To rehabilitate both jaws of a patient with a poor oral situation is already a challenge in itself. But we even wanted to try immediate loading with the help of BLX implants, which are excellent for this kind of work because of their macro geometry.
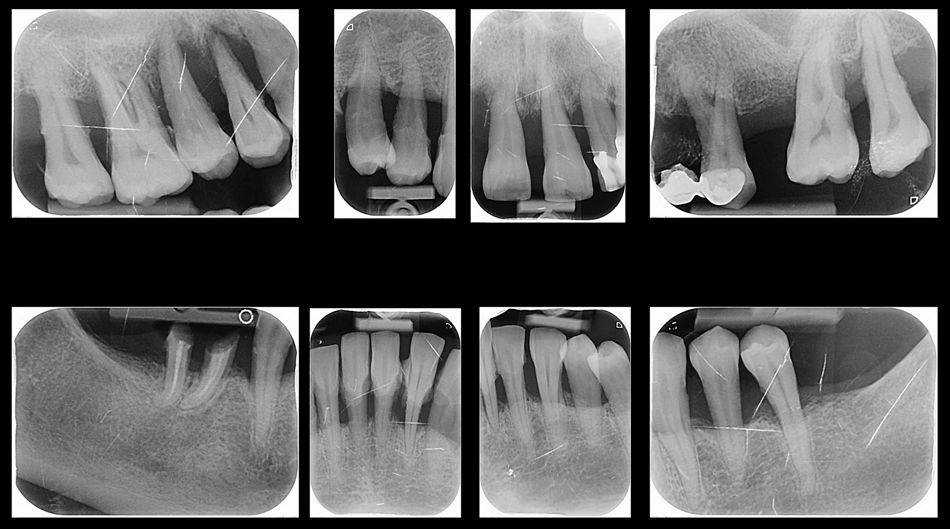
Initial situation
In April 2017 a 52-year-old woman presented at our dental clinic on her first visit. She exhibited really poor oral hygiene, and had not visited a dentist for six years (Figs. 1,2).
Her medical history was extensive: she had suffered from depression and been hospitalized for about a year. Hence her desire to fix her teeth permanently so that she could smile again.
It is our practice not to propose any implants until we see that the patient is able to improve their oral hygiene, so we began motivational training to achieve this goal.
Treatment planning
The first task we set ourselves was to restore and eliminate all active bacterial outbreaks and remove the periodontal teeth. Over the years, several authors have investigated the long-term maintenance of implants in relation to proper oral hygiene1, and they all agree that there is a high risk of implant loss in the absence of good hygiene. We therefore made sure that she was followed up and motivated by our dental hygienist.
We then wanted to see if the patient would have been satisfied with a complete denture, and had that been the case we would have considered placing four implants with a removable prosthesis with button attachments, but given her desire for a fixed solution we opted for this solution instead.
In this case, we chose to include the use of PRF membranes because, in our clinical experience, we have noticed that this promotes faster and more effective healing. Modern studies2 have shown the benefit and potential of white cells in the inflammatory process in stimulating osteoprogenitor cells. PRF captures all monocytes, making bone graft stimulation more efficient.
Surgical procedure
We first extracted all the periodontal teeth and provided her with a removable prosthesis. Shortly thereafter her oral situation improved significantly.
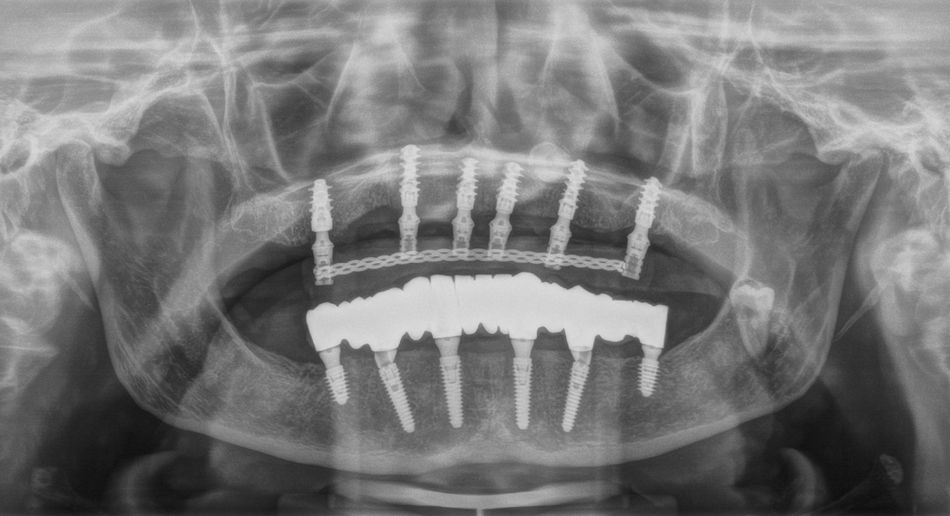
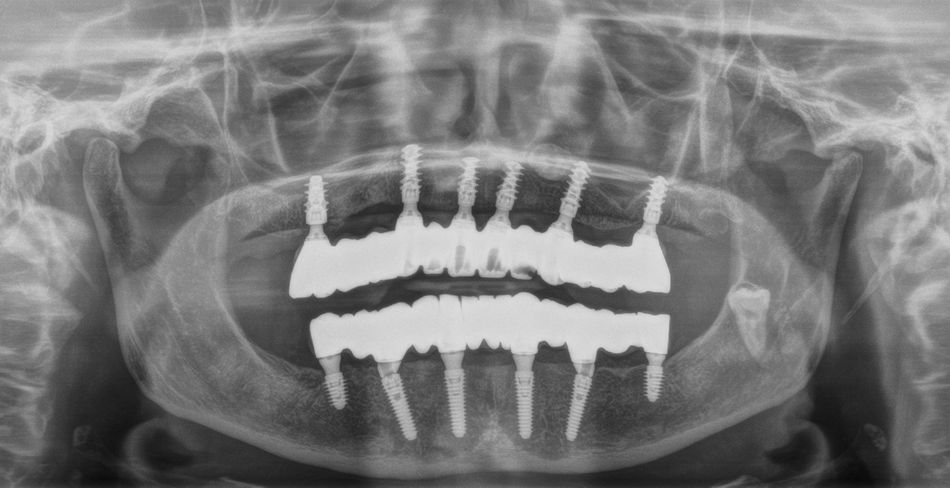
Later, we rehabilitated the mandibular arch with a Toronto prosthesis located on six implants (Fig. 3).
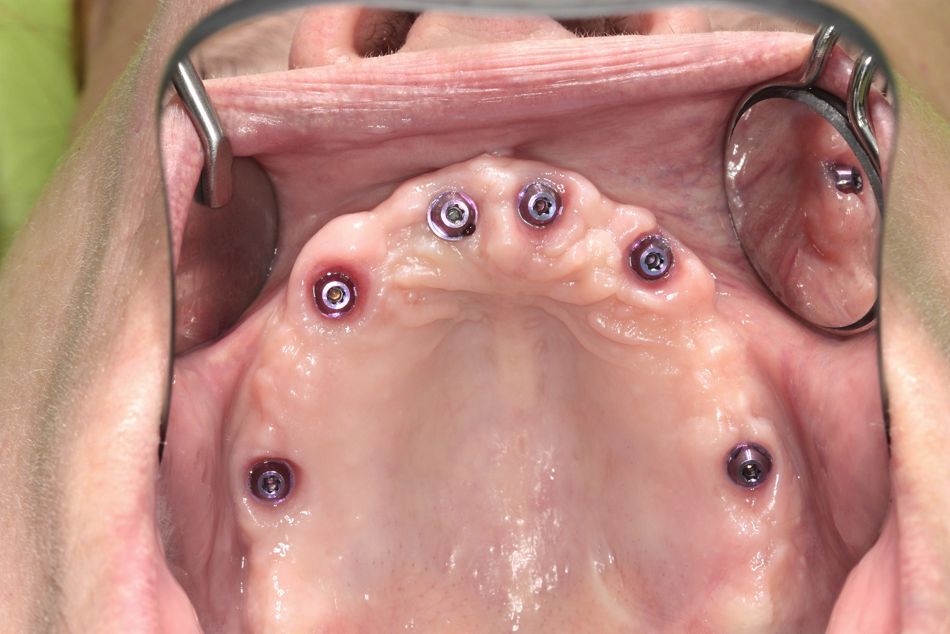
Since her oral hygiene was permanently improved, we decided to reward her by delivering a fixed prosthetic solution immediately loaded on six BLX implants.
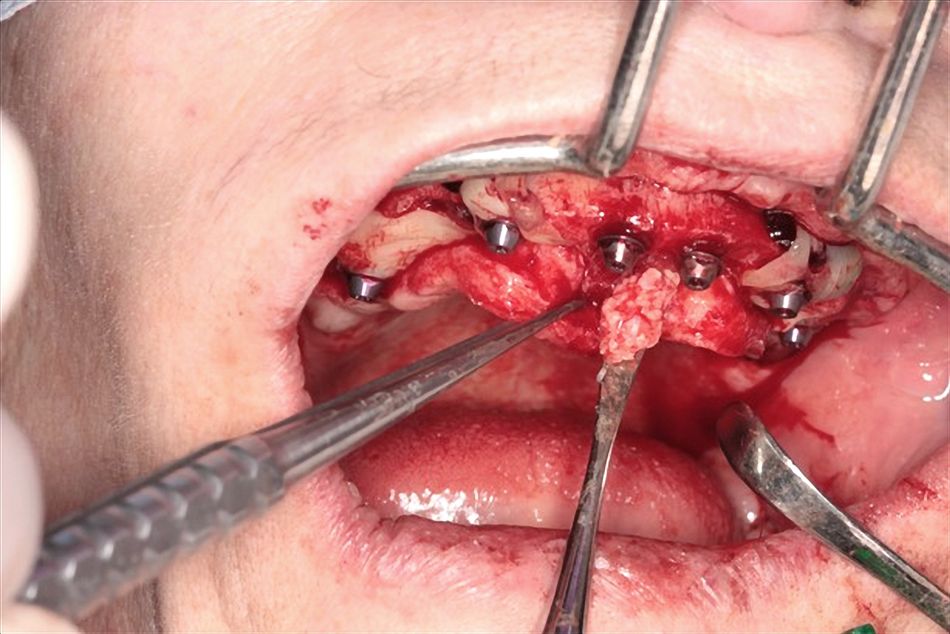
We started with a Summers’ technique sinus lift in the 16 region and placed A-PRF membranes.
We also decided to leave in situ 38 and 23 (which was horizontally inclined), both of which were totally impacted.
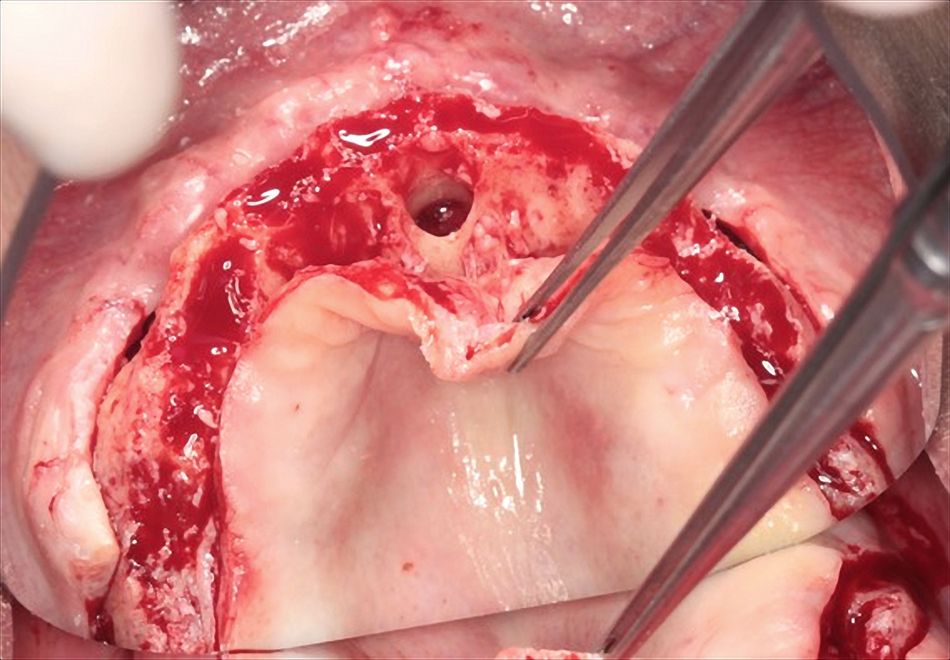
Since the incisive fossa and incisive foramen were quite wide, we decided to chip off the nasopalatine nerve at the caudal end and regenerate it with a biomaterial (maxgraft®, botiss biomaterials) mixed with I-PRF (Figs. 4,7,9).
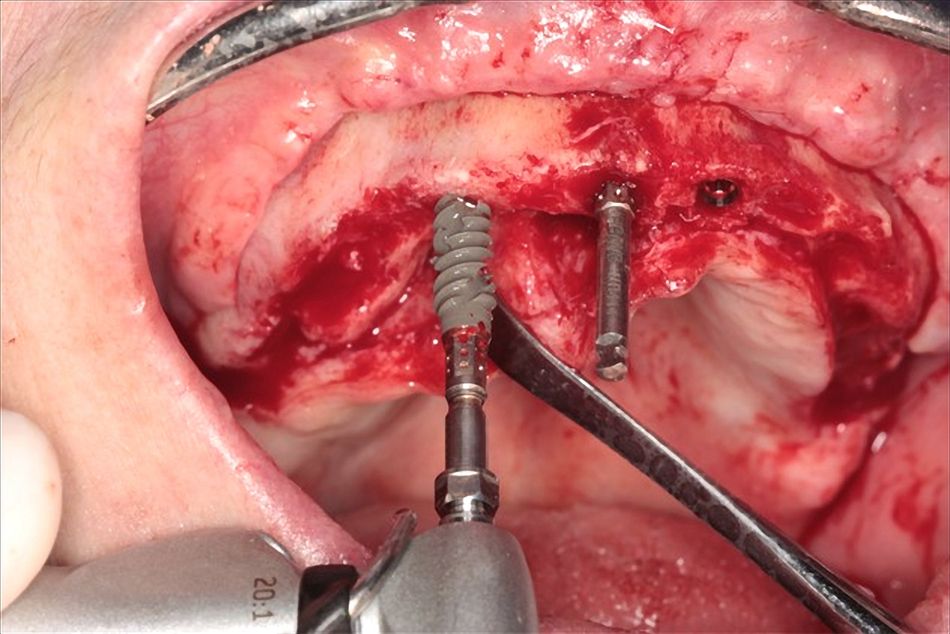
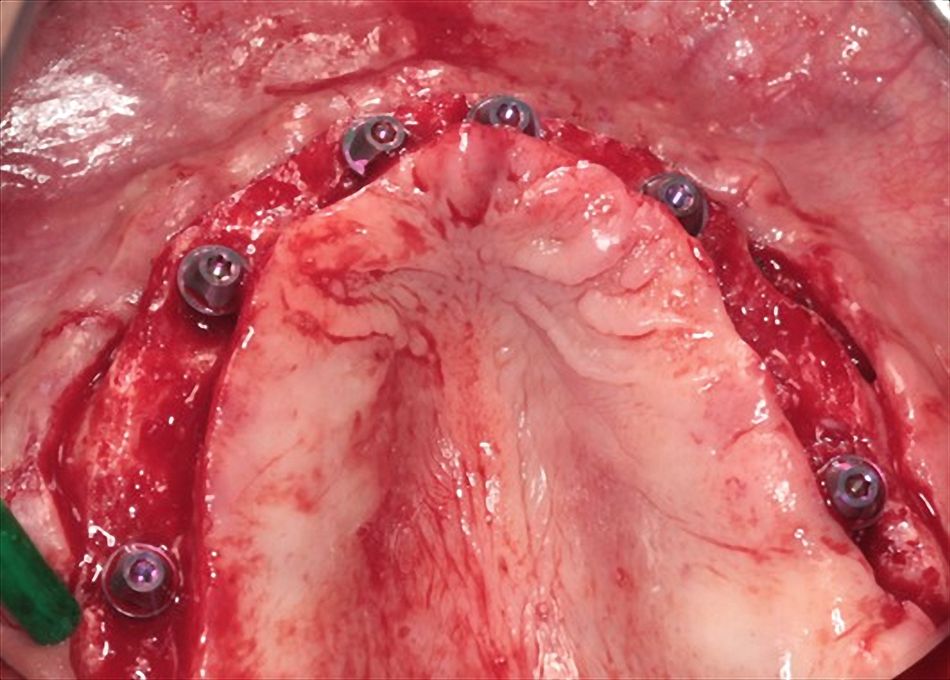
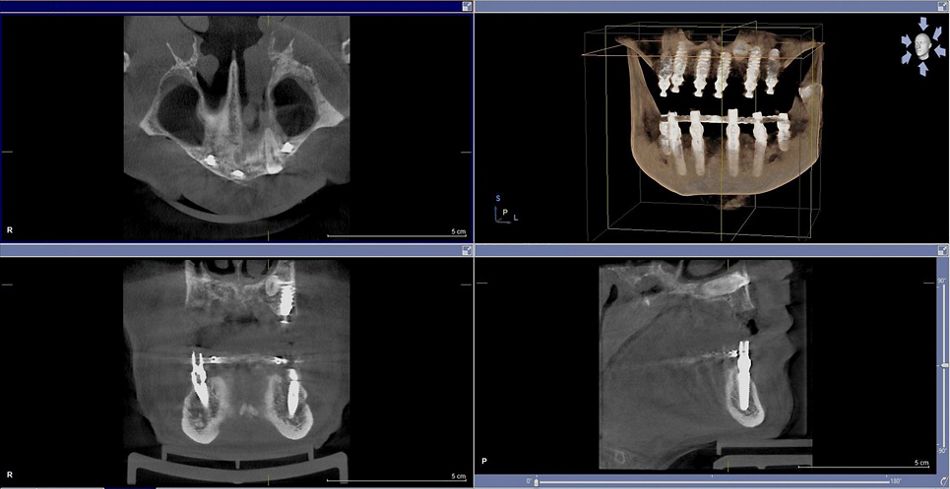
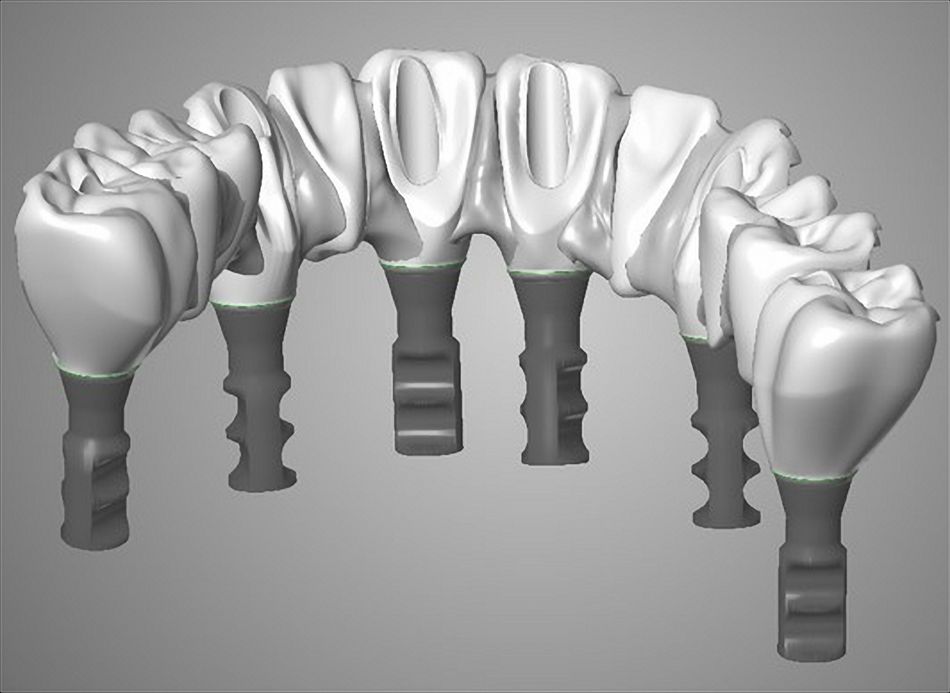
We placed Straumann® Roxolid® SLActive® 4.5mm-diameter implants in the sites 13, 11, 21, 24 and 26, and a 5.5mm-diameter implant in 16. All the fixtures were 10mm long except for 13 and 24, which were 12mm long (Figs. 5,6,8).
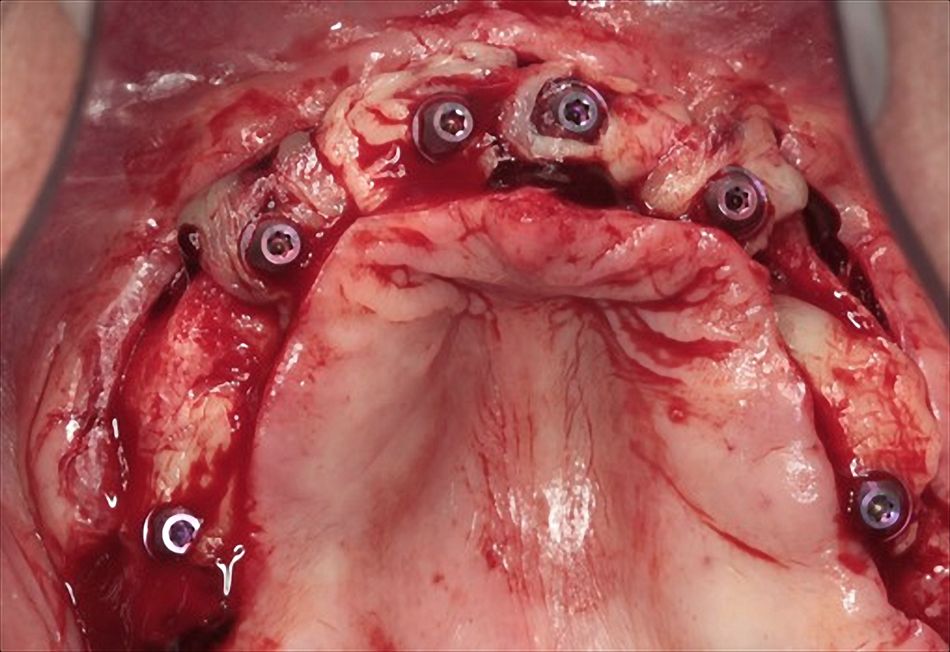
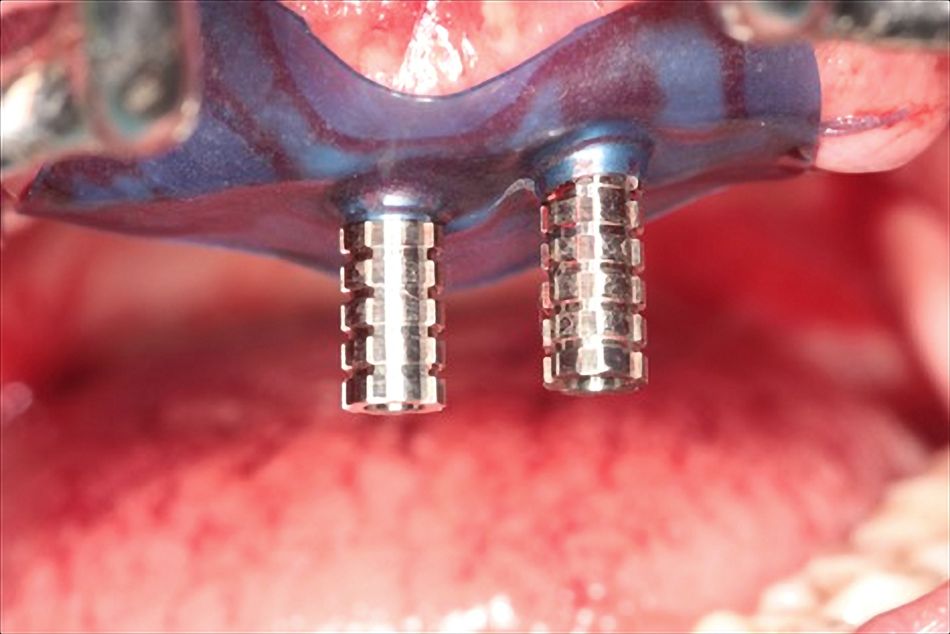
On the six BLX implants we screwed six SRA (screw-retained abutments) and, before closing the flap, we covered the fixtures with autologous A-PRF membranes (Fig. 10).
Prosthetic procedure
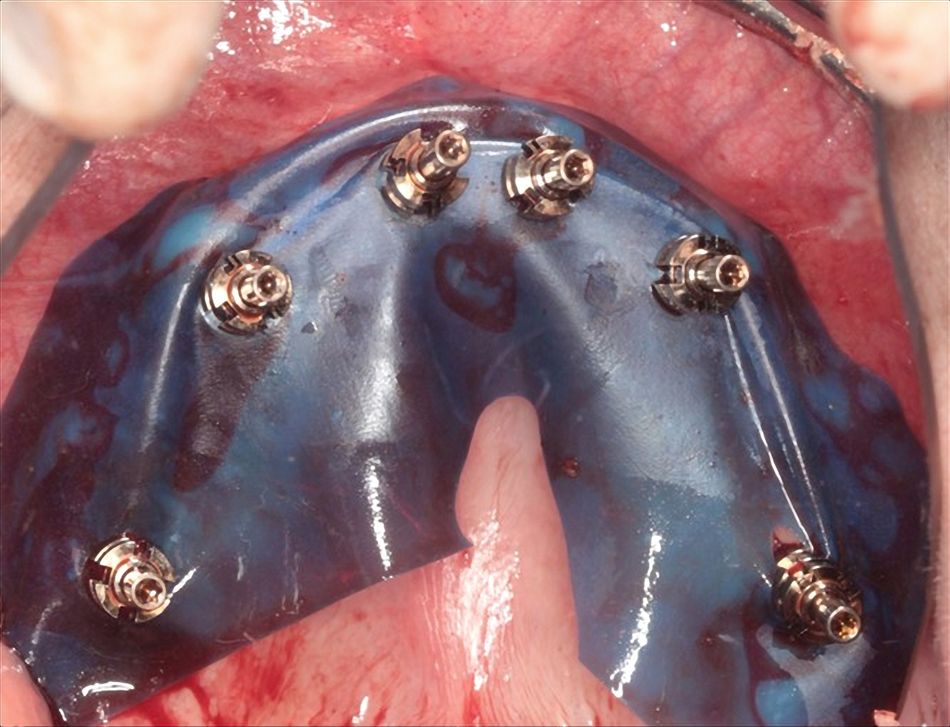
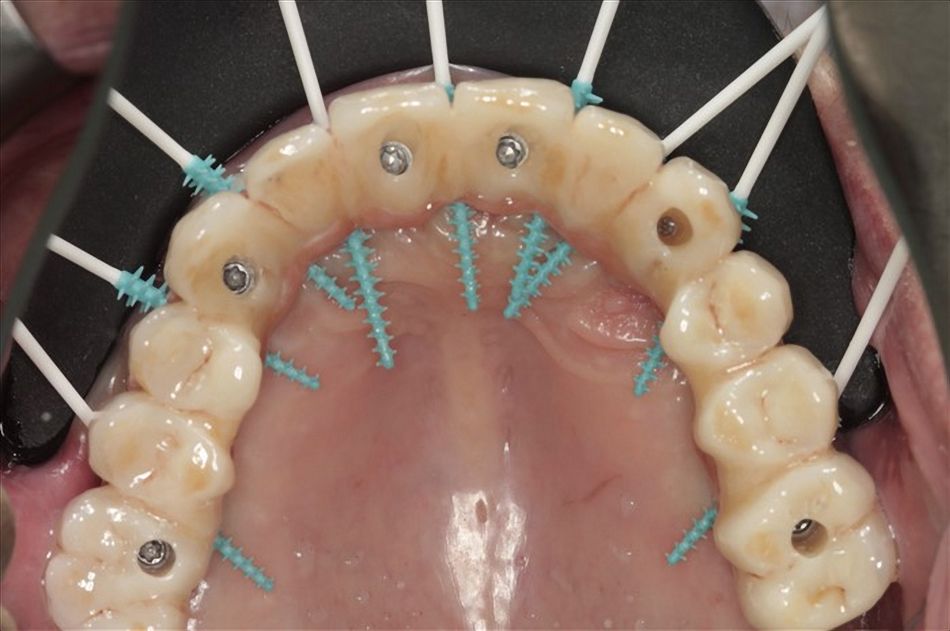
After the surgical steps we started with the prosthetic phases. First, we protected the operational field with a plastic dam and took an impression with a polyether impression material (Permadyne™, 3M ESPE) (Figs. 11,14).
In order to provide our dental technician with information about the vertical dimension and correct occlusion, we used a pattern resin and then fixed a transparent duplicate of the prosthesis onto the implants inserted in the 11 and 21 regions (Figs. 12,13,15).
A few hours after the surgery the patient received a fixed and protected solution screwed onto six implants (Figs. 16-19).
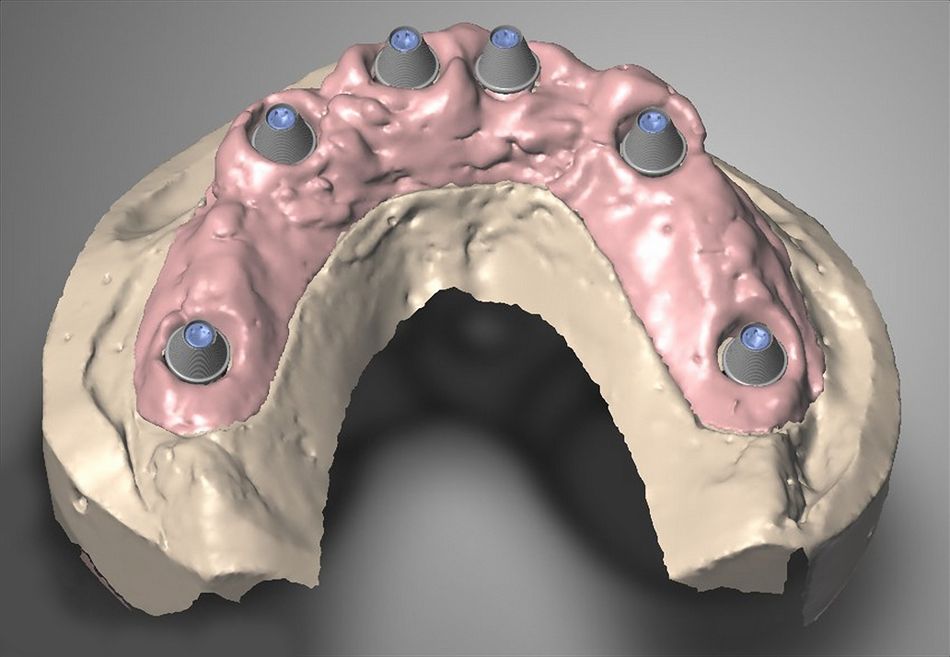
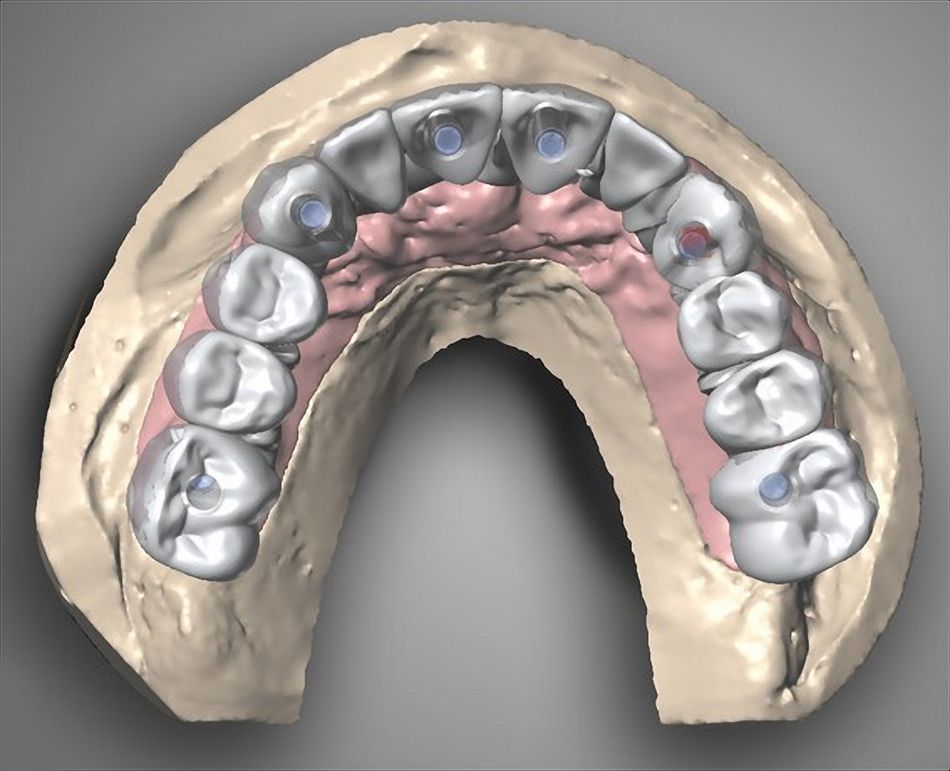
Six months later we produced the definitive impression by fixing the implants together with some resin, increasing the passivity and so reducing the tension (Figs. 20,21).
The mucosa healed extremely well with a large amount of keratinized tissue around the implants, and this was great proof of her commitment to practicing better oral hygiene (Figs. 32,33).
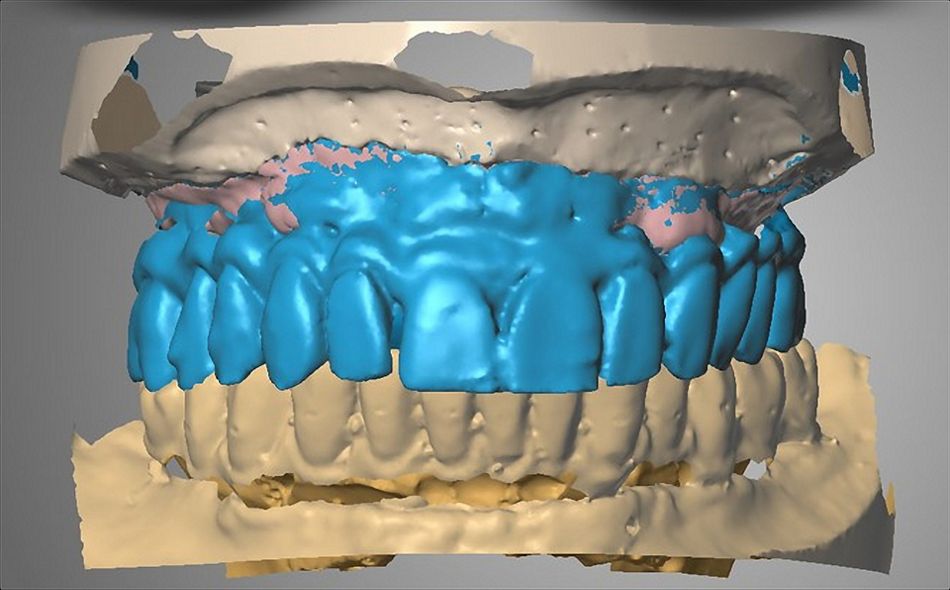
We then proceeded to the digital planning, and in our full-arch restorations we usually follow a partial digital workflow (Figs. 24,25,27). In this case we chose a multilayer high-translucency zirconium dioxide ceramic (zerion® ML).
We reproduced the vertical dimension with the provisional restoration and then duplicated it with a radiopaque polymer (Vivo TAC, Ivoclar Vivadent) so as to obtain a digital wax-up (Figs. 22,23).
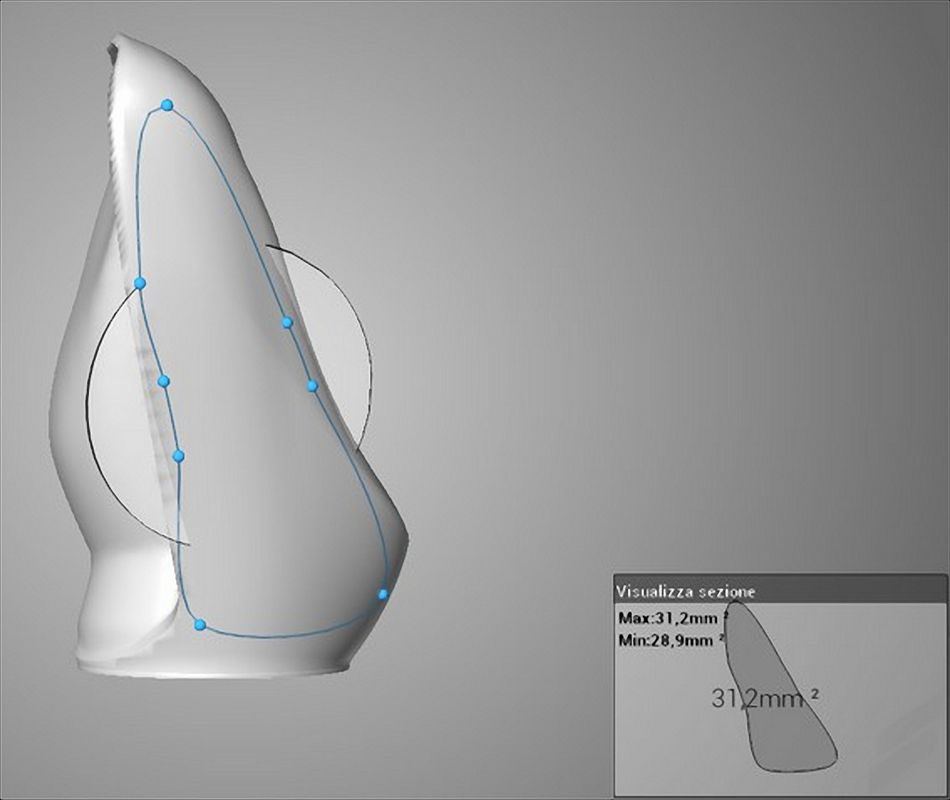
Using the zirconia, we discovered with our technician that the connector thickness in a Toronto prosthesis has to be at least 25 mm to be strong enough (Fig. 26). This material has excellent translucence and is highly resilient (Fig. 29).3
The buccal esthetic veneers were layered and customized by the dental technician, while the whole monolithic structure was milled (Figs. 28,30,31,34,35).
It is important to polish the zirconia perfectly on the occlusal surface in order to minimize abrasions (Fig. 37).
Last but not least, it is extremely important to create a cleaning space using the interproximal brushes (Fig. 36).
Treatment outcome
We are very happy with the results we achieved, because for us it was not only a technical and clinical challenge, it was also a matter of caring for this lady on a path of personal growth and regaining her self-esteem.
Since she has proved to have improved her oral hygiene permanently, she satisfies all the conditions for good long-term maintenance of the implants. After one year she is very glad and satisfied, and has finally managed to smile again without being ashamed of her appearance (Figs. 38, 39).
We are aware that, in a full-arch fixed rehabilitation, some chipping can occur in a veneered zirconia prosthesis. But after a careful postural and chewing analysis, we concluded that in her case we could succeed with this solution in both the upper and lower arches. But in order to avoid any risk we also provided a Michigan splint which the patient wears every night.