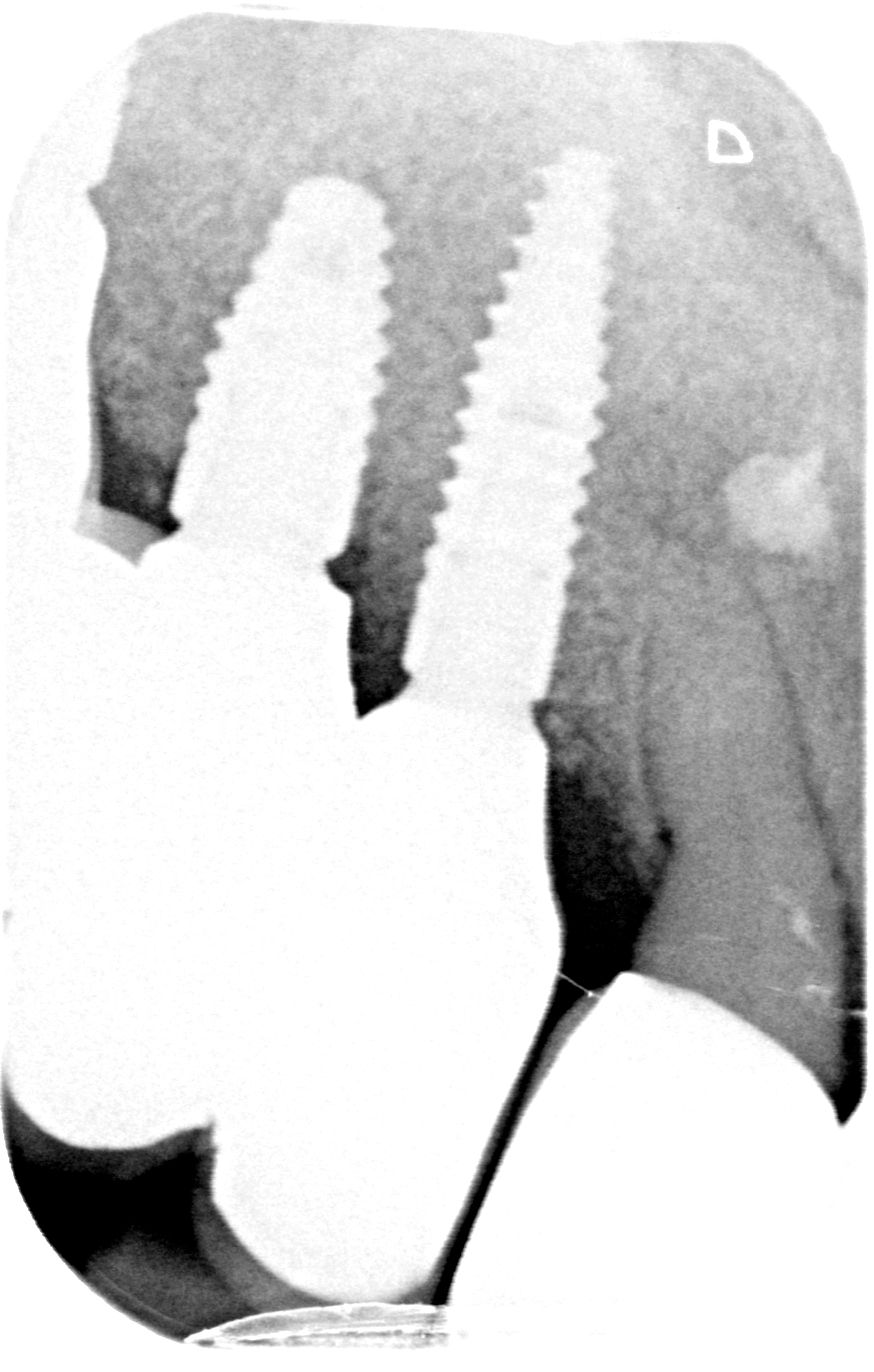
Premedication consisting of 2.25 mg of amoxicillin and 600 mg of ibuprofen were given one hour prior to surgery, and the patient rinsed her mouth with a chlorhexidine solution for one minute. Next, a mucoperiosteal flap was raised (Figs. 5-6) and a 6x7mm window prepared in the lateral sinus wall (Fig. 7). With the help of a surgical stent, the implant positions were determined using the 2.2 pilot drill (Figs. 8-9). As expected, a horizontal defect was found in positions 12 and 13. A trephine bur with external and internal diameters of 7 and 6 mm, respectively, was used to prepare the bed for a 6 mm botiss maxgraft® bonering (Figs. 10-11), paying particular attention not to perforate the palatal wall or remove too much of the patient's own bone. A planator was used to create a flat surface at the bottom of the trephined area in order to produce a perfect fit for the bonering. The maxgraft® bonering was adapted to the desired length using the holding instrument (Fig. 12), and a 2.8 mm bur was used for the final drilling procedure. After soaking the bonering for several minutes in the patient’s blood (Fig. 13), a 3.3x12mm Straumann BLT Implant (SLA®) was placed in position #12 through the bonering, which was tightened and compressed to the recipient bone (Fig. 14). Since the implant and bonering stability were excellent, no membrane screw was needed to further stabilize the ring, and a 0.5mm NC cover screw was placed. In position 13, a 4.1x8 mm Straumann BLT implant (SLA®) was placed inside the newly formed bony contour, and the harvested bone was collected. Meanwhile, the trephine bur for the implant in position #12 was used to augment the bone buccally to the implant at #13 (Fig. 15). In position 16, a sinus lift procedure was performed, keeping the Schneiderian membrane intact and using a xenogenic bone augmentation material while placing a 4.1x10 mm RC Straumann BLT (SLA®) Implant. Guided bone regeneration was done, covering the lateral window of the sinus, the implant in position 12 with the botiss maxgraft® bonering and the implant in position 13 with a xenogenic bone substitute and 20x30 botiss Jason® membrane (Fig. 16). The position of the implants was rechecked by means of x-rays (Figs. 17-18). Titanium pins were used to immobilize the membrane. After a periosteal releasing incision, the flap was sutured without tension (Fig. 19). The sutures were removed ten days later and the wound healing was good. Six months later, an apically repositioned split-flap was performed to augment the amount of attached gingiva bucally to the implant, and three Straumann gingiva formers were placed. After suture removal, the patient was sent back to the referring dentist for the subsequent prosthetic procedures and finalization of the implant-mounted screw-retained reconstruction.