Introduction
Evidence has shown that there is no requirement for complete socket healing, and both tooth extraction and implant insertion can be accomplished in a single surgical session2,3. As for the scientific evidence on the posterior area, Hayacibara et al. indicated that, when carefully planned, executed, and monitored, immediate implants of mandibular molars are a feasible surgical treatment with a high success rate4.
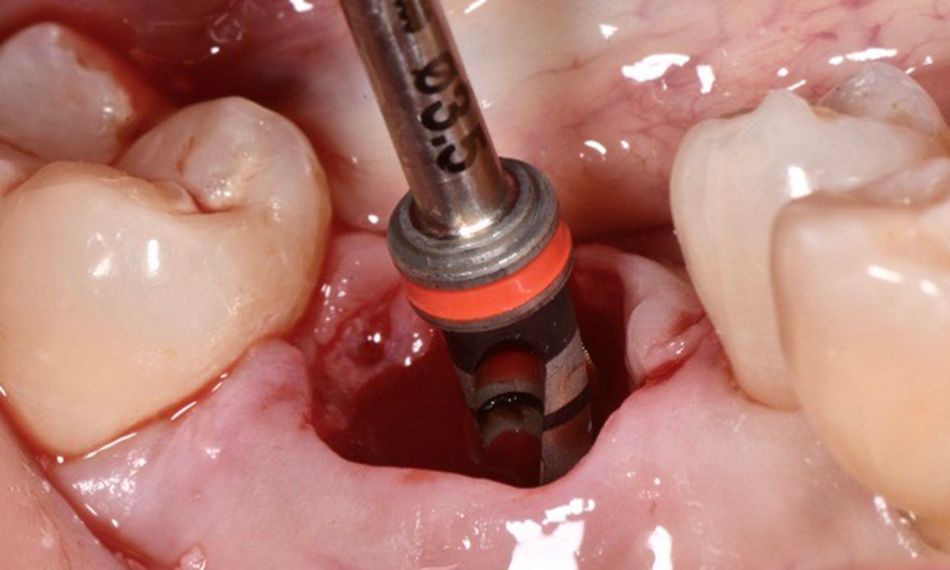
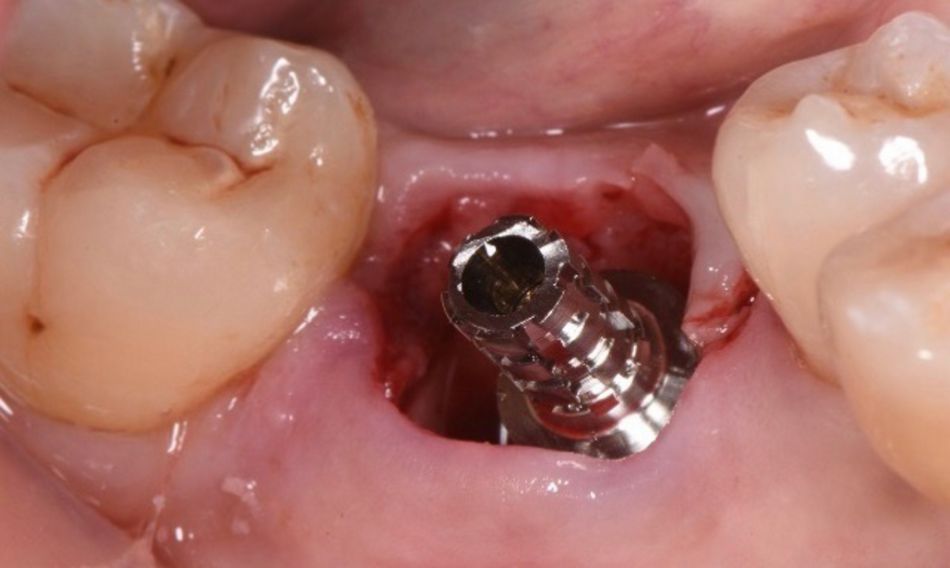
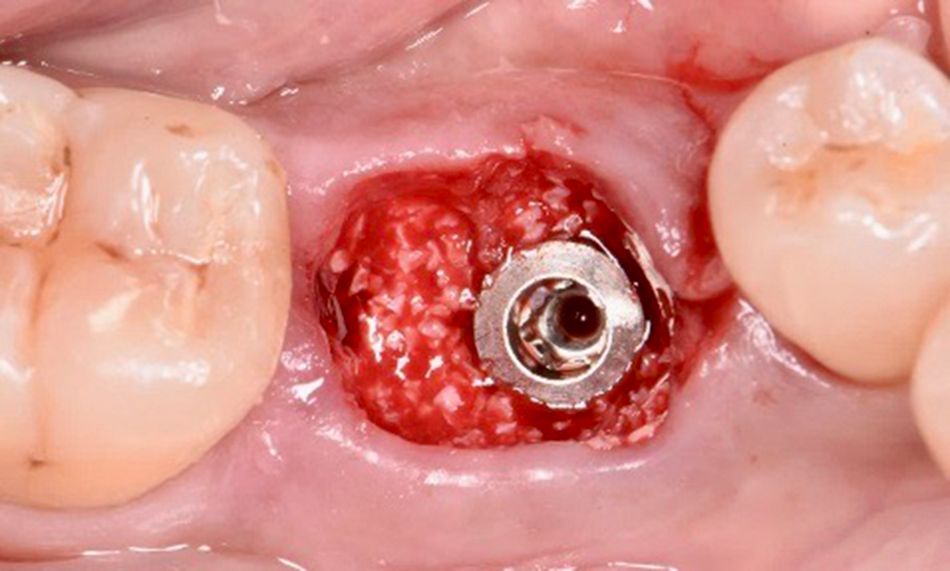
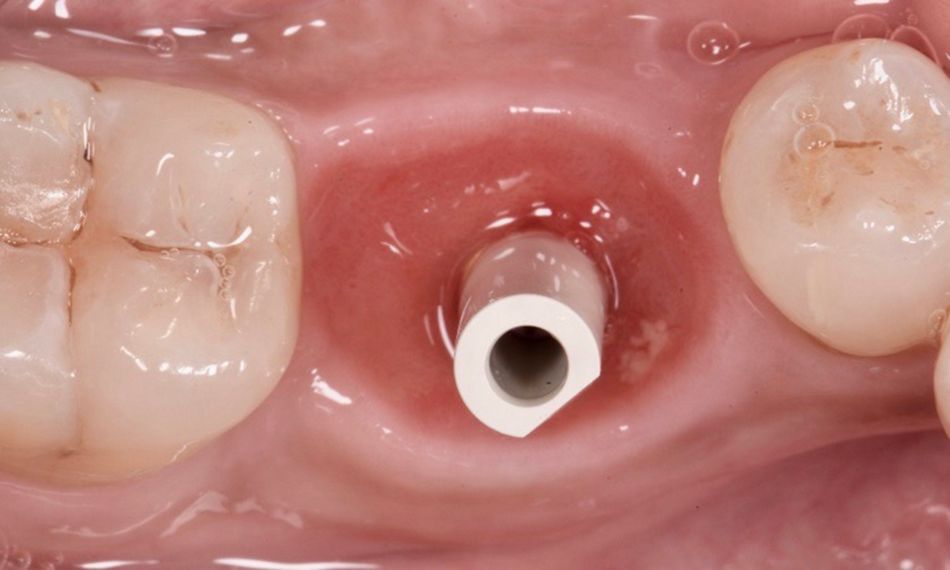
The following case report presents the treatment of a patient with immediate implant placement and bone grafting in a lower molar site. The Straumann® BLX with Roxolid® material and SLActive® surface was chosen for this situation as it allows us to achieve an optimal primary stability and predictable outcomes, enabling confidence for early implant insertion.
Initial situation
A healthy 48-year-old female non-smoker with no medication or allergies came to our clinic reporting pain in the lower right first molar. She stated that she had had this condition for the past few weeks, and that it was not improving and was aggravated by chewing. Since this situation was affecting her quality of life as she was not able to eat properly, her main wish was to have an immediate solution that would improve her quality of life.
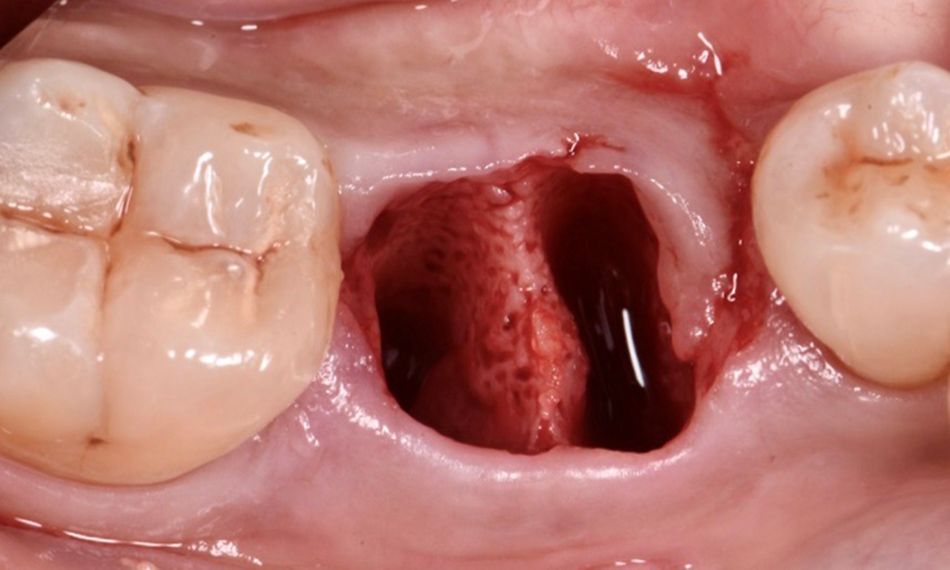
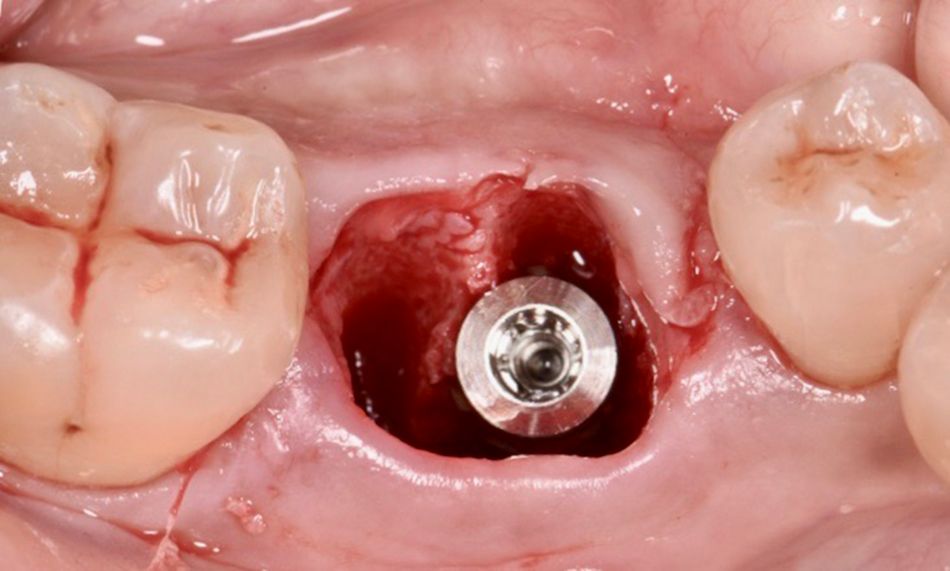
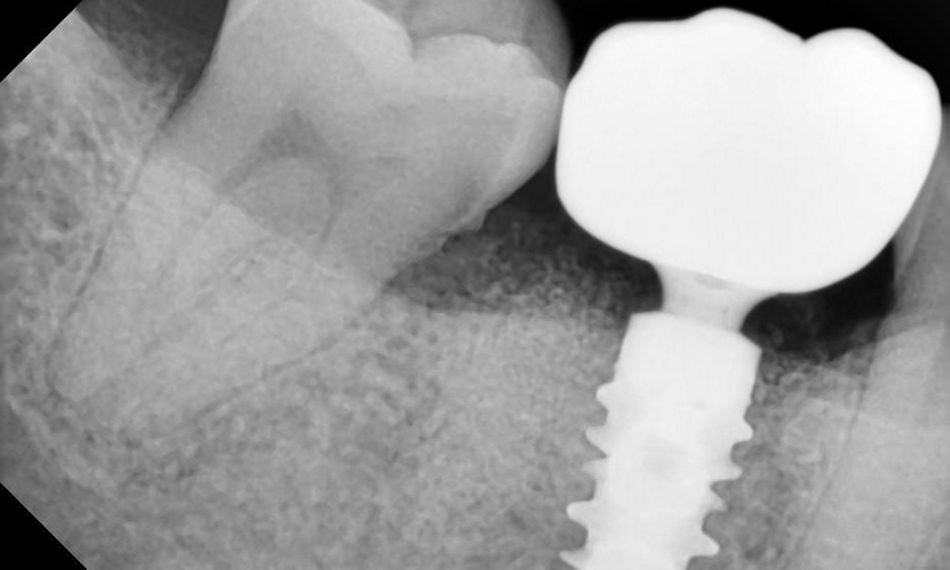
The extraoral examination showed a medium smile line. The intraoral examination revealed a coronal fracture on tooth #46 with a buccolingual crack line involving the pulp horn extending below the alveolar bone level. The tooth was painful to percussion and did not exhibit mobility. No caries or restoration was present (Fig. 1). Periodontal probing revealed deep pockets on the buccal and lingual sides of #46.
The radiographic assessment confirmed the fracture line below the crest of the alveolar bone on #46. The prognosis was not favorable.
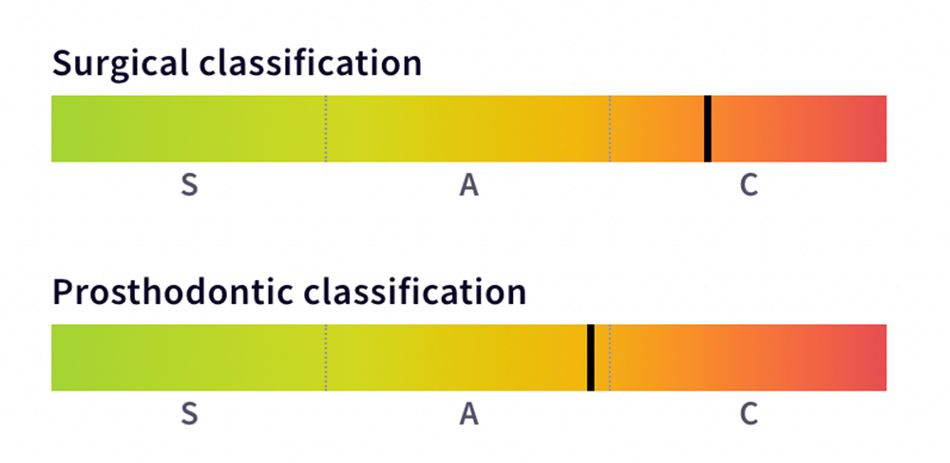
The SAC classification in implant dentistry was used to evaluate the degree of complexity and risk concerned with implant-related rehabilitation. Regarding the surgical and prosthodontic classification, the patient was considered complex and advanced, respectively (Fig. 3).