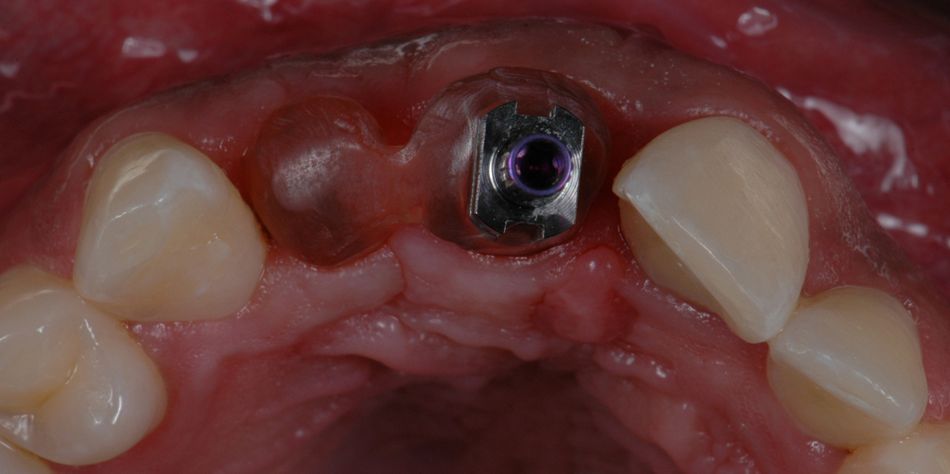
Initial situation
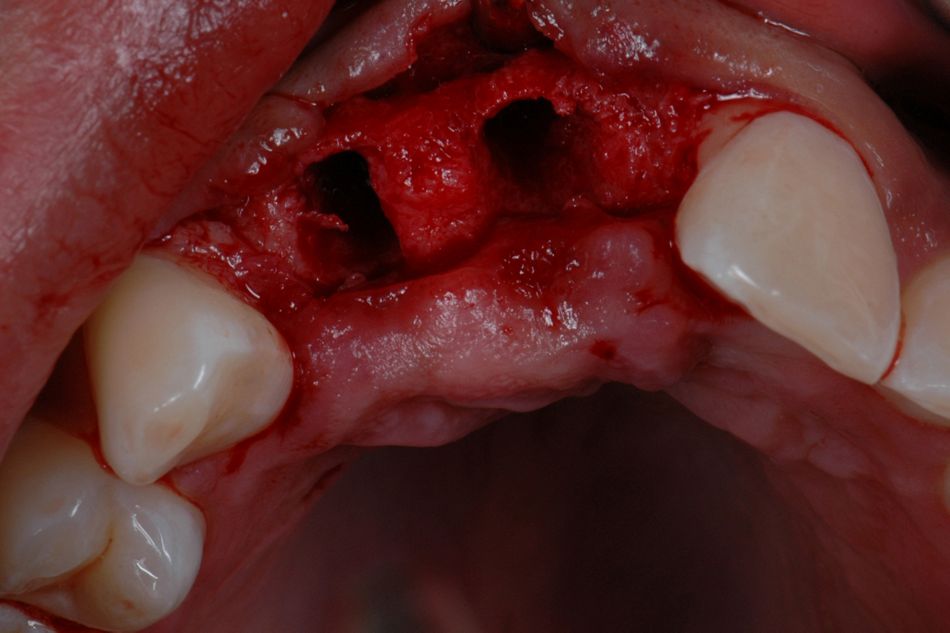
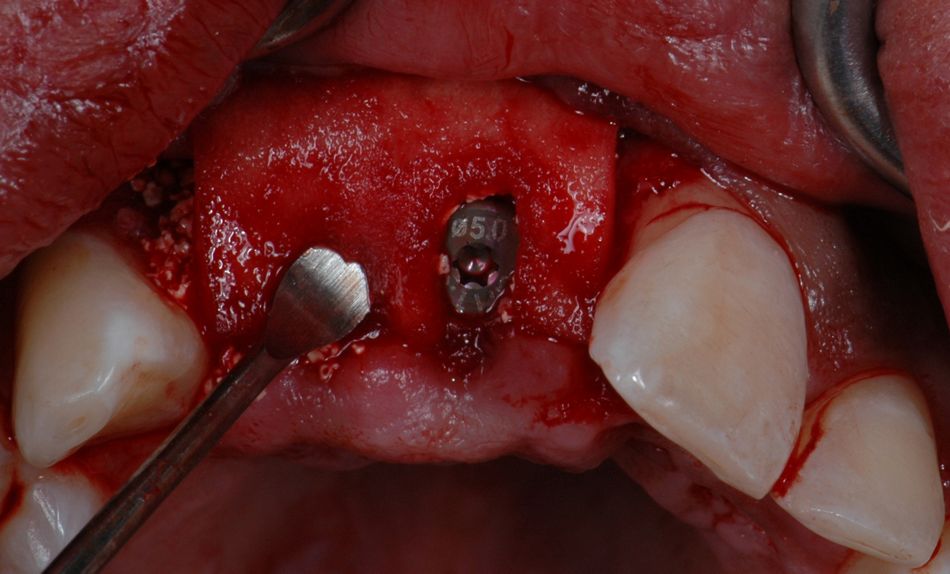
A healthy 27-year-old male suffered the avulsion of both central and lateral upper right incisors, during a street attack. At first, he attended to an emergency clinic in which the remaining teeth were splinted, and no effort was made to replace the avulsed teeth. (Fig. 1)
Treatment planning
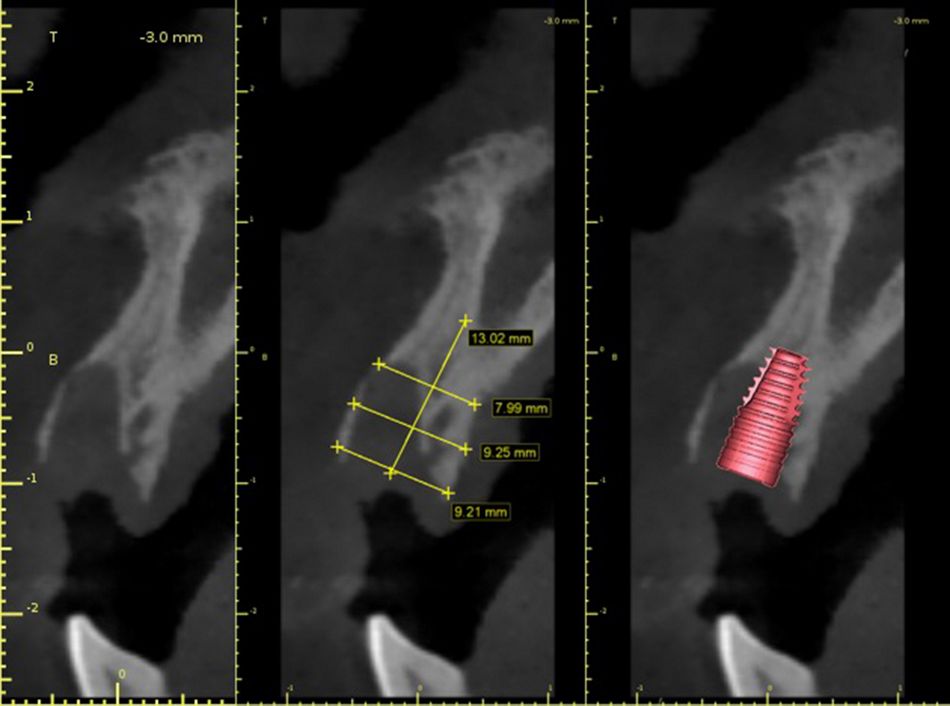
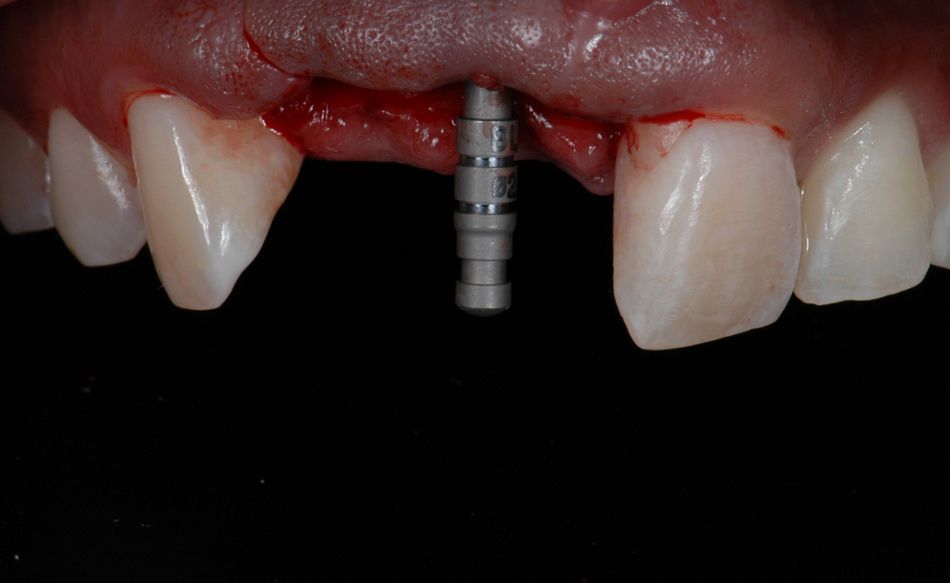
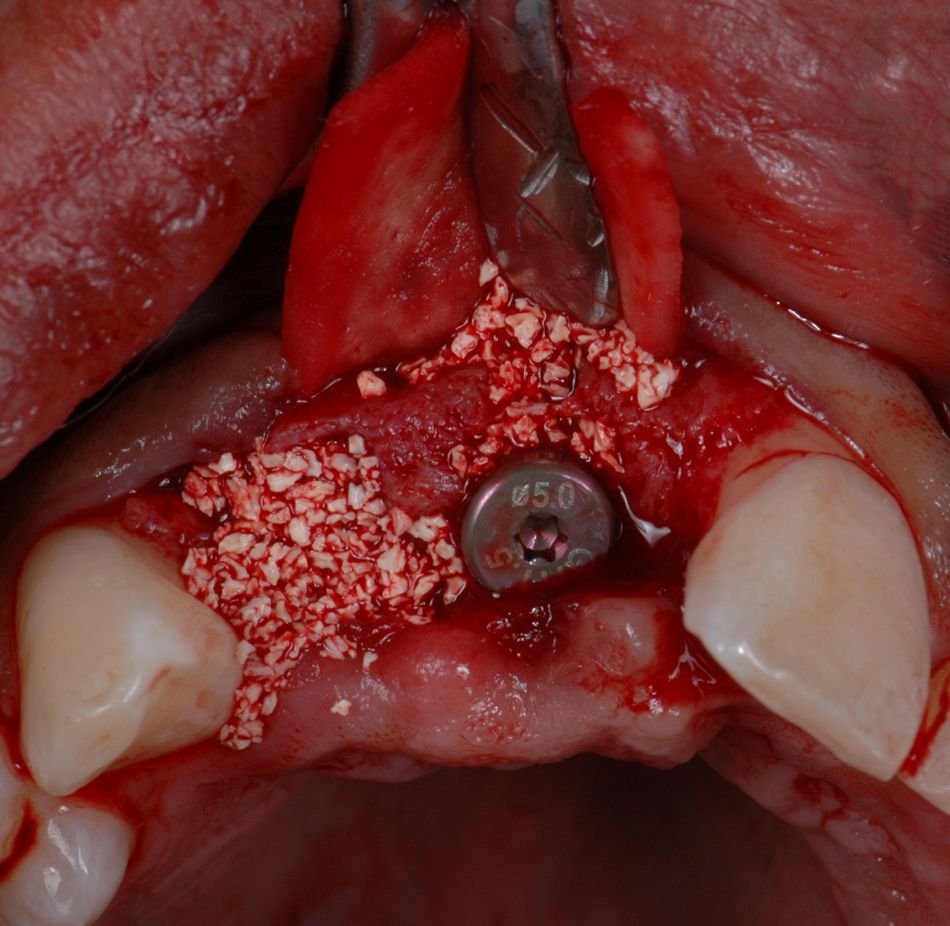
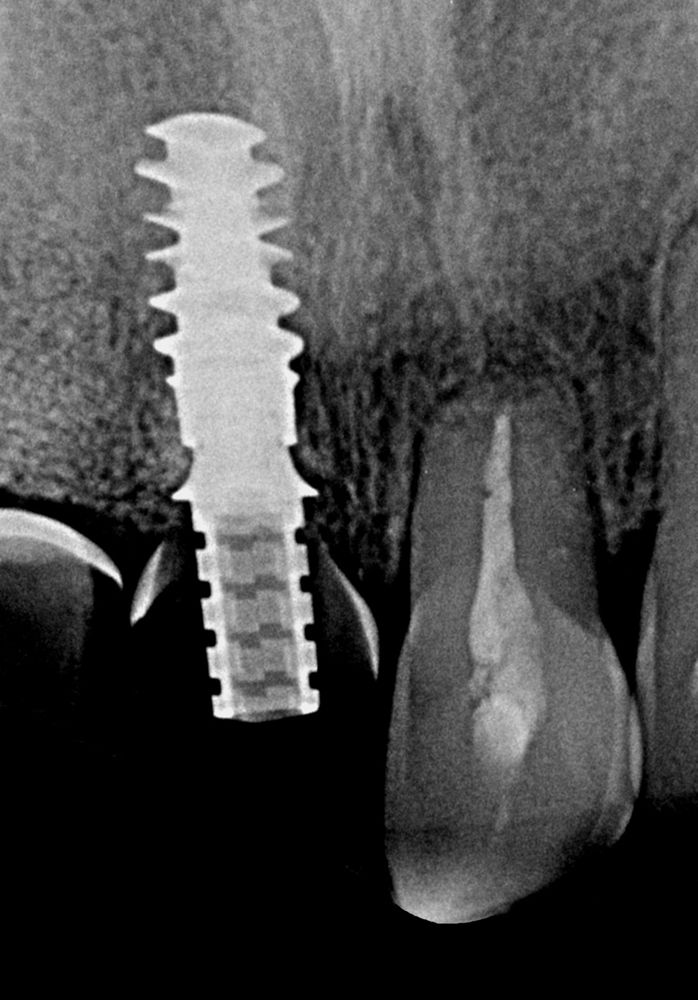
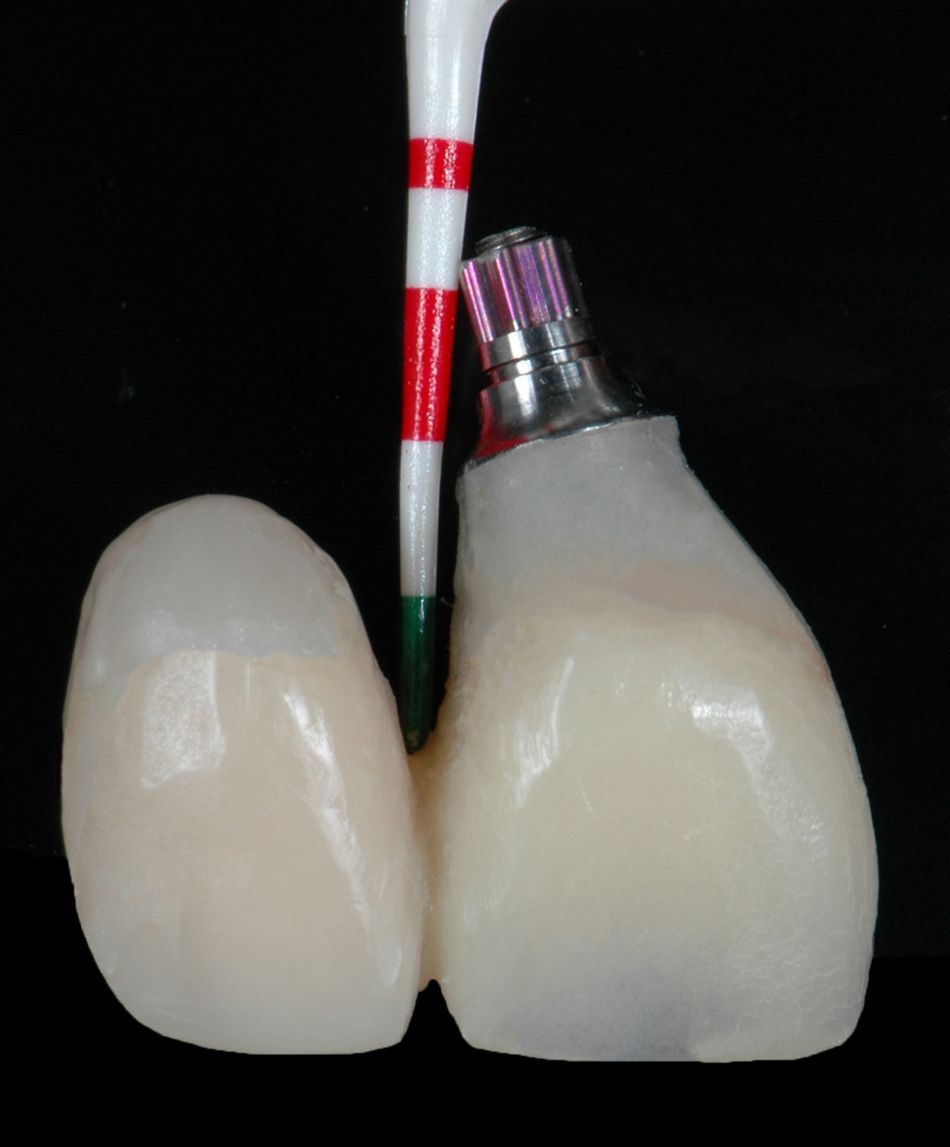
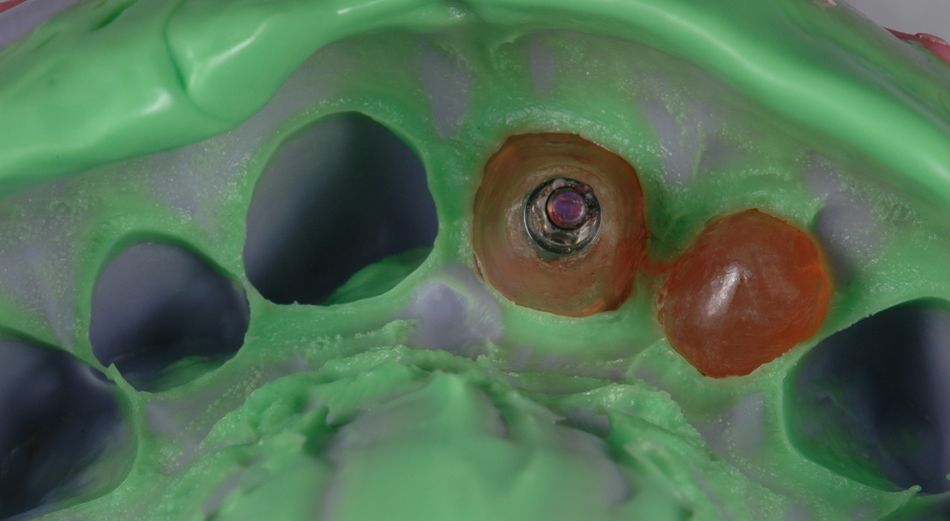
The clinical and radiological exams showed no signs of bone or adjacent teeth fracture. Nevertheless, we decided to take a CBCT for better planning of the case. In fact, bone plates were intact. Still, buccal bone plate showed thin and fragile. In cases like this, apical anchorage is the only way to increase primary stability. (Figs. 2-3) First approach was a removable partial denture made up with ovate pontics, as to preserve soft tissue shape. To increase primary stability, Straumann® BLX implant was the best option. With its unique functional design, it provides simplicity and immediacy. Progressive thread design compacts bone, increases its density and thus, increases strength. It cuts, collects, and condenses native bone, achieving almost perfect BIC (bone-to-implant contact).
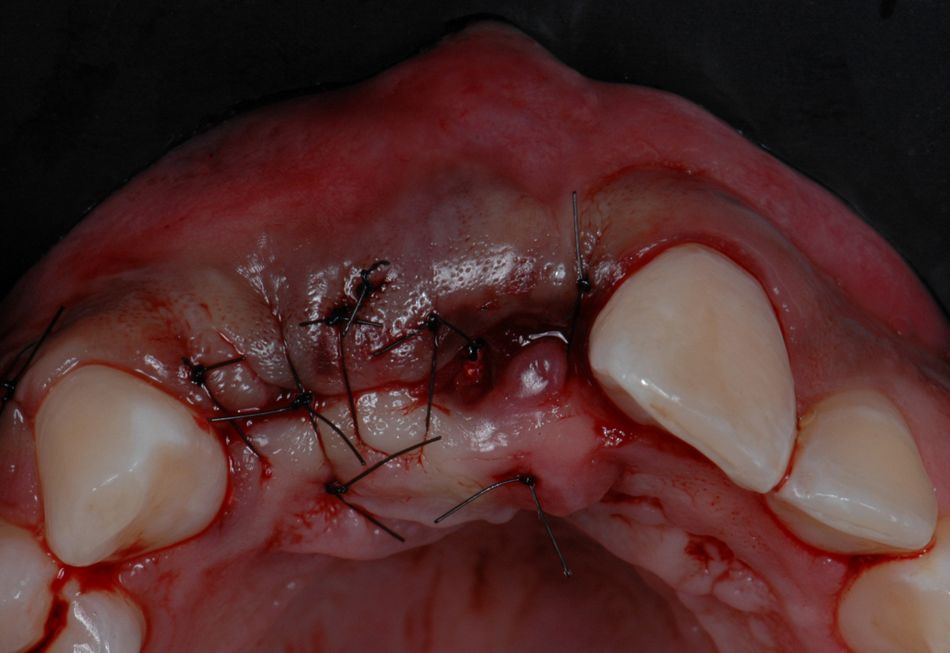
For better management of soft tissues, we decide a Type 2A, early placement and immediate restoration loading, 4 weeks after the incident.
Surgical procedure