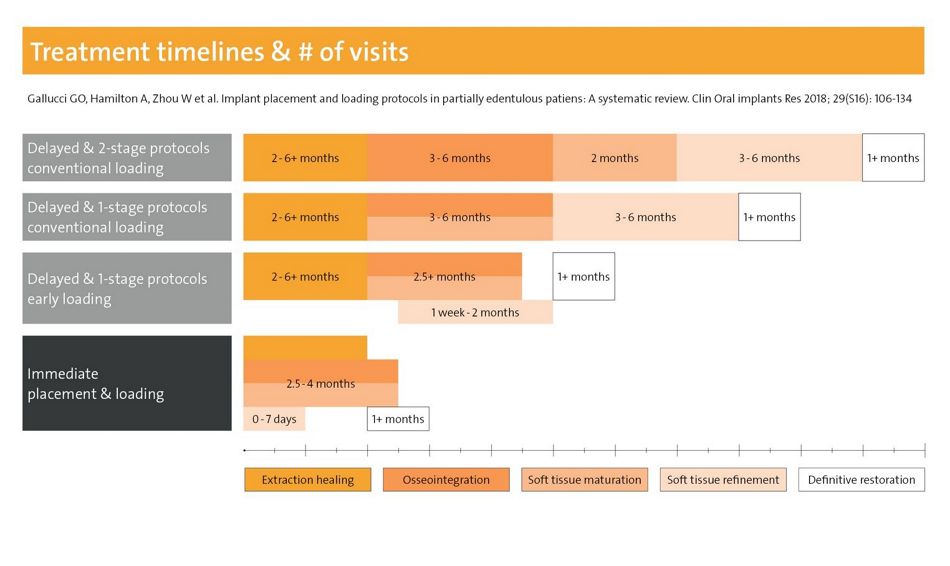
Fig. 1: Treatment duration and number of visits can be significantly reduced with immediate or early placement and restorative protocols
(with courtesy of Leziy/Miller, taken from here).
To preserve precious tissues and meet patient expectations implants should be placed within the first four months after tooth extraction. According to the latest ITI consensus paper, this is “due to the risk of alveolar resorption and reduction in bone volume, as well as the extended treatment time” for Type 4 placement (6 months or later)1, 3. Alternatively, a post-extraction (Type 1) or early (Type 2 or 3) implant insertion is preferable. Decisions will depend on diagnostic findings, e.g. as proposed in the SAC classification by the International Team for Implantology (ITI), and on the clinical expertise of the team4-6.
According to recent conference presentations, immediate placement can be indicated in sockets with more than 50% intact walls and thick biotypes. Risk factors include a non-optimal implant diameter or situations where primary stability requires a prosthetically non-optimal implant position (Dr Frank Schwarz, Germany, presentation at the Europerio 2022). According to Dr Ronald Jung (Switzerland) dedicated tissue level implants (Straumann® TLX, details see below) are optimized for immediate protocols in posterior areas.
Moreover, clinicians should be aware that physiological soft tissue thickening after extractions may mask an extended bone defect in patients with thin soft tissue types7. Therefore soft tissue or GBR augmentations are often indicated in connection with immediate or early implant placement4. For these indications different xenogeneic (e.g. Straumann® Xeno Graft) or allogenic grafting materials are available, which can be complemented by, e.g., the flexible Jason® collagen membrane.

Fig. 2: Both the Straumann® BLX (Bone Level) and Straumann® TLX (Tissue Level) Implant Systems have an identical deeply structured endosteal thread macro design. There is only one surgical tray for both systems, which allows to adapt the protocol to the intra-operative situation.
Implant systems designed for stability
Modern implant designs can enhance and simplify time-saving insertion and restorative protocols. For increased primary stability especially in soft bone, specific macro designs have been developed8, 9. For example, the Straumann® BLX implant system (Fig. 2) improves bone management, e.g. by means of a conical shape of the implant body with reduced neck diameter, deeply structured threads, bidirectional cutting and bone condensing properties. The thread design was transferred to the Straumann® TLX implant system (Fig. 2). Other Straumann® implants systems including the Zygomatic™ are equally compatible with digital and immediate placement or restorative options.
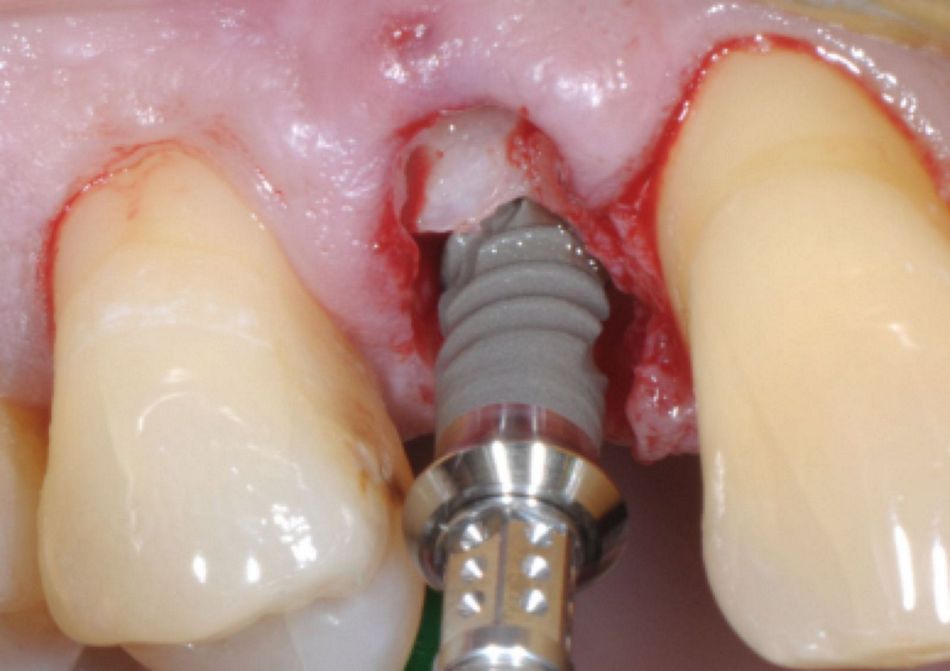
Fig. 3: The Straumann® TLX implant combines a smooth transgingival collar with an aggressive thread design optimized for high primary stability
(picture courtesy of Dr Mario Rocuzzo, see full case report here).
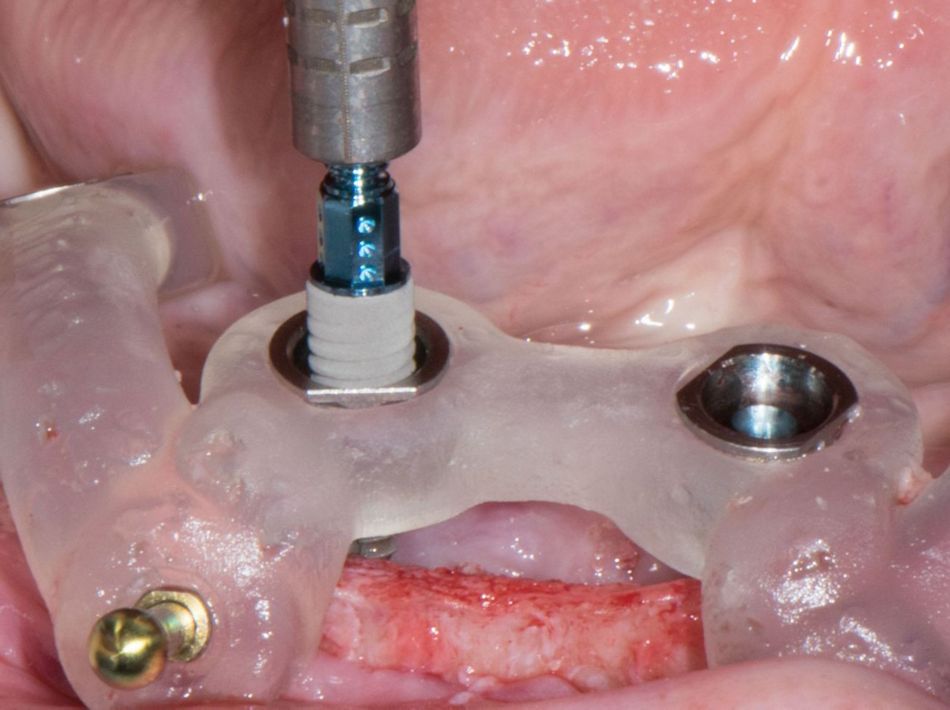
Fig. 4: Straumann® BLT implants are being used for this full arch case with fully guided surgery and immediate temporary loading
(picture courtesy of Dr Nikolay Makarov, see full case report here).
To enhance osseointegration and provide maximum secondary stability during bone remodeling (after 2-4 weeks), a chemically modified surface has been developed (Straumann® SLActive®)10, 11. This is especially relevant in connection with early loading or in patients with compromised systemic health12. The highly stable implant material Straumann® Roxolid® adds maximum fracture resistance. This combination of macro, micro and chemical implant features increase the predictability of immediate and early protocols. Finally, with transgingival healing only one surgery is needed in many cases.
References:
- Gallucci GO, Hamilton A, Zhou W, Buser D, Chen S. Implant placement and loading protocols in partially edentulous patients: A systematic review. Clin Oral Implants Res 2018;29 Suppl 16:106-134.
- Fortes JH, de Oliveira-Santos C, Matsumoto W, da Motta RJG, Tirapelli C. Influence of 2D vs 3D imaging and professional experience on dental implant treatment planning. Clinical Oral Investigations 2019;23:929-936.
- Morton D, Gallucci G, Lin WS, Pjetursson B, Polido W, Roehling S, et al. Group 2 ITI Consensus Report: Prosthodontics and implant dentistry. Clin Oral Implants Res 2018;29 Suppl 16:215-223.
- Buser D, Chappuis V, Belser UC, Chen S. Implant placement post extraction in esthetic single tooth sites: when immediate, when early, when late? Periodontol 2000 2017;73:84-102.
- Buser D, Chen S. Factors influencing the treatment outcomes of implants in post-extraction sites. ITI Treatment Guide, Volume 3, Implant Placement in post-extraction sites: Quintessence Publishing, 2008.
- Dawson A, Martin W, Polido W. The SAC Classification in Implant Dentistry, 2nd edition: Quintessence Publishing, 2022.
- Chappuis V, Araujo MG, Buser D. Clinical relevance of dimensional bone and soft tissue alterations post-extraction in esthetic sites. Periodontol 2000 2017;73:73-83.
- Arcuri C, Barlattani A, Jr., Mazzetti V, Carosi P, Ferrigno N, Ferrigno N. Immediate restoration of a single upper central integrating digital workflow and a novel dental implant: a case report. J Biol Regul Homeost Agents Dental, Supplement 2019;33:171-177.
- Jensen OT, Ringeman JL, Adams MW, Gregory N. Reduced Arch Length as a Factor for 4-Implant Immediate Function in the Maxilla: A Technical Note and Report of 39 Patients Followed for 5 Years. J Oral Maxillofac Surg 2016;74:2379-2384.
- Derks J, Hakansson J, Wennstrom JL, Tomasi C, Larsson M, Berglundh T. Effectiveness of implant therapy analyzed in a Swedish population: early and late implant loss. Journal of dental research 2015;94:44S-51S.
- Zollner A, Ganeles J, Korostoff J, Guerra F, Krafft T, Bragger U. Immediate and early non-occlusal loading of Straumann implants with a chemically modified surface (SLActive) in the posterior mandible and maxilla: interim results from a prospective multicenter randomized-controlled study. Clin Oral Implants Res 2008;19:442-450.
- Nelson K, Stricker A, Raguse JD, Nahles S. Rehabilitation of irradiated patients with chemically modified and conventional SLA implants: a clinical clarification. J Oral Rehabil 2016;43:871-872.
