The following case report describes the procedures of a complete smile makeover in a young lady with very high expectations. These included an immediate implant placement into a fresh extraction socket and immediate implant loading to replace a hopeless upper deciduous canine. Clinical cases like this one are also supported by Straumann® Smile in a Box™ - a flexible treatment planning and manufacturing service.
The Straumann® BLX implant made of Roxolid® and coated by a surface of SLActive® in combination with the digital workflow gave us precision and quality results; and allowed us to meet all the patient’s needs by applying an efficient treatment protocol for immediate implant placement and providing an esthetic provisional and final restoration design.
Initial situation
A healthy 30-year-old female patient presented at our dental clinic with the chief complaint of replacing the left upper deciduous canine with a conservative and predictable treatment approach. She also requested to have a temporary fixed rehabilitation during all the phases of the treatment and to improve the esthetics in the frontal area.
In the extraoral examination, the facial evaluation showed a symmetrical and proportional face. The analysis of the smile presented the midline sagittal plane coincident with the medium line of smile, and the exposure of the upper incisors and canines was 90% (Fig. 1). The smile also revealed that the lateral incisors were different in shape and the left upper deciduous canine was shorter, narrower and more yellowish in color in comparison to the contralateral permanent canine (Fig. 2-4).
In the intraoral examination, a good amount of keratinized gingiva was observed by the deciduous tooth and a good overall oral hygiene was presented (Fig. 5-7).
- Fig. 1: View of the patient before the treatment.
- Fig. 2: Frontal view of the patient’s smile.
- Fig. 3: Right lateral view of the patient’s smile.
- Fig. 4: Left lateral view of the patient’s smile.
- Fig. 5: Intraoral frontal view
- Fig. 6: Intraoral view: The discrepancy between upper canines and lateral incisors is clear. Note that the deciduous tooth is shorter than the contralateral, both at the occlusal and at the gingival side.
- Fig. 7: Magnification of the deciduous tooth: A wide amount of keratinized gingiva is shown.
The functional analysis revealed that the canine guidance was given by lateral incisor and first premolar whilst the deciduous canine was not involved (Fig. 8).
- Fig. 8: The functional analysis revealed that the canine guidance was given by lateral incisor and first premolar whilst the deciduous canine was not involved.
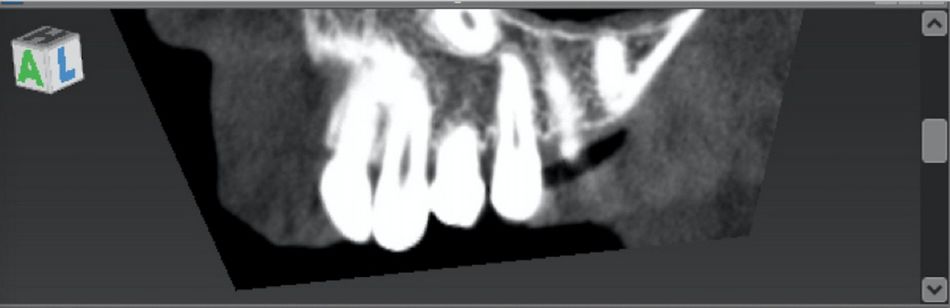
The radiographic evaluation with a Cone Beam Computed Tomography (CBCT) showed the extremely reduced root of the deciduous canine, the presence of an impacted left upper permanent canine and a thick cortical bone and adequate trabecular bone in the deciduous tooth site, as well as the feasibility of placing there an implant (Fig. 9-10).
- Fig. 9: Cone Beam Computed Tomography (CBCT) exam shows the presence of the impacted canine.
- Fig. 10: CBCT showed a thick cortical bone and adequate trabecular bone in the deciduous tooth site, as well as the feasibility of placing there an implant.
Treatment planning
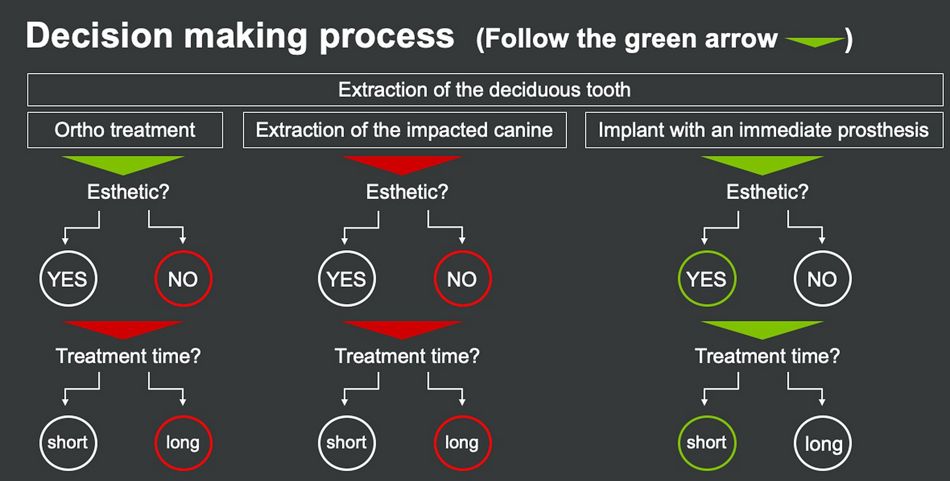
After a careful examination of the clinical and radiographic findings, we obtained the following treatment options:
a. Extraction of the deciduous tooth and orthodontic treatment for the repositioning of the impacted canine in the correct site and the re-alignment of the incisors to improve the smile appearance.
b. Extraction of the deciduous tooth and extraction of the impacted canine. After the healing, implant positioning and replacement of the canine with an implant-supported crown, and veneering of the right lateral incisor in order to improve the smile appearance.
c. Extraction of the deciduous tooth and positioning of an implant in the existing bone with immediate prosthesis with the aim of maintain a favorable esthetic appearance. After implant osseointegration, final implant-supported crown and veneering of the right lateral incisor.
We evaluated each of them considering the patient’s needs. As we were seeking for the most conservative and efficient approach, our preferable option was to place a post-extractive implant and provisional restoration in the site 23 leaving the permanent impacted canine in its position, as this allows a shorter treatment time and a better patient morbidity and esthetics (Fig. 11).
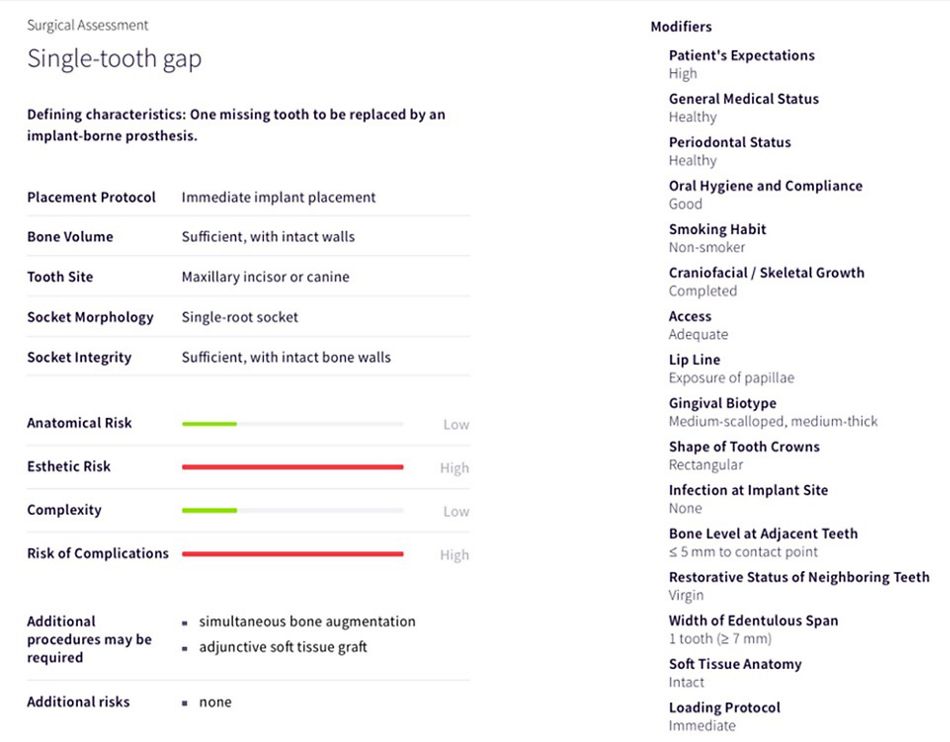
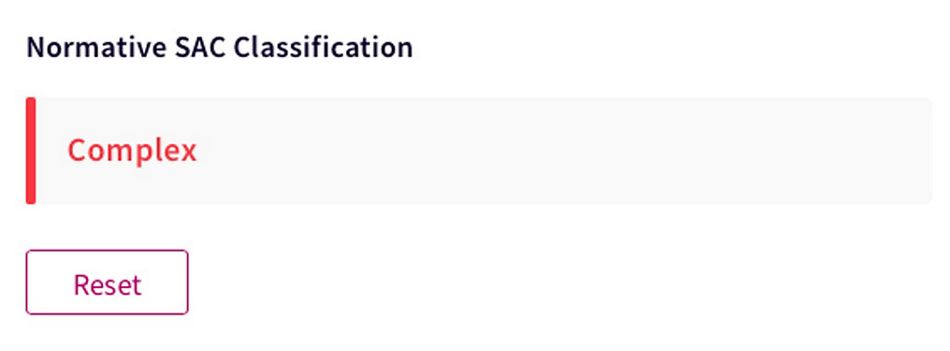
Within the treatment planning, it is also fundamental to identify and consider the degree of complexity and potential risk involved in the case. The SAC Assessment tool (based on ITI SAC Classification) can be successfully used for this matter. With the use of this assessment, the clinician can follow a step-by-step online procedure by introducing the data related to the patient (e.g. systemic conditions, local factors, etc.) and the loading protocol. Finally, a risk profile will be created according to the provided data. Within the SAC Classification, this specific case was considered as “complex” (Fig. 12-13).
- Fig. 12: Tool evaluation – SAC classification.
- Fig. 13: Following the SAC Classification, this specific case is considered as “complex”.
The final decision was to treat the patient with an immediate Straumann® BLX® ø4.5 mm SLActive® 8mm Roxolid® and an immediate prosthesis on position 23, using a computer-guided planning and surgery (coDiagnostiX®) with flapless technique. The rationale of our treatment plan relied on the following facts:
- The patient can be provided, as requested, with a non-invasive surgical approach allowing the presence of a fixed provisional crown along the whole therapy.
- The overall time of the treatment can be reduced.
- The use of a computer-guided approach will assure the precision needed in a case with such a limited vertical bone availability for the implant placement.
- The use of BLX® implant, thanks to its specific design and surface, will guarantee an optimal stability needed for the immediate implant placement and provisional prosthesis despite the reduced length of the implant site.
- The presence of a favorable site anatomy and a convenient amount of keratinized gingiva will reduce the risk of esthetic complications.
- The amount of keratinized gingiva will also allow to start the soft tissue conditioning around the canine at the time of the provisional crown placement.
Regarding the improvement of the smile and considering the patient’s request, the implant treatment of the left canine was planned to be followed by a modification of the shape of the right lateral incisor with a ceramic veneer.
As for this, the overall treatment workflow was divided in 8 phases:
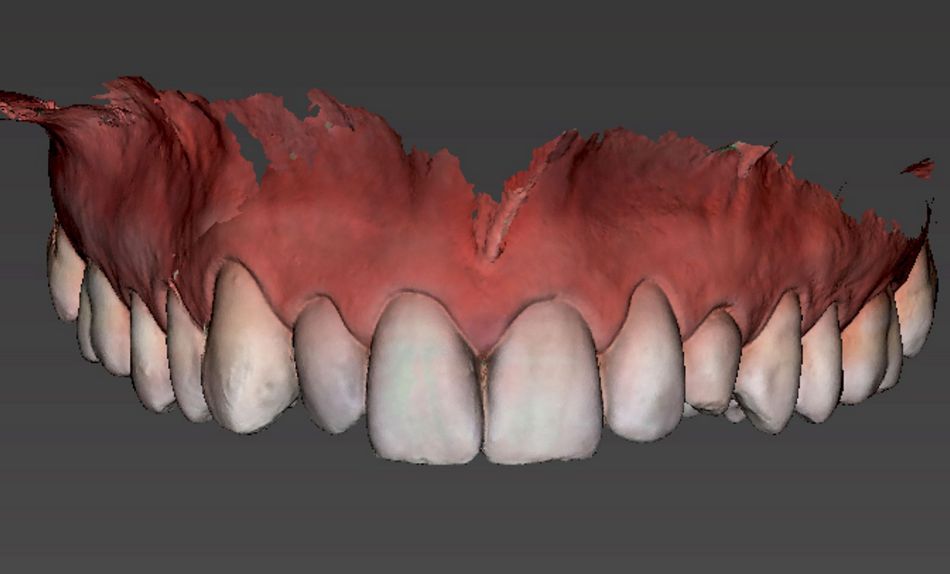
1. Preliminary data acquisition: intra and extra oral photos, digital impressions (DWOS Virtuo Vivo ™) and CBCT exam. (Fig. 14).
- Fig. 14: Digital impressions (DWOS Virtuo Vivo ™) are part of preliminary data acquisition along with intra and extra oral photos and CBCT exam
2. Esthetic analysis of the clinical case, pre-visualization of the final result by using a mock-up. The mock-up is based on the creation of digital wax-up related to tooth 23 ideal shape for the computer evaluation and to tooth 12 ideal shape for the final veneering. (Fig. 15-17).
- Fig. 15: Esthetic analysis.
- Fig. 16: Diagnostic wax-up
- Fig. 17: It is important to analyze the integration of new tooth shapes in the patient’s face. Comparing the image related to the initial situation with the planned one, it is clear that the smile has been evidently improved. Being the patient really satisfied, the wax-up related to this dental display will be used for the computer analysis.
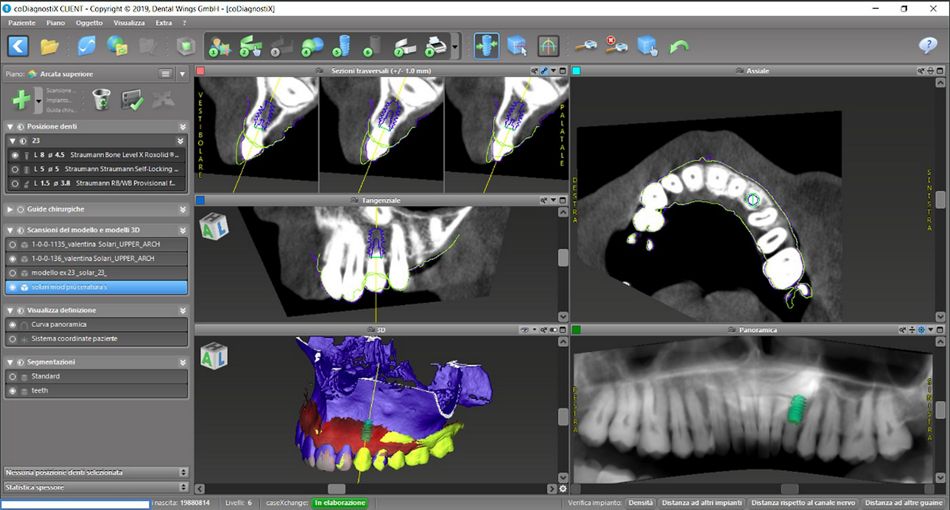
3. Processing of Dicom (CBCT exam) and STL (optical impression and digital wax-up) data in coDiagnostiX® planning software in order to carefully plan the implant placement and design surgical guide. (Fig. 18 -19).
- Fig.18: Planning the case step-by-step with coDiagnostiX®.
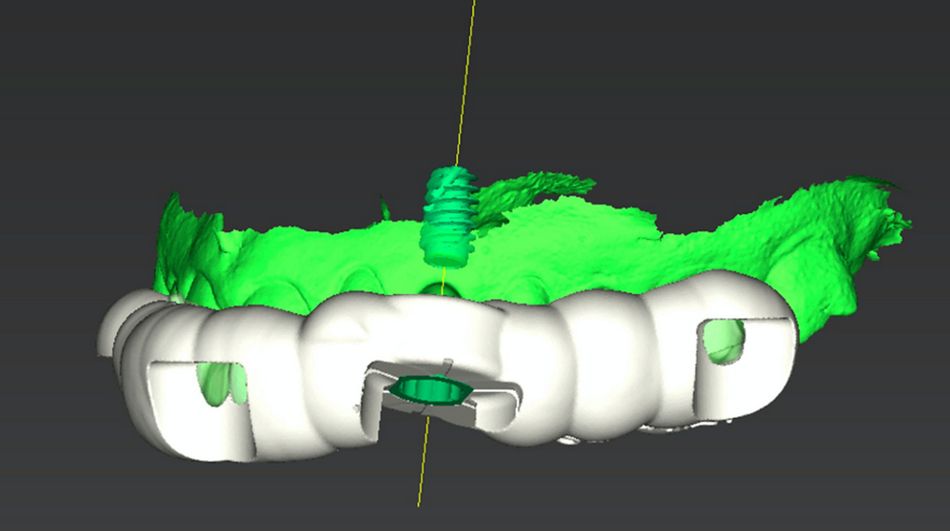
- Fig 19: Planning the surgical guide.
4. Production of printed surgical guide and resin models via coDiagnostiX® plan (Fig. 20-21).
- Fig. 20: In accordance with the STL file produced in coDiagnostiX®, the surgical guide was printed.
- Fig. 21: The guide seated on the printed model to verify the precision of the procedure.
5. Execution of the provisional crown by dental lab on the basis of digital wax-up (on resin printed models) (Fig. 22-24).
- Fig. 22: Lateral view of the printed model: Note that the shape of the provisional canine crown is now in line with the adjacent teeth.
- Fig. 23: Provisional crown.
- Fig. 24: The occlusal view shows the provisional abutment and the temporary crown adapted on top of it.
6. Guided implant placement with a flapless technique and provisional crown positioning.
7. After the healing, soft tissue conditioning with the provisional crown.
8. Final rehabilitation with screw-retained crown on BLX implant and ceramic veneering of tooth 12.
Surgical procedure
The patient underwent local anesthetic infiltration in the area corresponding to the canine apex (Fig. 25). The extraction of the deciduous tooth resulted in a simple procedure being the root almost completely reabsorbed (Fig. 26-28).
- Fig. 25: Anesthetic infiltration in the area corresponding to the canine apex.
- Fig. 26: Plier in position for the extraction procedure.
- Fig. 27: The extraction resulted in a simple procedure being the root of the tooth almost completely reabsorbed.
- Fig. 28: Occlusal view of the extraction socket.
After the extraction, the surgical guide was placed in the patient’s mouth as it is important to verify the stability and the precision of it through the windows created into specific locations (Fig. 29).
- Fig. 29: After the extraction, the guide was finally checked in the patient’s mouth: It is important to verify the stability and the precision through the windows created into the guide in specific positions of the teeth
Following guide placement and verification of the fit, the dedicated set of surgical instruments were ready to use (Fig. 30).
- Fig.30: Dedicated set of surgical instruments for the BLX implant guided surgery
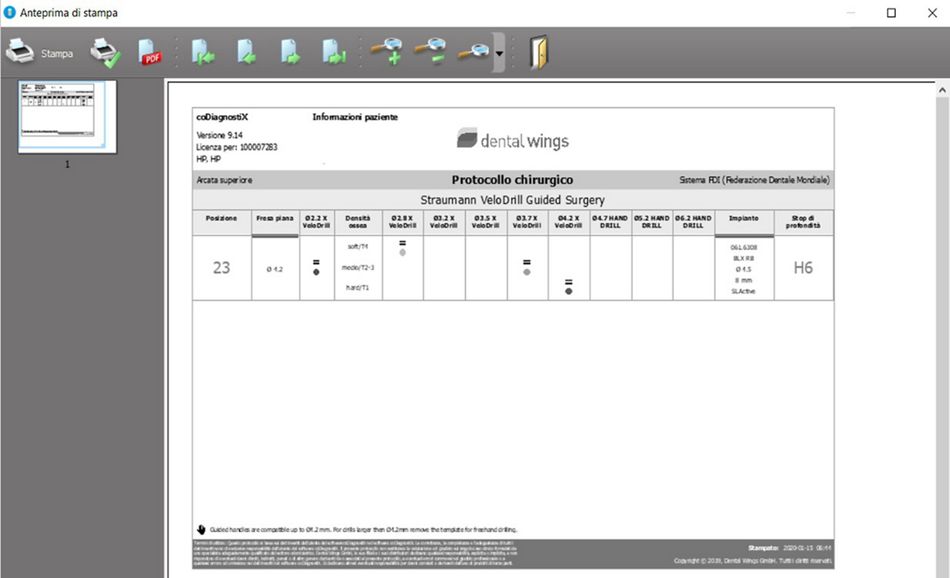
As described in the instructions for use, the drilling procedure was carried out until the stop, located on the drill itself. The protocol for this patient considered the placement of a Straumann® BLX® ø4.5mm and 8 mm length in a soft bone, and only 3 drills were required (Fig. 31).
- Fig. 31: Printing of the surgical protocol. This represents the plan to be used during implant placement. It drives the choice of the drills that must be strictly followed in order to perfectly stick to the implant planned positioning
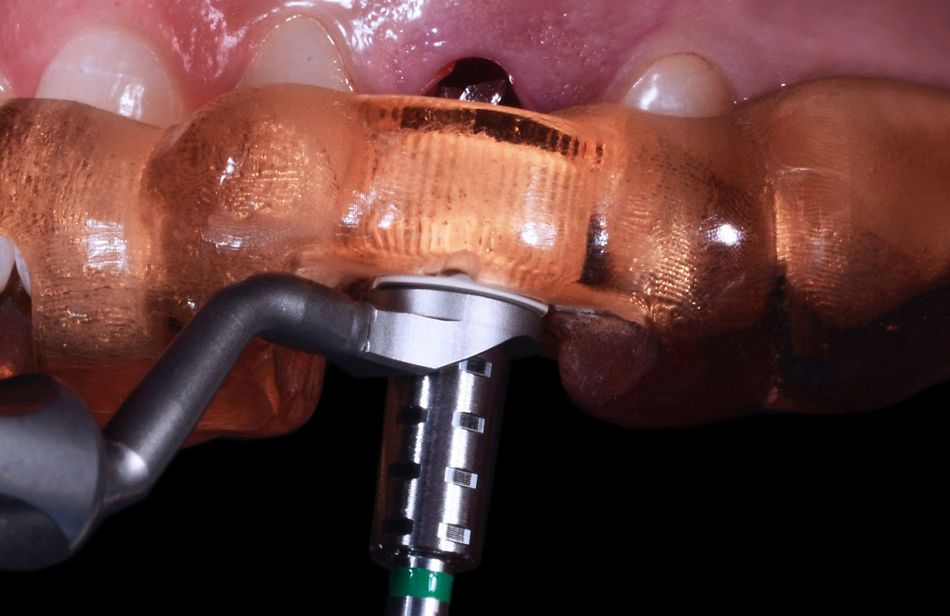
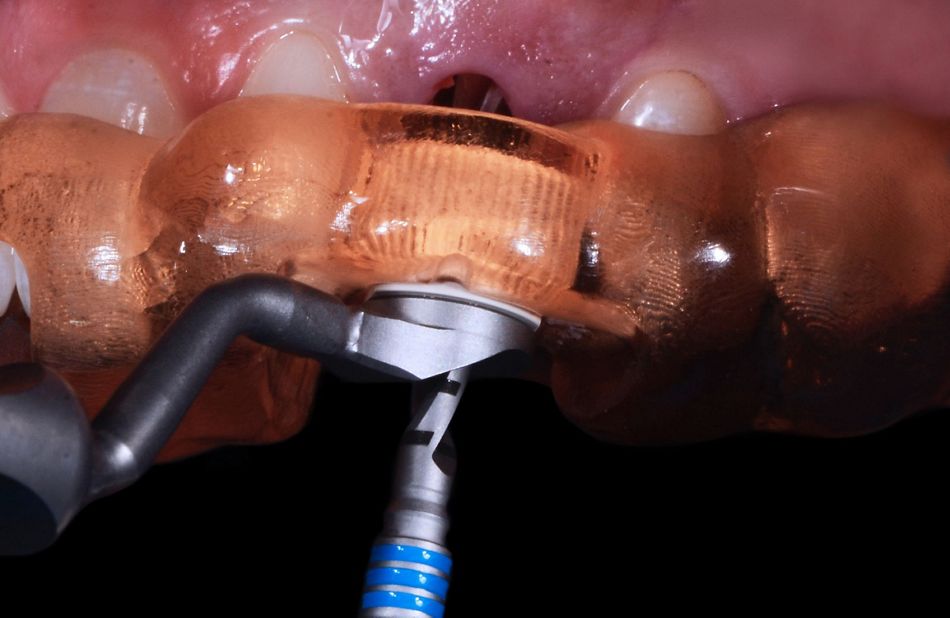
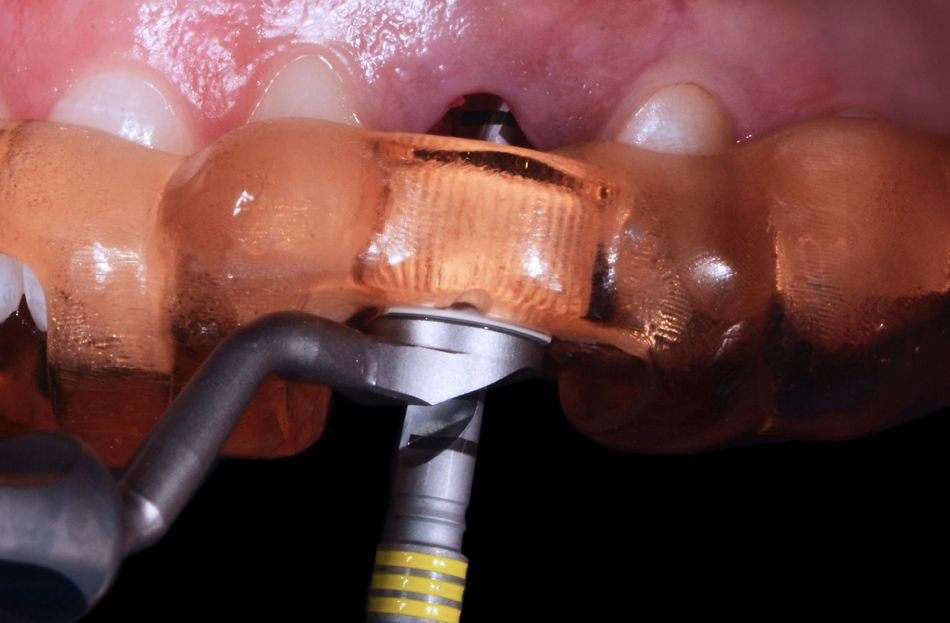
It started by using the milling cutter bur in order to create a flat surface for the precise work of the further drills (Fig.32), followed by the pilot drill (2.2mm diameter) (Fig. 33) and finally by the use of the 2.8mm drill (Fig. 34).
- Fig. 32: After the guide placement, the milling cutter bur was used with the purpose of creating a flat surface for the precise work of the further drills. The specific handle reduces the dimension of the sleeve to those of the selected drill.
- Fig. 33: Use of pilot drill (2.2 mm diameter)
- Fig. 34: Use of 2.8 mm drill
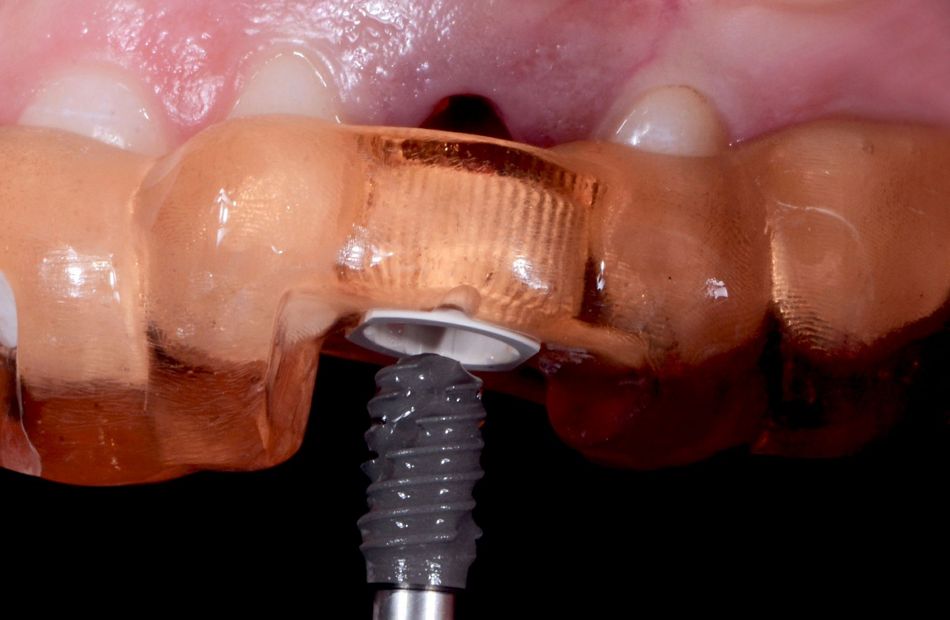
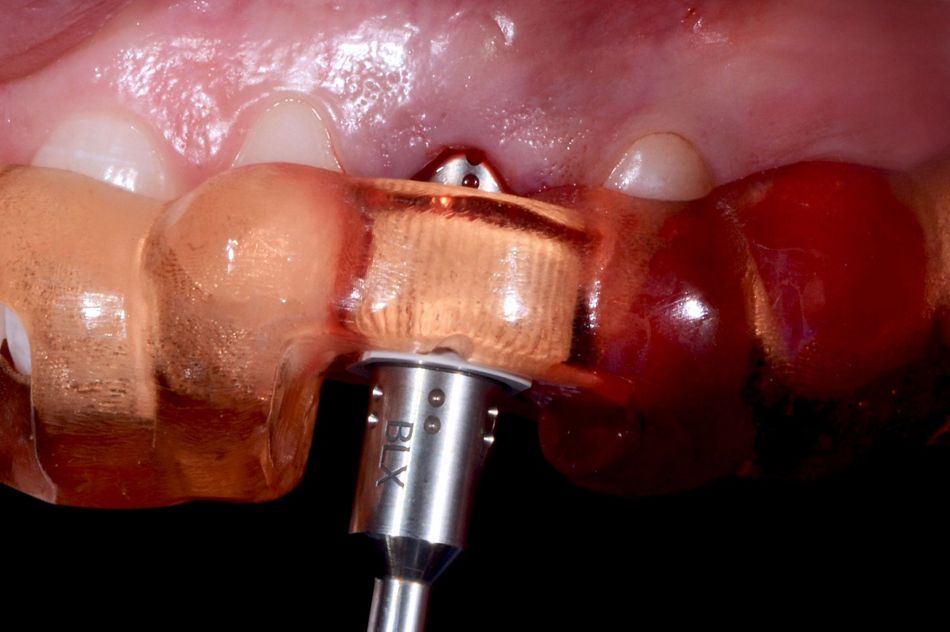
In accordance with the choice done during CoDiagnostiX® planning, a BLX® with 4.5mm diameter and 8mm length was selected and placed (Fig. 35 - 36).
- Fig. 35: In accordance with the choice done during coDiagnostiX® planning, a BLX with 4.5 mm diameter and 8 mm length was used.
- Fig. 36: A detail of the pickup of the implant: the pin placed in the apical part of the implant was gently broken.
The implant was engaged into the sleeve with the perfect guidance in the prepared bone site (Fig. 37) and the dedicated BLX® transfer piece drove the implant in the correct position (Fig. 38). The occlusal view after the implant placement and the removal of the guide showed an optimal 3D implant position (Fig. 39).
- Fig. 37: The implant ready to be engaged into the sleeve for the perfect guidance in the prepared bone site.
- Fig. 38: The dedicated BLX transfer piece drove the implant in the correct position.
- Fig. 39: Occlusal view after the implant placement and the removal of the guide.
Despite the reduced amount of available bone, it was possible to reach a 35n/cm torque value for the implant stability and this allowed the placement of an immediate prosthesis (Fig. 40). The customized provisional abutment with a diameter of 3,8mm and a gingival height of 1,5mm was screwed on top of the implant (Fig. 41). Afterwards, the chimney of the provisional abutment was protected with a cotton pellet to avoid during the further steps the occlusion of the access to the screw. Then, the temporary crown was placed into the transparent mask; and after having filled the crown with resin, it was brought in its position by means of the transparent mask for the connection with the provisional abutment. Following the resin polymerization, the temporary crown was unscrewed (Fig. 42) and the space between the crown and the abutment was filled with resin and then adapted until obtaining a proper emergency profile (Fig. 43).
- Fig. 40: Despite the reduced amount of available bone, it was possible to reach a 35 n/cm torque value for the implant stability. This allowed the placement of an immediate prosthesis.
- Fig. 41: The provisional abutment, shortened and sandblasted by dental lab, was screwed on top of the implant.
- Fig. 42: After resin polimerization, the temporary crown was unscrewed.
- Fig. 43: Image of the crown once screwed on the analog, vestibular side.
After the adjustments, the temporary crown was placed in the patient’s mouth (Fig. 44) and post-op X-rays images were taken in order to ensure the precision of the implant and the provisional restoration (Fig. 45).
- Fig. 44: After the refinements, occlusion was checked in the patient’s mouth.
- Fig. 45: Post-op X-ray images showing the precision of the placement.
Prosthetic procedure
At the 3- month follow-up visit, the patient presented with an outstanding healing of the soft tissues and referred having no complications within the previous months (Fig. 46).
- Fig. 46: Note the nice emerging profile of the temporary crown; ready for the final prosthetic phases.
The ideal emerging profile of the temporary crown was therefore ready for the final prosthetic phases involving the implant-supported crown of left canine and the ceramic veneer of right lateral incisor. For this, the tooth 12 was prepared using a silicon mask as a guide: first of all, the initial mock-up was recreated and then the silicon mask (made on top of it) was used to verify the thickness needed for the ceramic veneering (Fig. 47).
- Fig. 47: The lateral incisor was treated with veneer to improve esthetics and avoid ortho treatment. This was an alternative solution offered to patient. As a first step, the mock-up was made once again and a silicon mask, created on top of it and cut in the middle, was used as a guide during the preparation of the tooth. This allowed us to pre-visualize the final shape of the tooth and to then remove the correct amount of enamel and create the exact space for the ceramic veneer.
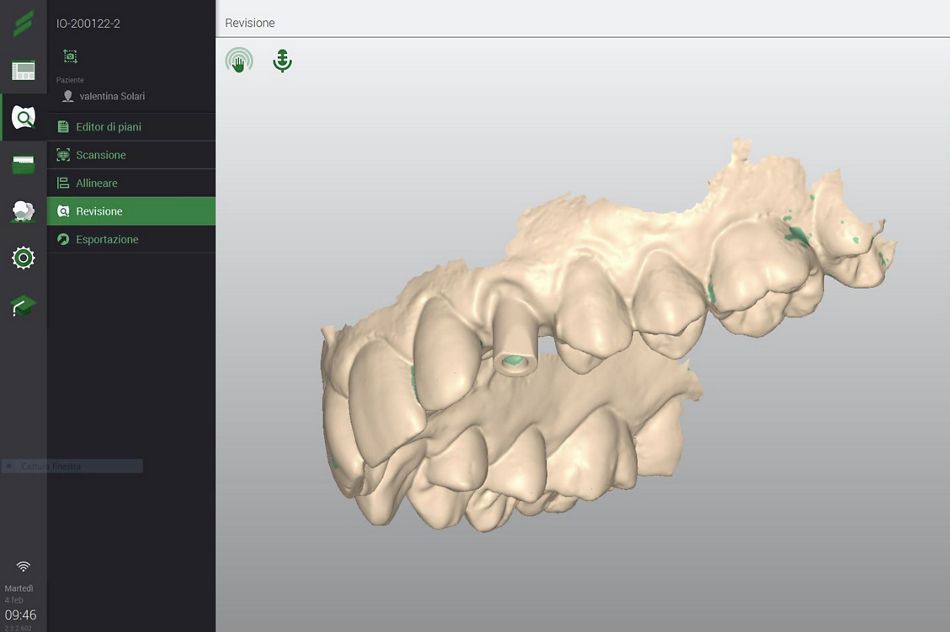
Afterwards, digital impressions using the Virtuo Vivo™ intraoral scanner were taken, and with this objective a dedicated scan body was screwed on top of BLX® implant and a retraction cord was placed around the tooth 12 in order to mark the line preparation (Fig. 48). Couple of minutes later, a digital impression of the area was obtained (Fig. 49).
- Fig. 48: Final digital impression: A dedicated scan body was screwed on top of BLX implant and a retraction cord was placed around the tooth 12 in order to highlight the finishing line preparation.
- Fig. 49: Final digital impression: a screenshot of the data acquisition with the intraoral scanner DWOS.
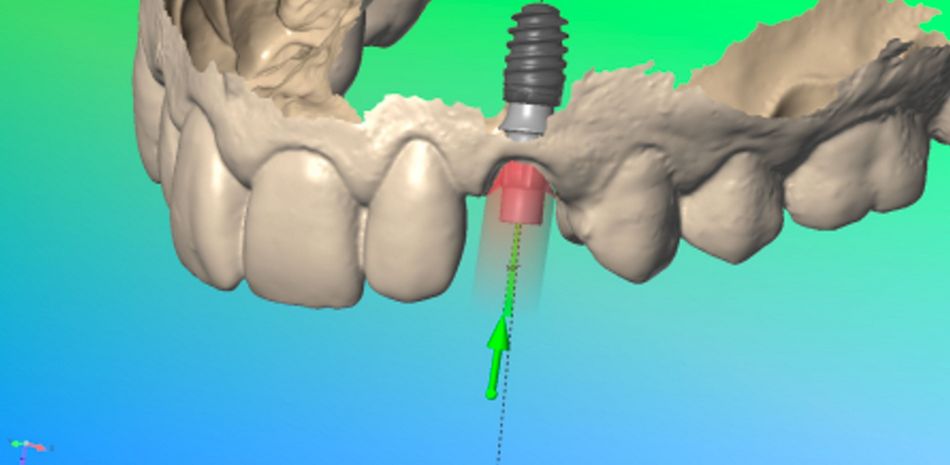
Then, the STL files related to the impressions were imported in the Dental Wings lab modeling software. The implant was virtually inserted into the model and the Variobase® RB with a diameter of 3,8mm and a gingival height of 1,5mm was placed on top of it (Fig. 50 a & b)
- Fig. 50a and b: the STL files related to optical impression were imported in Dental Wings lab modeling software. The implant was virtually inserted into the model and the Variobase® was seated on top of it.
- Fig. 50a and b: the STL files related to optical impression were imported in Dental Wings lab modeling software. The implant was virtually inserted into the model and the Variobase® was seated on top of it.
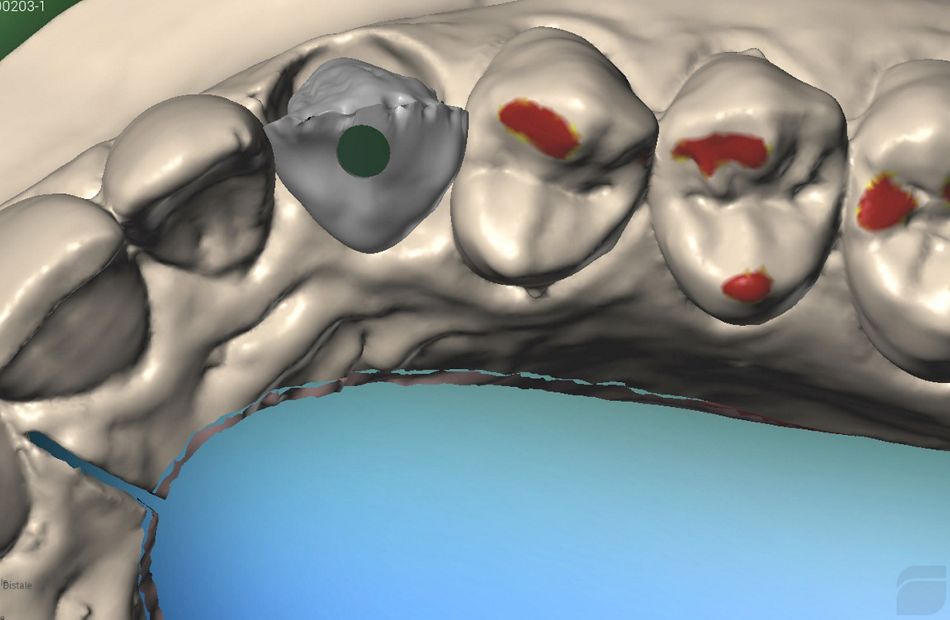
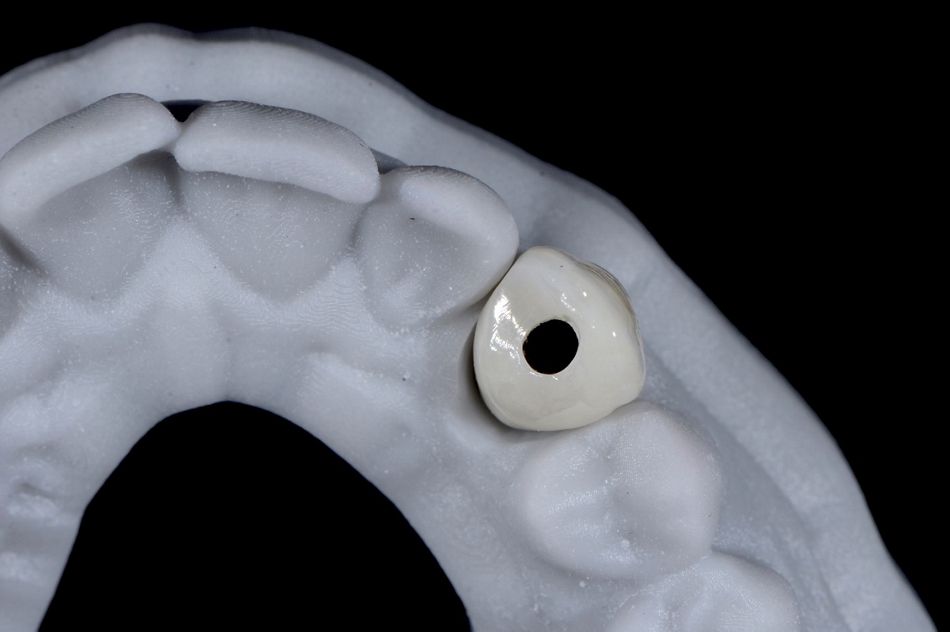
Then, the modeling of the zirconia crown to be veneered after milling on the vestibular side with ceramic was performed. Once this step was completed, the zirconia crown was produced using this as a reference (Fig. 51). Following the milling of the zirconia crown and the ceramic veenering, the crown was cemented on the Variobase® using a composite cement (Fig. 52). Afterwards, the final crown was carefully polished and adjusted for the placement in the patient’s mouth (Fig. 53-54).
- Fig. 51: Modeling of the zirconia crown to be veneered after milling on the vestibular side with ceramic. Once this procedure is completed, the zirconia crown will be produced on the basis of this project.
- Fig. 52: After the milling of the zirconia crown and its ceramic veneering, the crown was fixed on the Variobase® by using composite cement.
- Fig. 53: Vestibular view of the final crown.
- Fig. 54: Palatal view of the final crown.
Meanwhile the ceramic veneer for tooth 12 was also prepared and ready to be cemented. Both final restorations were received in a printed resin model, that allowed us to visualize the final result (Fig. 55-56).
- Fig. 55: Printed resin model with ceramic veneer and crown in position.
- Fig. 56: Occlusal view of the crown on the model: note the exact positioning of the screw hole due to the precise implant placement with computer-guided surgery.
For the cementation of ceramic veeners, it is fundamental to have an absolutely dry area. Therefore, all the anterior zone was isolated with a dental dam and the finishing line of the preparation was identified (Fig. 57-58).
- Fig. 57: Isolation of the operating field with dental dam for the cementation of the ceramic veneer: for the long-term success of the procedure it is fundamental to have an absolutely dry area.
- Fig. 58: A detail illustrating the finishing line of the preparation: It was perfectly visible and ideal for a correct cementation procedure.
Afterwards, the tooth was conditioned protecting the adjacent teeth and the ceramic veener was cemented using a flowable composite (Fig. 59-60).
- Fig. 59: Acid-etching of enamel: Note how the adjacent teeth were protected from the injury of the acid.
- Fig. 60: Cementation of the ceramic veneer with flowable composite.
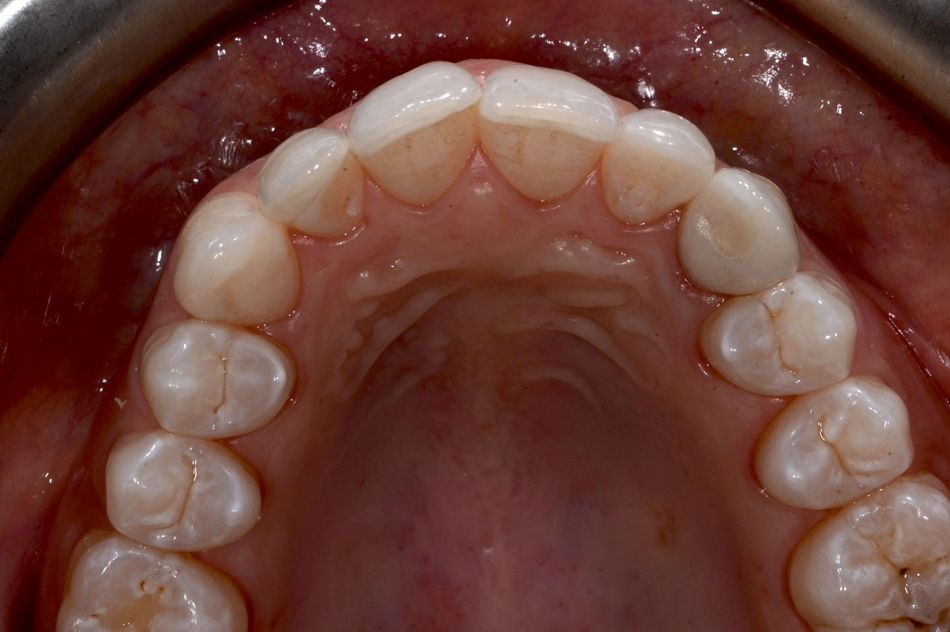
Finally, the screw head was protected by using a teflon floss and then the screw channel was filled with composite (Fig. 61-62).
- Fig. 61: After the tightening of the crown at 25 n/cm, the screw head was protected by using a teflon floss and the screw channel was filled with composite.
- Fig. 62: Final occlusal view.
Treatment outcomes
The patient and our team were extremely satisfied with the final outcome in terms of health, esthetics and function. Even when analyzing in detail, the final restoration could be hardly identified (Fig. 63).
- Fig. 63: Frontal view of the final result.
At this point we could say that we cover all our patient’s needs and expectations and we can appreciate a big improvement in comparison to the baseline situation (Fig. 64).
- Fig. 64: Before and after the treatment: Note how the smile of the patient was improved simply by modifying the shapes of 12 and 23
The new smile was harmoniously integrated in the patient’s face (Fig. 65-66) and finally, she was involved in a maintenance program for follow-up visits once per year.
- Fig. 65: The pleasant smile of the patient
- Fig. 66: New smile is harmoniously integrated in the patient’s face
Acknowledgments
Alessandro Giacometti, dental technician