Get exclusive access to Dr. Chen's presentation
Roxolid® shows increased
anti-inflammatory potential* vs Titanium2
Advanced biocompatibility studies and latest osseoimmunology insights suggest that Roxolid® is biologically superior to Ti, as Roxolid® implants stimulate an early anti-inflammatory cell response. Our immune system favors Roxolid. * in vitro
Clinical Oral Implants Research4
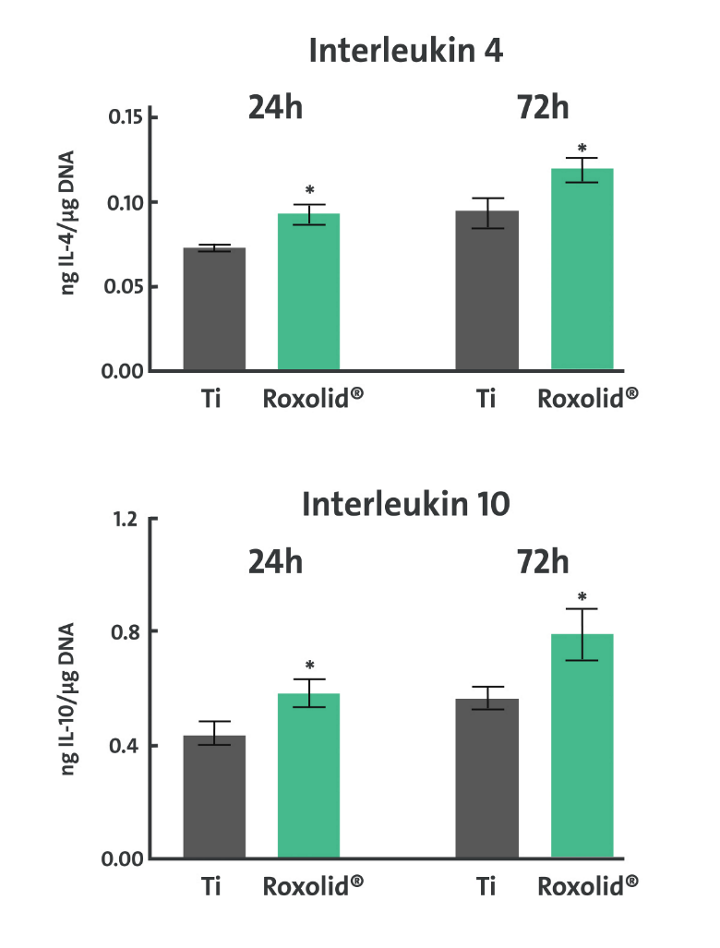
How does Roxolid® show increased anti-inflammatory potential over Titanium?
The choice of material used for medical implants plays a critical role in how the body responds post-surgery, particularly concerning inflammation. In-vitro studies have revealed that human macrophages cultured on Straumann® Roxolid® compared to those grown on Titanium exhibited a significant increase in their anti-inflammatory response, manifested by increased levels of Interleukin 4 and Interleukin 10.At the same time, a greater reduction of pro-inflammatory response indicated by down-regulation of Interleukin1β, Interleukin 6, and TNFα, was observed for Straumann® Roxolid® when compared with Titanium.
Watch Dr. Stephen Chen's presentation and receive a discount code for our eShop. Don't miss out!
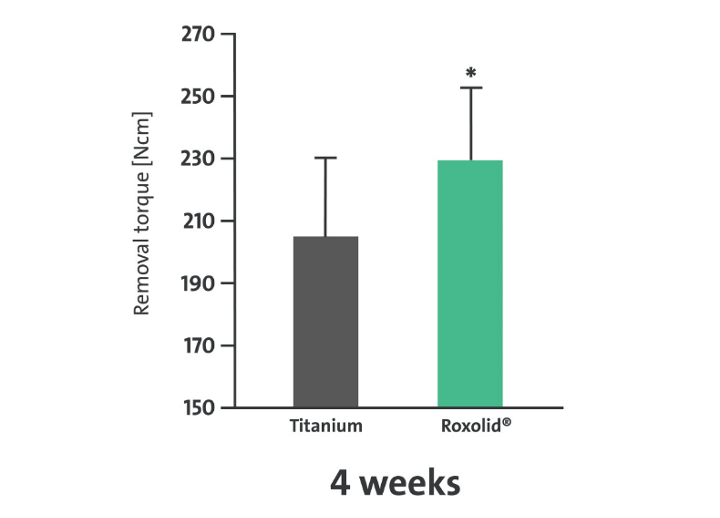
Roxolid® facilitates stronger
osseointegration
The favorable immune response facilitates early healing and superior osseogenesis. In fact, in vivo research reported significantly higher removal torques for Straumann® Roxolid® implants compared to Ti implants, confirming the superior bone quality surrounding Roxolid® implants and higher quality of osseointegration.
Clinical Implant Denistry and Related Research3
Clinical Oral Implants Research4
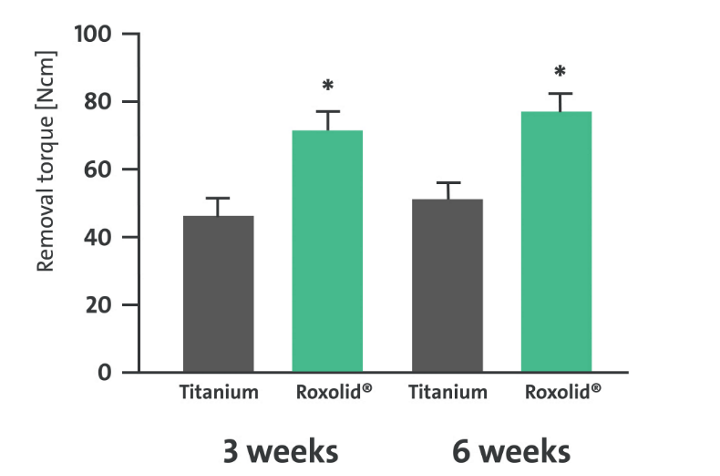
How does Roxolid® facilitate stronger osseointegration over Titanium?
Osseointegration starts with initiation at the implant-bone interface of multiple processes leading to 1) bone healing and 2) the establishment of a strong and stable implant-to-bone connection on the molecular level. This complex sequence of events is modulated by a number of molecules known to facilitate this process, with their functional proficiency potentially influenced by the implant material composition. Galli and collaborators have reported that when compared to Titanium, Roxolid® material significantly increased gene expression of the molecules involved in early healing and osteogenesis response including growth factors, extracellular matrix proteins, cell attachment markers, osteoclasts markers, and cytokines.
Supplementary insights from Wen et al. 2014, and Gottlow et al. 2012 reinforced these findings. They reported significantly higher removal torques for Straumann® Roxolid® implants in vivo compared to Titanium implants, confirming the superior bone quality surrounding Roxolid® implants, thus higher degree/quality of osseointegration.
Watch Dr. Stephen Chen's presentation and receive a discount code for our eShop. Don't miss out!

Roxolid® – Not only stronger –
also biologicaly superior
Newly published long-term clinical data shows that Roxolid® implants delivered 98.9% survival rate after 10 years in a double-blind randomized controlled multi-center study.
implant survival
after 10 years1
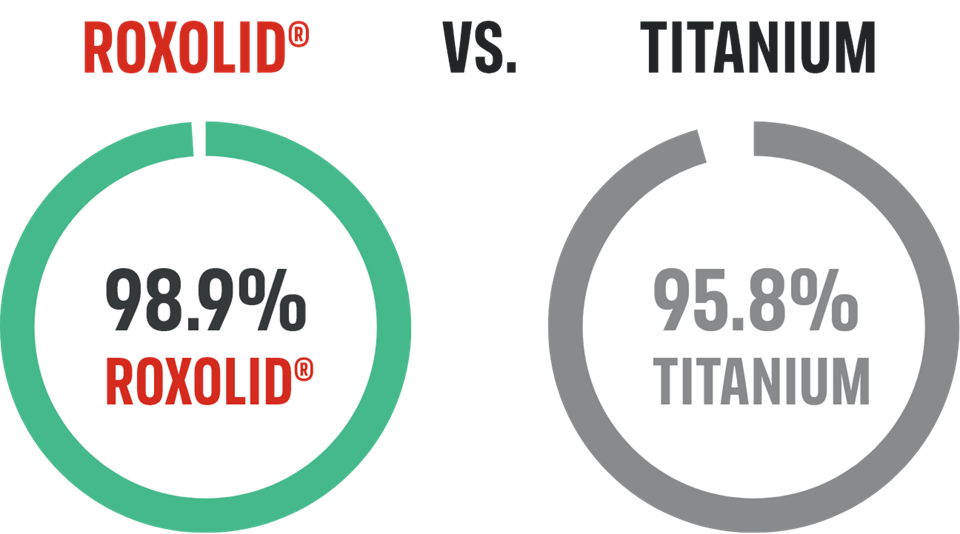
Double-blind randomised controlled multi-center clinical trial.1
The latest insights from osteoimmunology show that Roxolid® elicits a more favorable immune response than does Ti.
In fact, the advanced biocompatibility studies show that Roxolid® is biologically superior to Ti when it comes to immune response and osseointegration strength.
Watch Dr. Stephen Chen's presentation and receive a discount code for our eShop. Don't miss out!
1.
ROXOLID® stronger than titanium
Stronger material.
Stronger implant.
*Bernhard N et al.; Forum Implantologicum 2009 ; 5(1): 30-39
2.
Roxolid® helps avoid invasive grafting procedures
Straumann® Roxolid® reduces invasive bone grafting procedures with smaller and stronger Roxolid® implants.
helpS avoid bone augementation
Journal of Implantology5
Clinical Oral Implants Research
∅3.3 mm Roxolid® implants “may predictably bear the mechanical stresses generated by occlusal loading (…) in the lateral-posterior areas”.6
3.
reduces invasiveness and preserves bone
Stronger material allows a smaller implant.
Roxolid® reduced-diameter implants have multiple advantages over their regular-diameter counterparts
- Reduced drilling
Preserves vital structures and vascularization - Easier placement
Saves time and patient discomfort - Better fit in narrow spaces
Leads to reduced treatment complexity
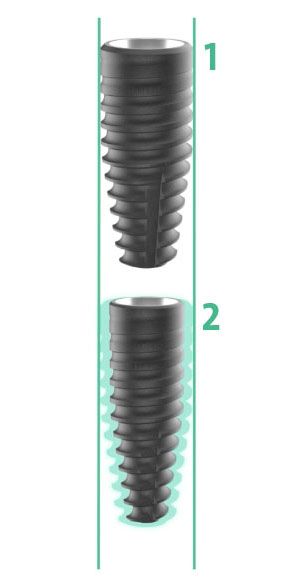
1 Straumann® BLT Titanium ∅4.1
2 Straumann® BLT Roxolid® ∅3.3
Less drilling means enough bone
Smaller/shorter Roxolid® implants

Reduce drilling, preserve bone, vital structures and vascularization

Maintain thicker buccal bone when placing the implant

Increase treatment options in challenging anatomical situations and narrow interdental spaces
4.
roxolid® maximizes esthetics
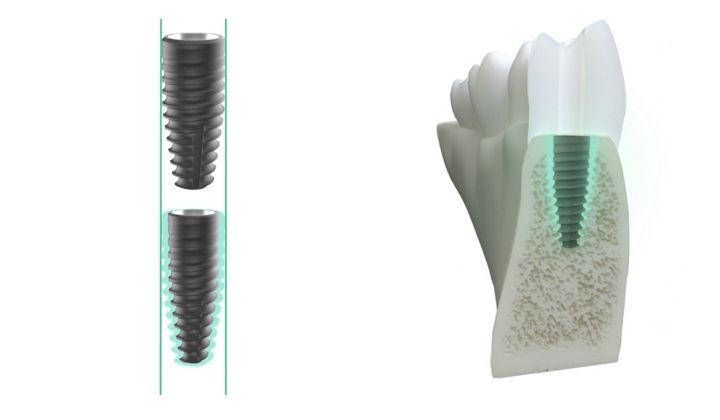
Maximize the space for the bone and soft tissues with Roxolid® BLT Ø2.9mm.

Less
invasive

Reliable with highly
esthetic outcomes
Roxolid® Ø2.9MM implant
Small enough to fit – strong enough to last.
Based on a legendary scientific concept with an impressive track record. This diameter-reduced implant is the ideal implant solution for narrow interdental spaces and narrow bone ridges: Less invasive and highly reliable with convincing results. A perfect combination of implant design, strength and healing effect. The novel prosthetic design resembles the anatomy of natural teeth. Thanks to Roxolid®, another solid and reliable treatment option is now available.

5.
roxolid® increases treatment options in anatomically challenging situations
Avoid bone augmentation for limited bone height with Roxolid® 4mm short implant.
Roxolid® 4MM short implant
Reduced invasiveness through use of shorter implants.

Roxolid® 4mm short implant is the shortest screw-type implant with internal connection on the market, providing even more treatment options.
- Perfectly suitable for the treatment of partially and fully edentulous patients with very limited vertical bone availability in the posterior region
- Possibility to treat patients without complex vertical bone augmentations.
Watch Dr. Stephen Chen's presentation and receive a discount code for our eShop. Don't miss out!