Introduction
In this case report, we present a young male patient referred for the extraction of tooth #11 due to a horizontal root fracture. The patient, concerned with the functional and esthetic impact of losing his front tooth, requested a durable and fixed solution. Clinical and radiographic examinations confirmed the need for extraction and showed sufficient bone support for immediate implant placement. Given the patient’s high smile line and gingival recessions in adjacent teeth, a precise treatment plan was necessary to achieve optimal functional and esthetic outcomes.
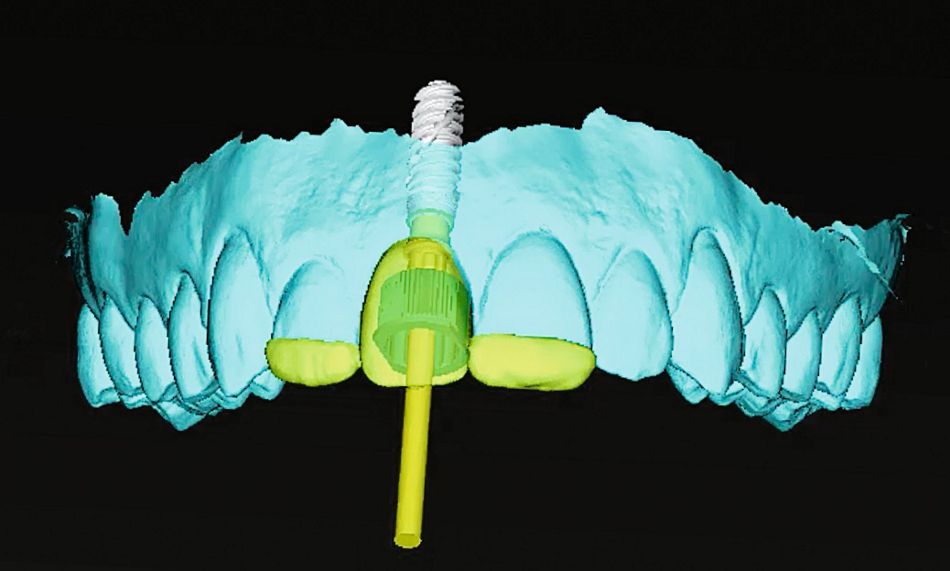
Leveraging a fully digital workflow within our practice, we chose to collaborate with the Smile in a Box™ team for assistance. This allowed us to streamline the surgical and prosthetic phases, outsourcing the production of the surgical guides and temporary implant prostheses. Additionally, we maintained full control over the surgical planning using coDiagnostiX® software, ensuring a personalized approach tailored to the patient's unique needs.
This report highlights the use of Smile in a Box™ for immediate extraction and implant placement in the esthetic zone, showcasing the benefits of precision, predictability, and efficiency in digital dentistry. Through this integrated approach, the patient received an immediate functional and esthetic restoration, resulting in high satisfaction and outstanding clinical outcomes.
Initial situation
A young male patient arrived for a consultation, referred by his endodontist for the extraction of tooth #11, which presented a horizontal root fracture. The patient had already been informed that he was going to lose the front tooth and desired a durable, fixed, functional, and esthetic solution.
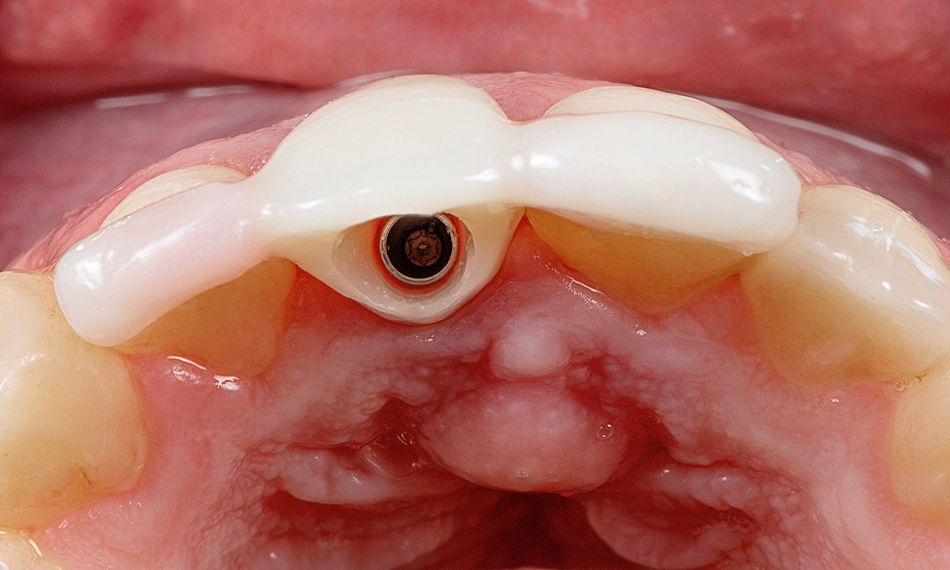
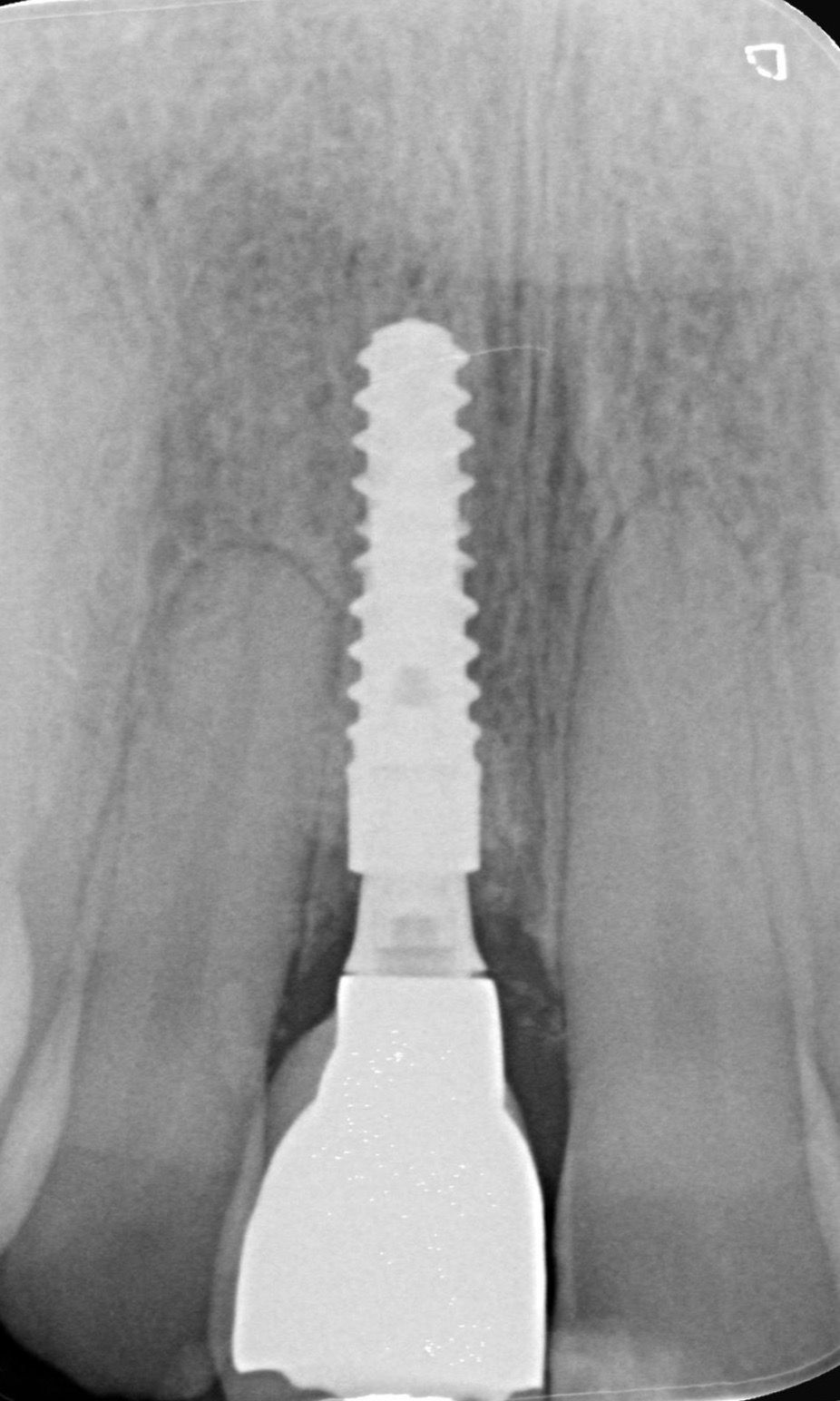
The patient’s medical history revealed no significant findings, and intraoral examination showed good oral hygiene. Tooth #11 exhibited discoloration and grade II mobility; no bleeding on probing was noticed. A high smile line and a healthy amount of keratinized tissue surrounding tooth #11 were observed. The patient also presented marked recessions in the adjacent teeth. Radiographic examination showed sufficient mesiodistal width and an adequate distance from adjacent teeth.
Based on clinical and radiological assessments, the horizontal root fracture was confirmed (Figs. 1,2).