The immediate implant placement and loading of a prosthesis in an edentulous jaw is an accepted treatment modality in dental practices worldwide. Optimization of treatment time is an attractive option for both the treating implantologist and the patient; thus, a single-stage surgical procedure and new loading protocols have been explored. The implant’s implant design, core material, and surface modification are important device related factors that may influence primary stability. All of these factors, as well as patient anatomy and bone quality, are prerequisites for immediate loading treatments. Scanning and milling techniques have opened up a new landscape for implant dentistry, enabling implant prosthetic dentistry to take a major step forward. Digital workflows are increasingly used, particularly for single-unit restorations, and they allow for straightforward and cost effective protocols that improve patient satisfaction. One-Tooth One-Time (1T1T) is a technique developed to predictably place implants in the molar area of the mandible, followed by immediate loading of a definitive prosthesis just hours after surgery using the new Straumann® BLX system and a digital workflow.
Initial situation
Patient presented to the office with a missing lower first molar. (Figs. 1-4) His chief complaint was that even if the tooth does not have an impact on aesthetics, he was feeling pain while eating on the respective side because of the pressure onto the gums. (Fig. 5) For this reason he realized he started to shift all his chewing activity to the opposite side and now his wish is to have the site restored as soon as possible.
Considering the patient presents a well balanced occlusion and the missing tooth was the only tooth missing, it was discussed the One-Tooth One-Time technique with the patient which would fulfill his primary wish.
Treatment planning
A CBCT scan was taken pre-operatively confirming 13 mm of vertical bone between the inferior alveolar nerve and the coronal cortical margin of the mandible, as well as a minimum bone width of 6 mm. The implant selected for the surgical procedure was a Straumann BLX® with ø5.5x10mm followed by Intra Oral scanning plus the manufacturing of hybrid ceramic crown onto a WB Variobase® abutment and torqued to 35Ncm.
Surgical procedure
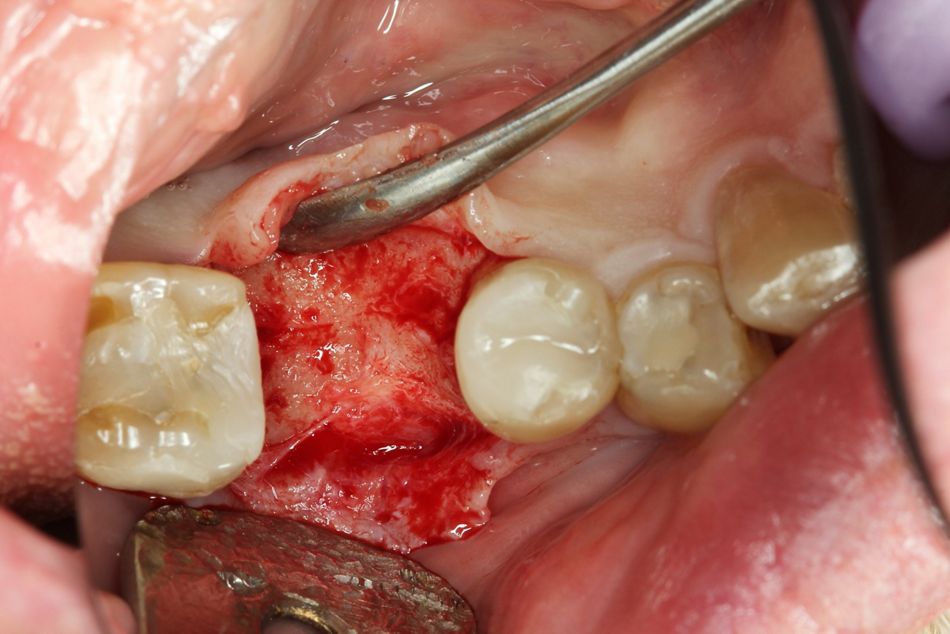
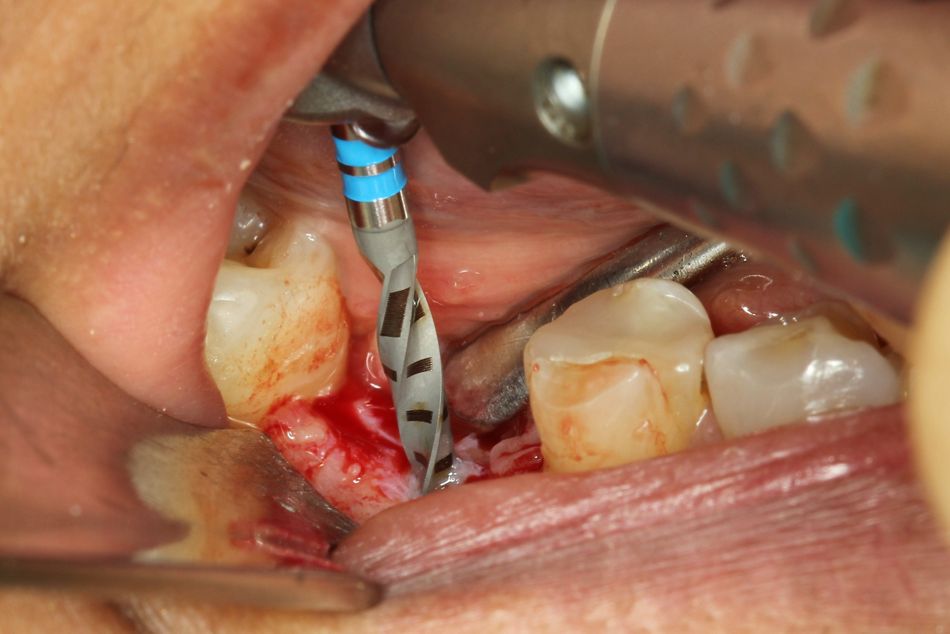
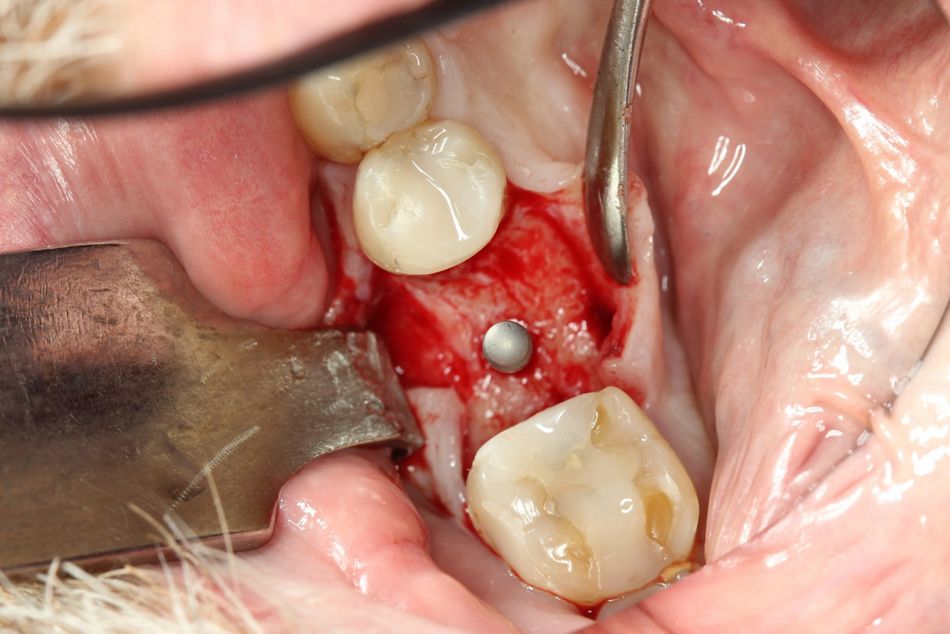
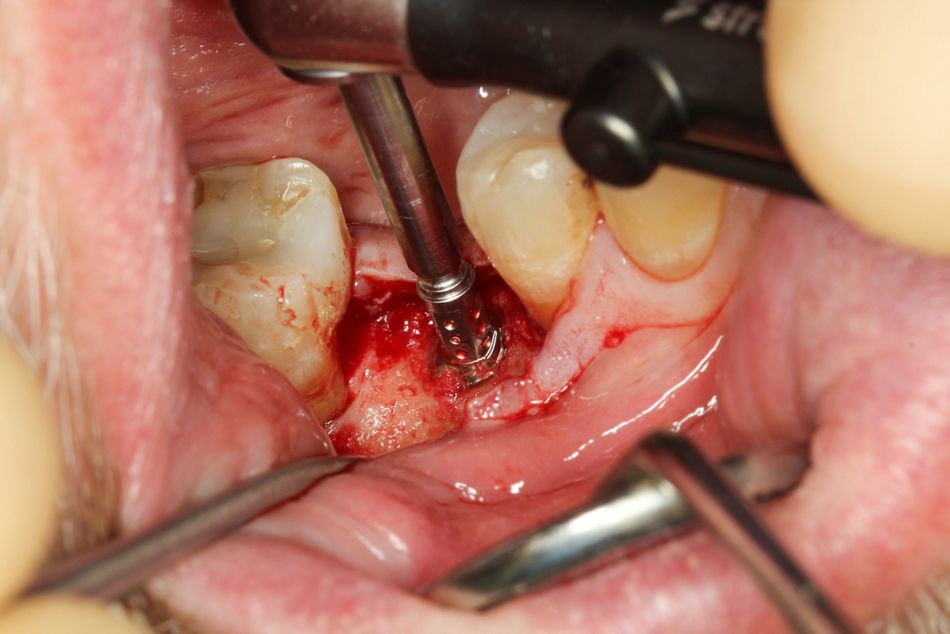
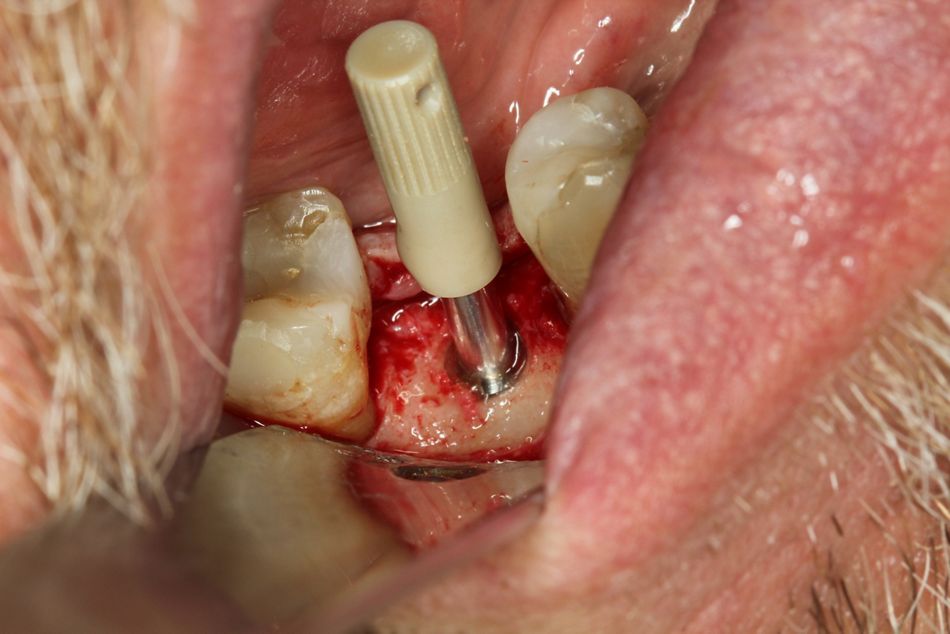
A flap was raised to expose the alveolar bone in the surgical area (Figs. 6-7). The ideal position for the implant was selected with careful determination of the best 3D position via clinical assessment. A pilot hole (2 mm) was drilled to determine the bone density (Fig. 8). The alignment pin was placed to confirm the ideal 3D position and the preparation depth (Figs. 9-10). The width of the osteotomy was defined by clinical evaluation of bone density and following the recommended drilling protocol. (Figs. 11-13).
A 5.5mm x 10mm BLX implant is placed with the use of the ratchet and the Straumann® Surgical Torque Control device. (Figs. 14-15). Because of the very engaging design the implant reached the torque value of 55Ncm. (Fig. 16)
A 5.5mm x 10mm BLX implant is placed with the use of the ratchet and the Straumann® Surgical Torque Control device. (Figs. 14-15). Because of the very engaging design the implant reached the torque value of 55Ncm. (Fig. 16)
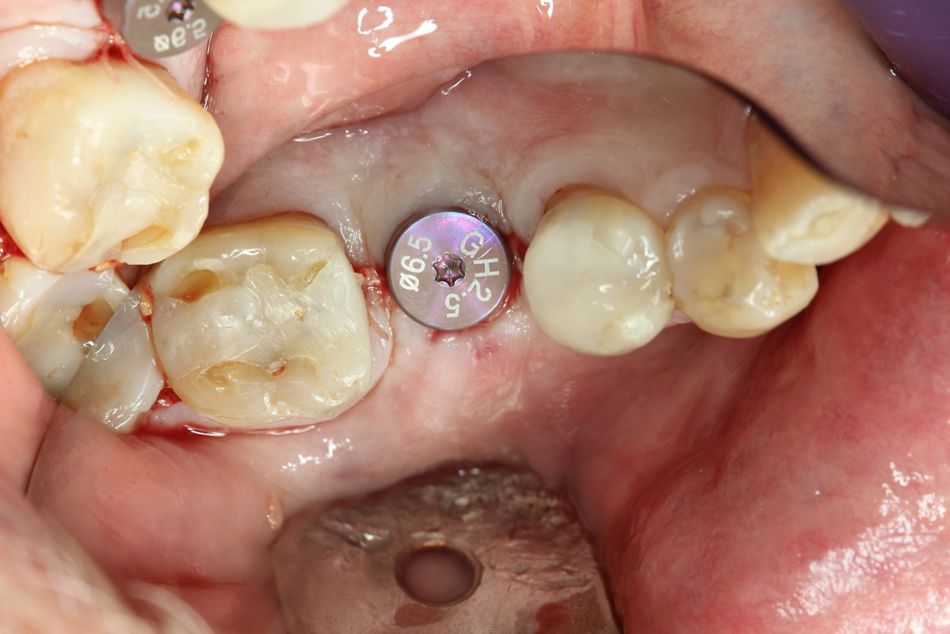
The primary stability was further evaluated using the Implant Stability Quotient (ISQ) level (Osstell; Integration Diagnostics, Gothenburg, Sweden). (Figs. 17-18) A minimum measurement of ISQ necessary for the implant to be sufficiently stable for immediate definitive loading is 60. The BLX WB healing abutment, with a diameter of 6.5 mm, was placed, and the initial neck height of 2.5 mm, was selected determined by the coronal bone anatomy . A-PRF membranes were placed on the buccal surface of all implants to aid soft tissue healing (Fig. 19). Sutures were placed to create a soft tissue seal around the implant (Fig. 20-21). The patient was then transferred to the prosthodontist office.
Prosthetic procedure
The prosthodontic and technical work followed a digital workflow that included a DW intraoral scanner and CAD/CAM processing using Straumann CARES® Digital Solutions.
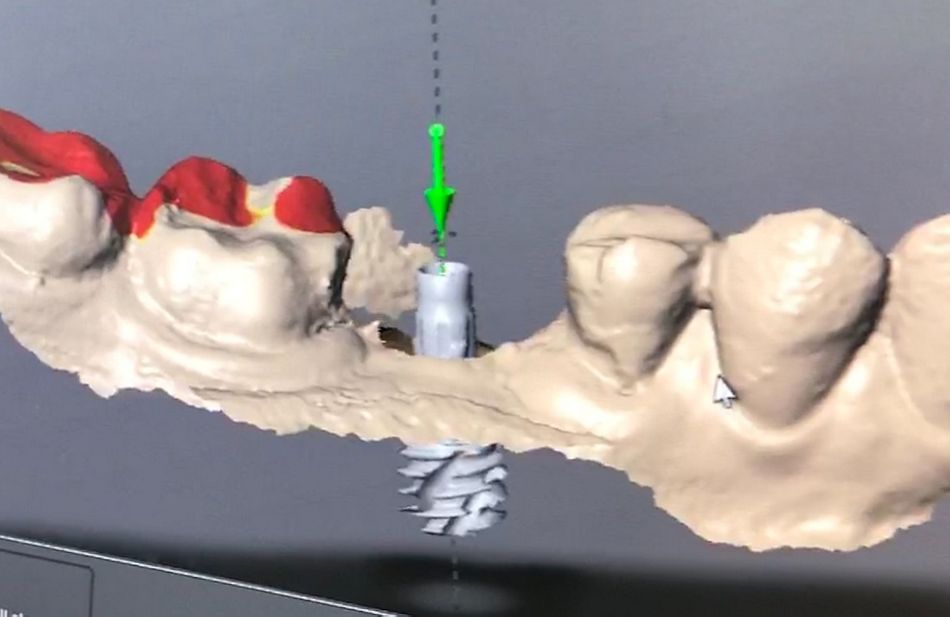
The Intra Oral Scanner captured the peri-implant mucosal architecture, including the neighboring teeth, in a quadrant-like approach. Then, a monotype scan body was screwed into the implant (Fig.22), and the 3D implant position was determined. The corresponding opposite arch was scanned in the same way. Finally, the bite recording was also digitally transferred.
Based on the .STL file from the IOS, a full-contoured crown was designed as a screw-retained dental hybrid ceramic (Vita Enamic IS-16L, Vita Zahnfabrik, Bad Säckingen, Germany) (Fig.23) and bonded with composite luting cement to a RB/WB Variobase® and produced digitally without any physical models or casting. The virtual crown design was processed and produced with 4-axis wet milling and grinding equipment (CARES C-Series, Institute Straumann AG, Basel, Switzerland). After the crown was milled, the restoration was cleaned with 95% ethanol and, after further post-processing, polished and individually characterized. Then, the prepared crown was directly bonded to a WB Variobase® extra-orally.
First the interproximal fit, and then the marginal integrity of the restoration, were clinically assessed. Identical continuity with dental floss was separately checked for the mesial and distal contact surfaces. Next, the occlusal scheme was checked statically and dynamically with Shimstock foil, achieving light occlusal contacts.
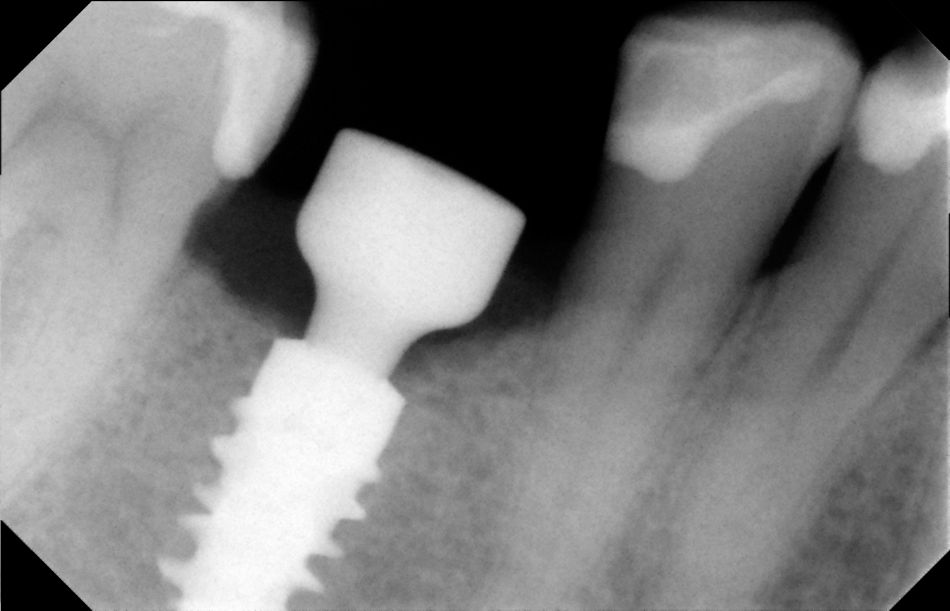
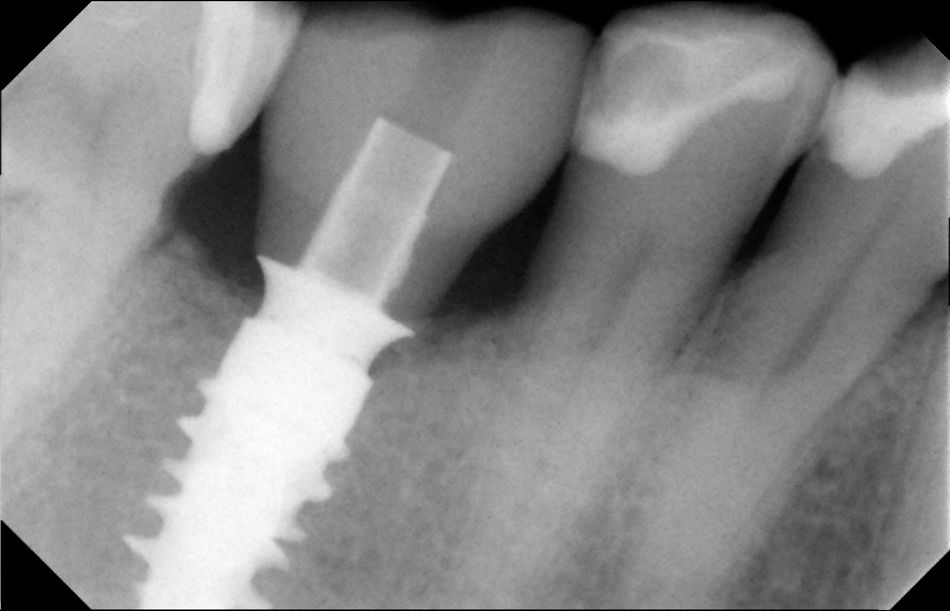
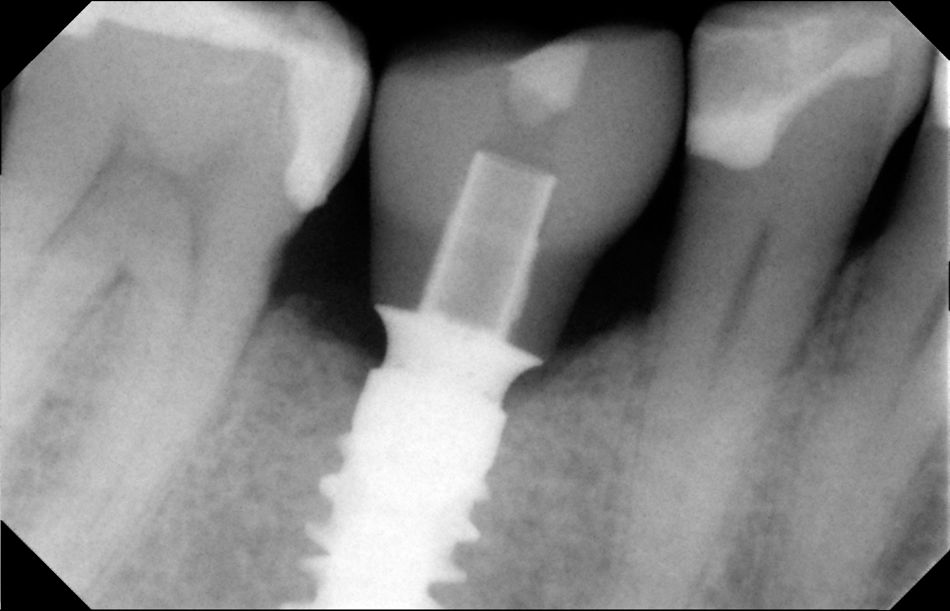
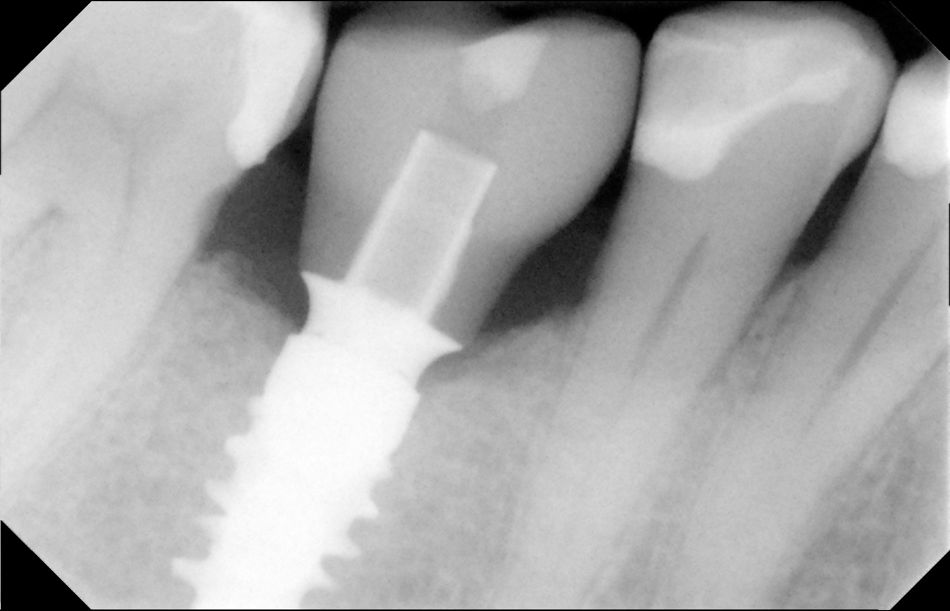
The restoration was screwed with a torque of 35 Ncm, according to the implant provider’s recommendations. The screw access hole was sealed with Teflon tape and composite material (Figs.24-25). PeriaFig.al radiograph was used to check the position of the implants after the procedure (Fig.27). Follow up X-rays was taken at the day of suture removal (15 days) (Fig.27), in 3 months (Fig.28) and 6 months (Fig.29)
Treatment outcome
To perform 1-Tooth 1-Time technique patient selection is key, with only one missing posterior tooth required to be restored in well balanced occlusion relation. It is critical to select an implant design that will ensure primary stability and enhanced bone-to-implant contact. Fully tapered implants favour this outcome.
The Straumann® BLX implant is designed for increased primary stability to enable immediate treatment protocols. The first requirement is that the implant should achieve primary stability, and thereafter a crown can be manufactured with full digital flow. This has the added advantage of no impression material ever coming into contact with the surgical wounds.
Digital implant dentistry will soon have an enormous impact on daily dental practice because of its precision in replicating the structures in the mouth. Analogue methods using traditional impressions often encounter inaccuracies. This new standard, as with all newly acquired knowledge, requires experience and familiarity with the products used. While some adjustments to the occlusal and interproximal contacts were needed, this need is way less than in analogue way. Digital protocols lead to more predictable results and a more efficient workflow, which will help control costs and save time for both the patient and the dental team.
Conclusion
The 1T1T technique presented showed a missing lower first molar treated with implant and restored with the definitive crown a few hours after the surgical procedure. This treatment modality has been shown to be a reproducible and predictable treatment option through the combination of the Straumann® BLX implant system and its respective digital workflow.