Surgical procedure
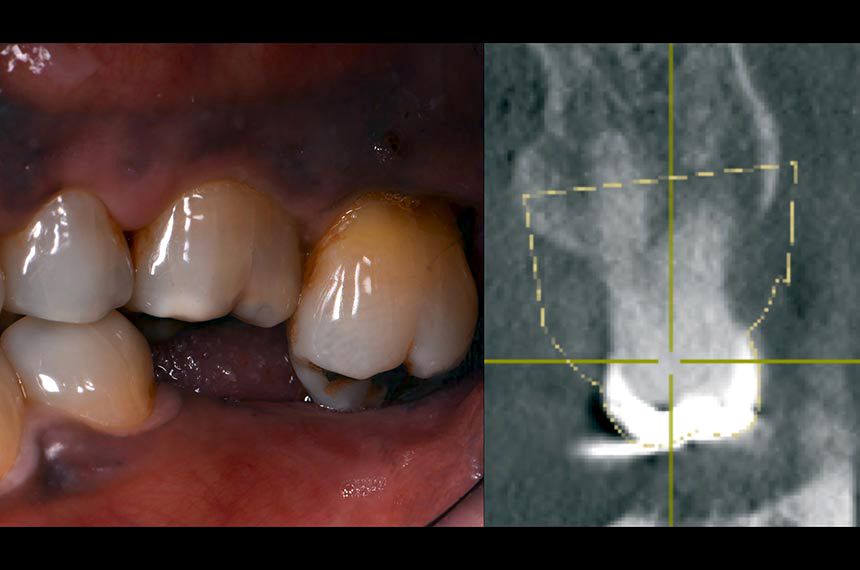
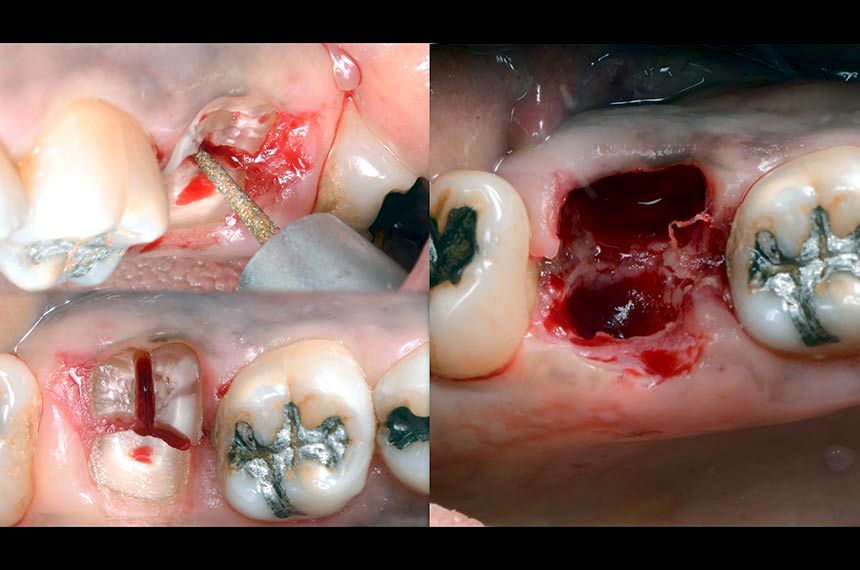
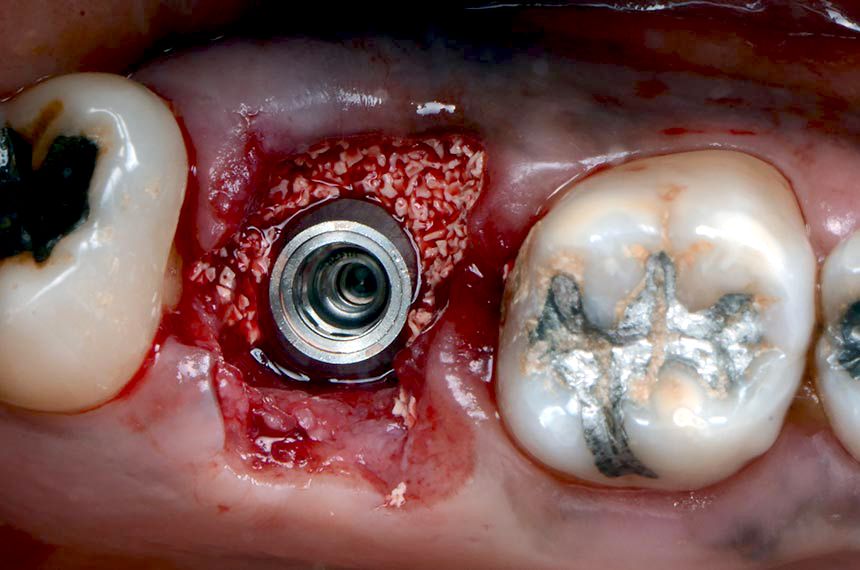
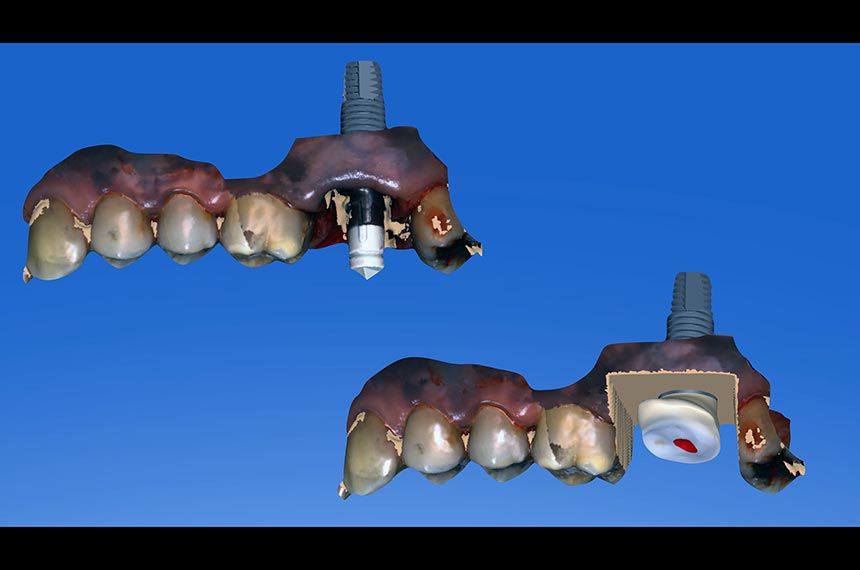
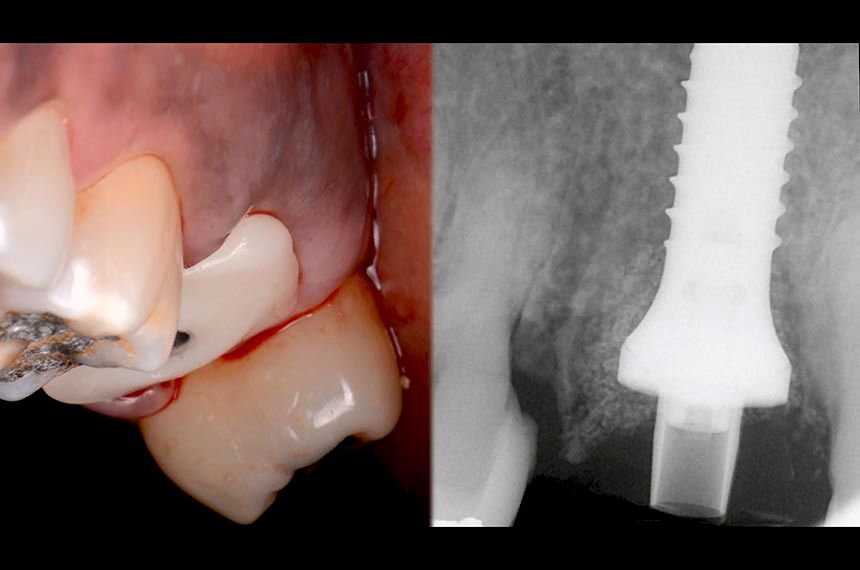
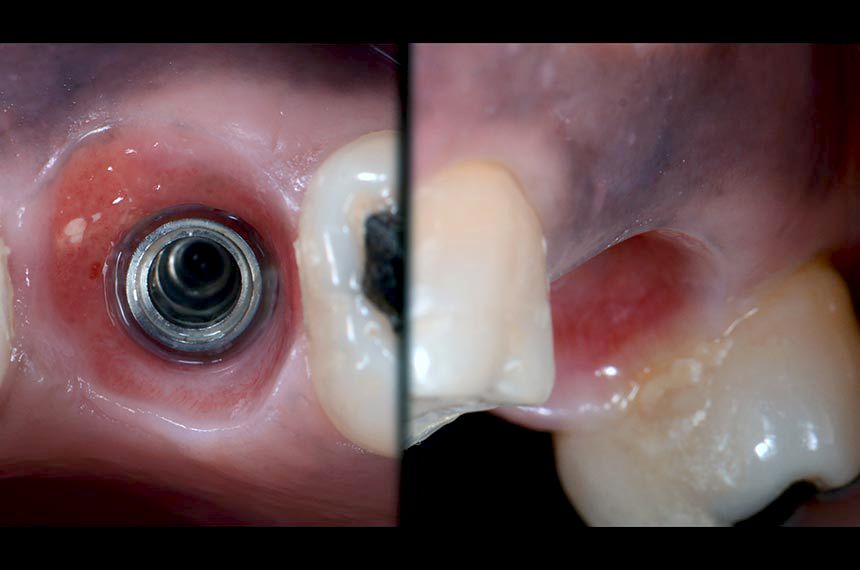
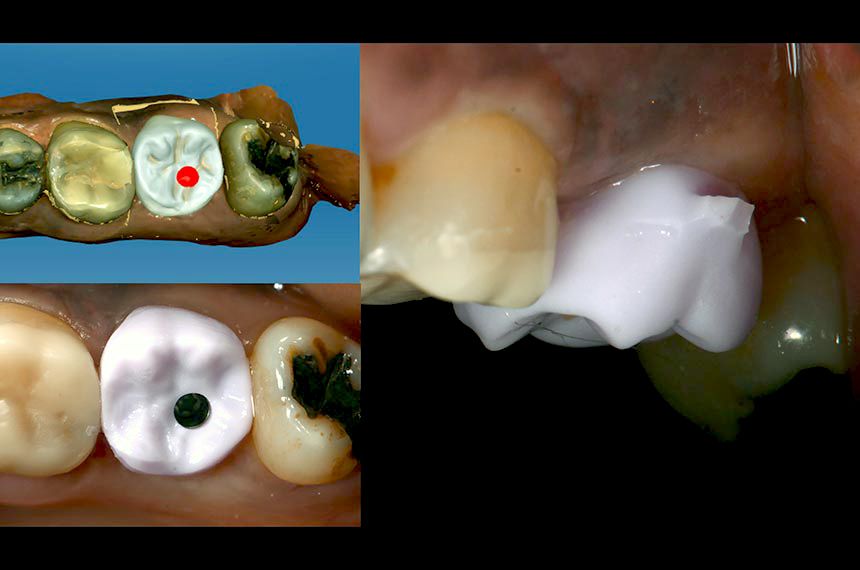
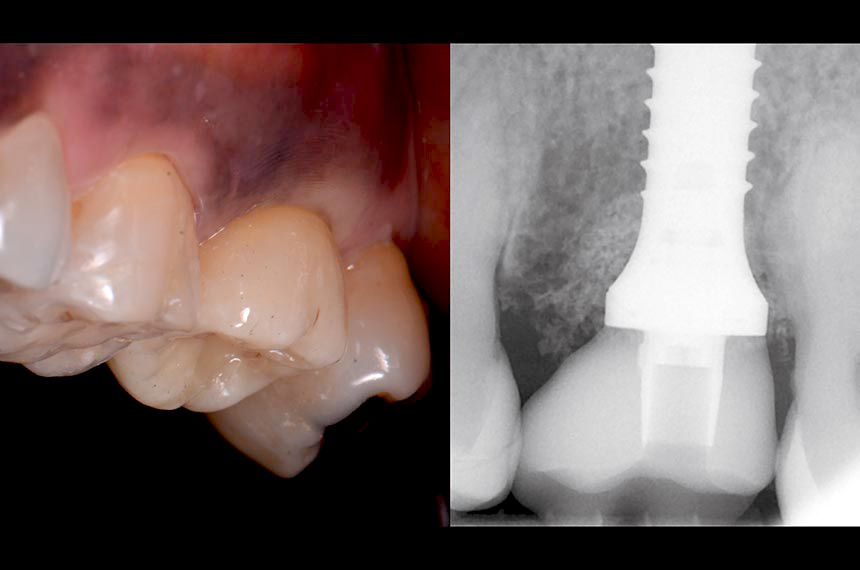
A major challenge encountered while undertaking immediate implantation in the molar area is the complexity of obtaining primary wound closure and coverage of the extraction site. Accordingly, this proposed protocol involves the chairside fabrication of a CADCAM abutment to seal the alveolar socket (SSA: Sealing Socket Abutment) immediately at the time of extraction-implantation (Finelle & al. 2016). Atraumatic flapless tooth extraction was performed by odontosection (Figs. 3,4) and separation of the supracrestal gingival fibers with periotomes. After extraction, the alveolar socket was liberally irrigated with sterile saline solution and cleaned with curettes to remove granulation tissue. A Straumann® Standard Plus Implant 4.8×12 WN was placed according to the instructions for use. The implant bed was prepared in the middle of the septum as virtually planned at the diagnostic stage (Fig. 5). The insertion torque was recorded during the placement and reached 30N/cm. Xenograft bone substitute (botiss cerabone®, granules 0.5-1mm, 1×0.5cc, Botiss) was packed to fill the alveolar socket surrounding the implant (Fig. 6). (Chu et al. 2012). To obtain closure of the socket at the time of extraction, an innovative protocol has been established to allow digital impression and immediate customized CADCAM abutment at the time of the surgery. A scan body (Cerec, Sirona) was connected to the platform of the implant to allow the intra-oral scanner (Omnicam, Sirona) to capture virtually the 3D position of the implant (Fig. 7). Immediately after acquisition, the SSA was designed on the prosthetic software (Fig. 8). The design process consists of: 1. Reproducing the outline of the previous freshly extracted molar in order to create a mechanical seal between the oral cavity and surgical site. The transmucosal portion is designed with a concave shape in order to accommodate for proper biological space (Finelle 2011, COIR). 2. Creating an ideal emergence profile to guide soft healing and positioning during the maturation process (Dual Zone concept Tarnow, Chu). The digital file was then exported to an in-office milling system (MCXL, Sirona) for fabrication of the SSA abutment (telio CAD 16, Ivoclar) in a chairside manner (Fig. 9). During the milling (15 minutes), sterile gauze was placed on the surgical site and post-operative recommendations were given to the patient. After milling, adhesive cement (Multilink abutment, Ivoclar) was used to assemble the SSA device onto the Variobase abutment for Cerec (Variobase C WN, Straumann) (Fig. 10). Finally, the SSA was inserted into the implant (with manual insertion torque) to support the surrounding soft tissues and provide a seal to the bone substitute material without the use of a biological membrane (Fig. 11)(Chu & al. 2012). Immediately after the surgery, post-operative periapical radiographs were taken to verify the proper position of the implant (Fig. 11). At the one week follow-up, the patient reported an uneventful post-operative recovery. The clinical examination at one week showed favorable soft tissue healing with minor inflammation (Fig. 12). After 12 weeks of osseointegration, soft tissue around the SSA abutment was healthy, and the buccal contour was maintained (Fig. 13). Removal of the abutment at the time of impression-taking showed a healthy and anatomical prosthetic emergence profile and a well-designed transmucosal portion (Fig. 14). A digital impression (Omnicam, Cerec, Sirona) using Scanbody for Cerec was taken for implant-supported restoration (Fig. 15). Finally, an implant screw-retained crown was designed (Fig. 16) on the Cerec Software (Cerec 4.4) and milled out of a monolithic lithium disilicate block (Emax CAD, Ivoclar) (Kapos & al. 2014). Before sintering, a blue CAD crown was tried in to validate the shape, contact point and occlusion (Figs. 16). The emergence of the implant screw axis allowed for a screw-retained prosthesis as originally planned (Fig. 17). The crown was stained and the occlusal grooves were readjusted to improve occlusal anatomy. The implant crown was bonded to a titanium base abutment adapted for the Cerec implant block (Variobase C, Straumann) with a resin cement (Multilink Hybrid Abutment, Ivoclar). At the time of final crown delivery (Fig. 18), we noticed the adequate emergence profile of the peri-implant soft tissues precisely fitting with the transmucosal anatomy of the ceramic crown. Final insertion torque (35N/cm) was applied, and the access hole was covered with restorative composite (Gænial A2, GC) (Fig. 19). A post-operative periapical radiograph was taken to verify the seating and marginal integrity after insertion (Fig. 19). While #27 was undergoing restoration, #36 and #37 were treated by surgical and restorative procedures, and two screw-retained single crowns were inserted (Fig. 20) in order to restore adequate prosthetic space (Fig. 21).