Initial situation
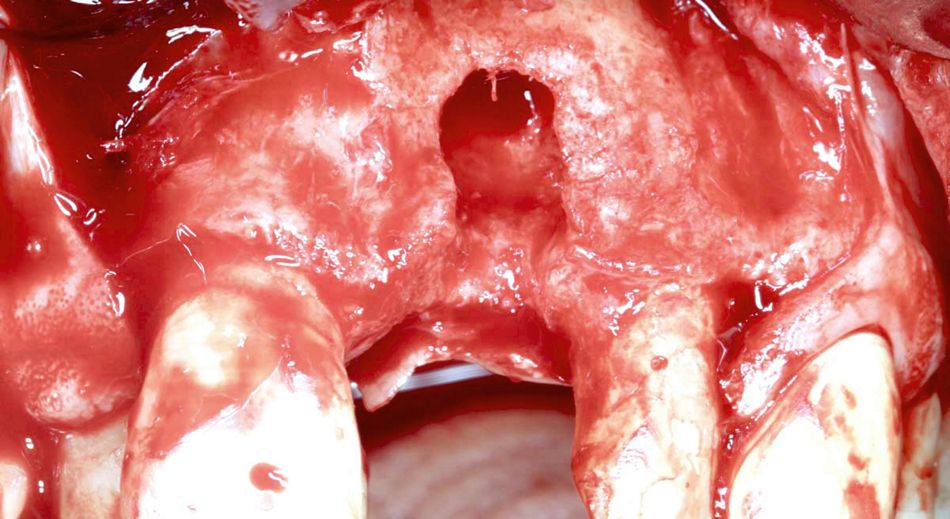
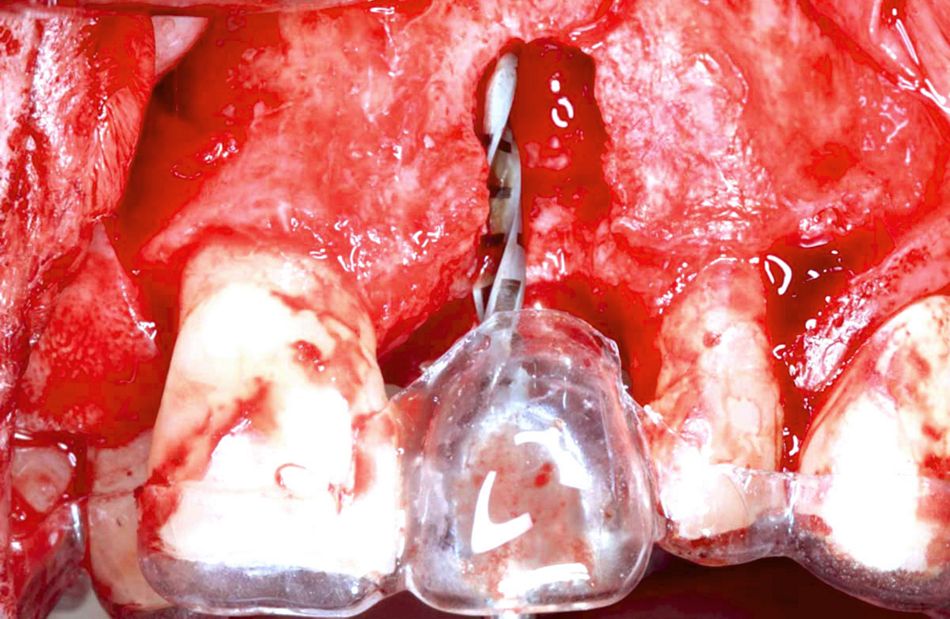
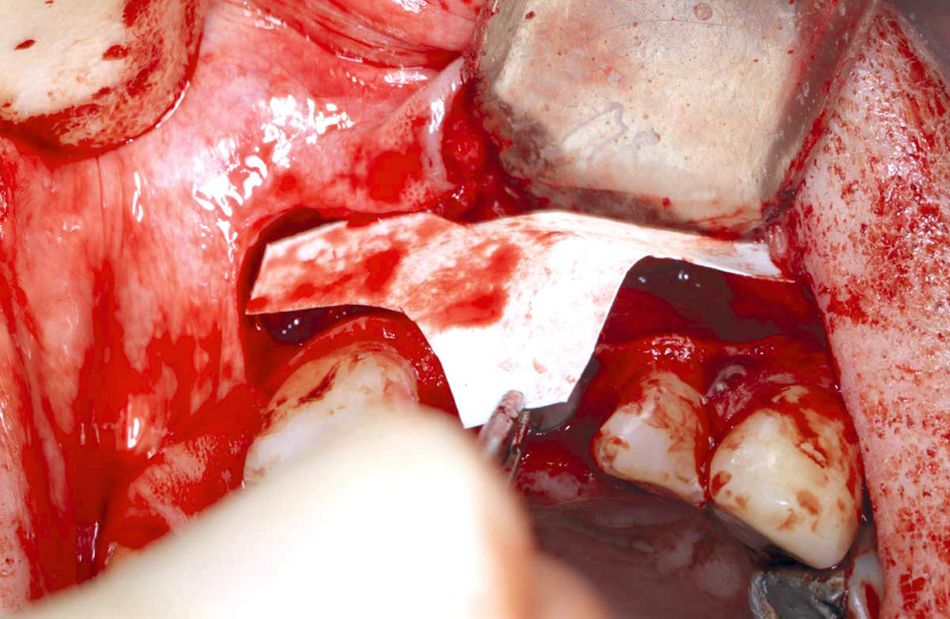
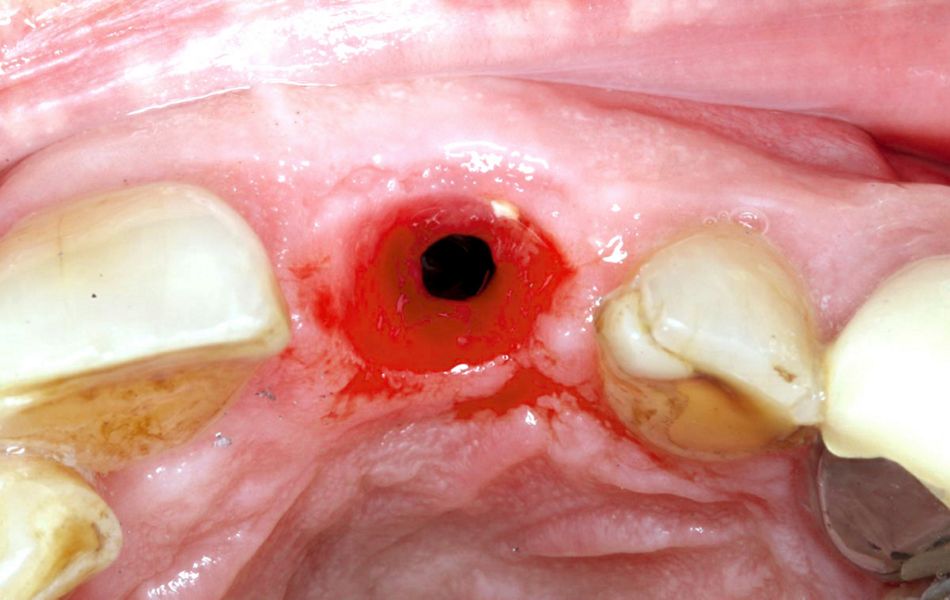
A 68-year-old patient was referred from a colleague who already had to extract tooth #21 due to a failing post crown with cracked root. The patient is fit and healthy, not taking any medications, a non-smoker and with good oral hygiene. The missing front tooth site was left to heal for two months (Fig. 1). The occlusal view of the missing #21 showed severe buccal bone loss, which was even more visible after the flap was opened (Figs. 2-3).
Treatment plan
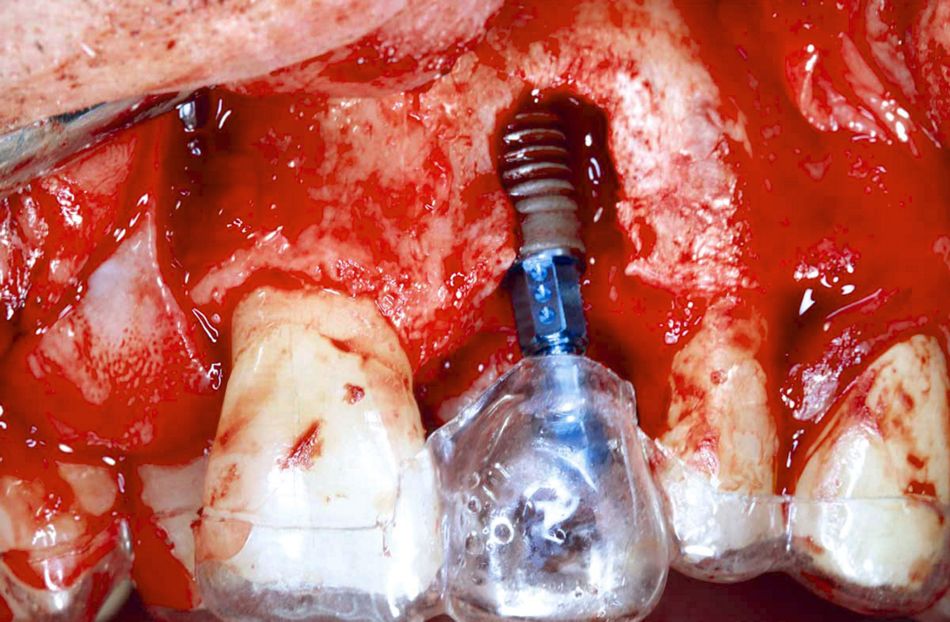
The surgery was planned with Straumann® Guided Surgery to obtain restoratively ideal implant positioning and the correct angulation of the implant. The surgical planning revealed that the implant had to be placed within the prosthetic envelope and in correct fourth dimension to allow for aesthetic restoration. Therefore, bony perforation and dehiscence were anticipated, and the site had to be grafted. A Straumann® Bone Level Tapered Implant (BLT) was planned to help achieve satisfactory primary stability and minimize bone drilling, due to the tapered shape of the apex of the implant.
A prosthetic template (surgical guide) was prepared beforehand and used for the initial osteotomy.
Surgical procedure
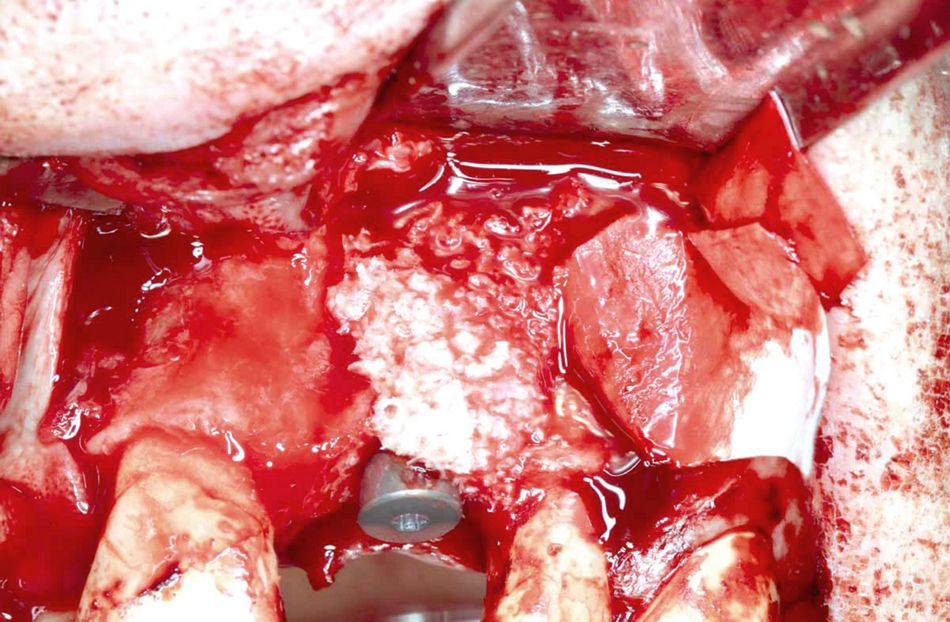
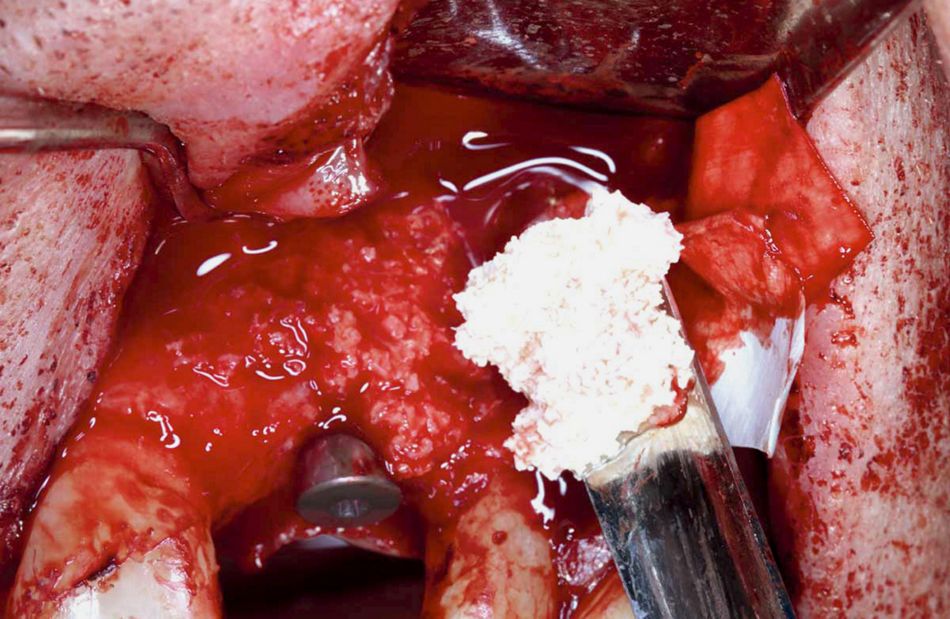
After the administration of local anesthesia, the flap was raised with vertical releasing incisions, and the surgical template was put in place (Figs. 3-4). Next, a Straumann® BLT Implant 4.1 x 14 mm with an RC healing abutment 5x4 mm were placed (Figs. 5-6). Afterwards, the exposed threads of the dental implant were covered with maxgraft® cancellous granules to gain vital bone around the implant (Figs. 7-13). maxgraft® is a processed and freeze-dried allogenic bone substitute with excellent osteoconductive properties that will remodel into native bone.
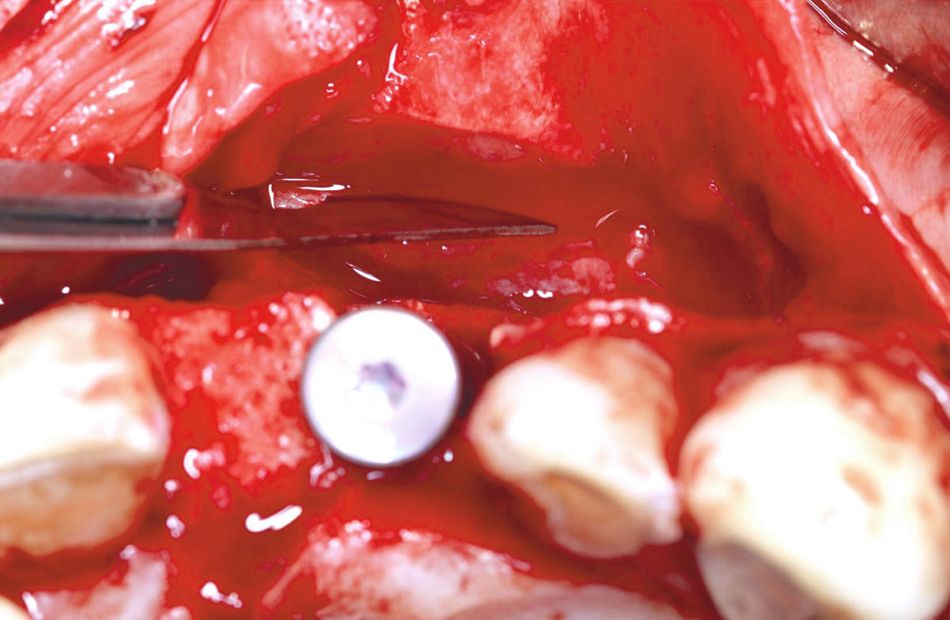
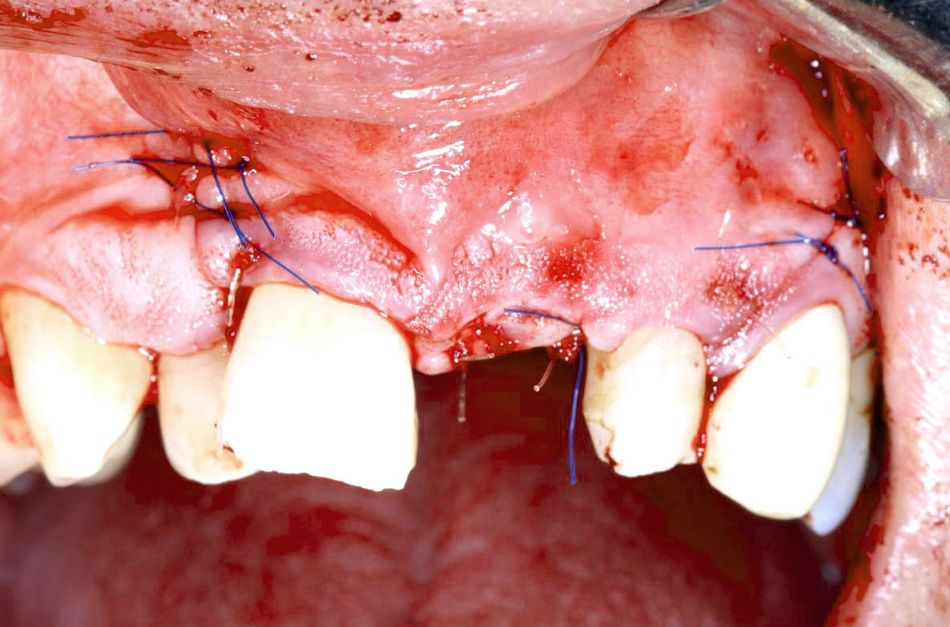
Accordingly, the site was covered with cerabone® granules 0.5 – 1.0 mm, a slowly resorbable bovine bone substitute, in order to prevent resorption, gain convexity and preserve the long-term aesthetic outcome (Fig. 8). The layering technique in combination with maxgraft® was chosen because ITI guidelines recommend that native bone should ideally cover the exposed implant surface. A periosteal releasing incision was performed before applying the granules in order to ensure that the mucogingival flap could be closed in a tension-free manner with the additional volume of the grafting material (Fig. 9). The shape of the Jason® membrane, a porcine pericardium membrane with a prolonged barrier function, was modified using a template (Fig. 10). The Jason® membrane was cut according to the template extra orally and fixed in place using 3mm titanium pins to achieve maximum stability, which has been linked to predictable guided bone regeneration outcomes (Fig. 11). The GBR was performed using the layering technique, first applying the maxgraft® and then the cerabone® covered with Jason® membrane (Figs. 12-14). Jason® membrane was used to cover the augmentation site to prevent soft tissue cells from proliferating into the site (Fig. 15). The GBR was performed up to the level of the healing abutment, which was also used to tent the membrane. In the authors’ view this method can provide more predictable GBR results. The site was sutured with 5/0 Prolene sutures and left to heal for 12 weeks (Fig. 16). Post-operative instructions verbally and in writing were given to the patient, and sutures were removed two weeks later. After 12 weeks of uneventful healing, the healing abutment was partly visible through the gingiva, and the gum looked healthy (Fig. 17).
Prosthetic procedure
A chairside temporary crown was built, and an RC temporary abutment was used with the help of the surgical guide (Figs. 18-20). Protemp shade A3 was used for the build-up, and it was subsequently shaped and polished with softlex disks to produce a concave sub-gingival profile, a satisfactory gingival seal, a natural zenith and a convex supra-gingival contour (Figs. 21-22). Occlusion was adjusted to rule out tensile forces or interferences on anterior guidance. Over a couple of visits the temporary was adjusted with the aim of contouring the gum to achieve a more natural look utilizing the prosthetic soft tissue sculpture technique (Figs. 23-24). Teflon tape and flowable composite were placed in each visit to protect the screw head. Before integrating the final crown, the gum looked healthy (Fig. 25).
Final result
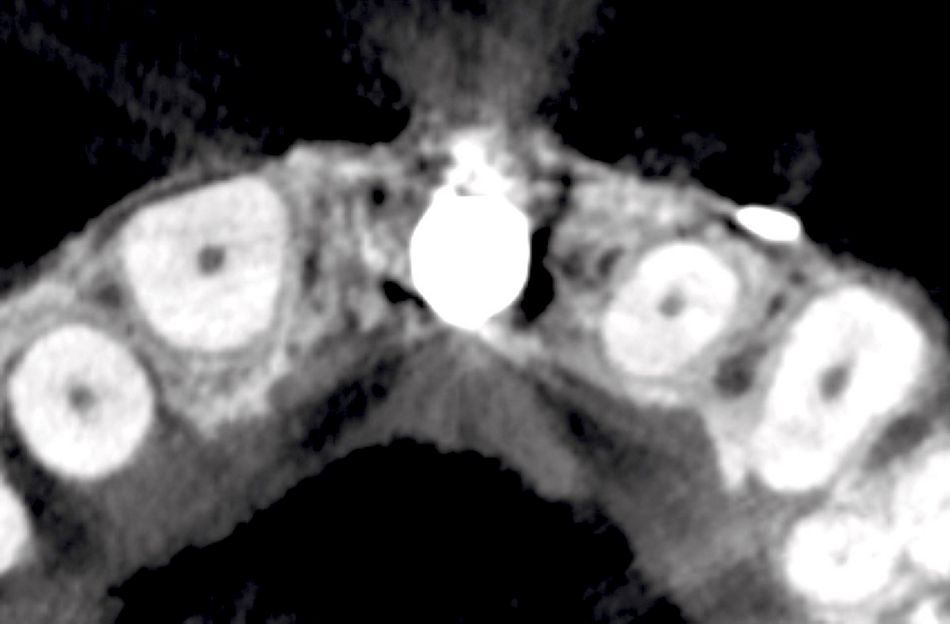
A customized impression pick-up was used, and the final screw-retained crown with Co/Cr Straumann CAD/CAM abutment was prepared using angulation correction technology. The crown was fitted and torqued to 35 NCM (Figs. 26-27). The occlusal view after integration of the crown showed satisfactory convexity, representing the regenerated hard tissue on the buccal aspect (Fig. 28). The Cone Beam CT scan taken 20 weeks after implant placement showed 2.5 mm labial bone (with the temporary crown in place) (Fig. 29). The final CT showed 2.4 mm bone gain on the shoulder of the implant, which suggests a long-term peri-implant bone stability, ensuring a predictable and satisfactory aesthetic outcome (Fig. 30). The final result 24 weeks after placement showed aesthetic and natural results, and the patient was highly satisfied (Fig. 31).
Findings
One Size Doesn’t Fit All:
Even in aesthetically challenging areas a GBR with a layering technique together with restoratively driven surgery planning can result in highly aesthetic implant outcomes. The bone gain on the shoulder of the implant suggests long-term implant success and aesthetics. However, it is necessary to apply our biological understanding of bone healing when deciding what bone graft needs to be placed where in peri-implant defects.
Exposed implant threads are usually better covered with autogenous grafts and allografts (in this case maxgraft® cancellous granules), while convexity is better achieved with a xenograft (in this case cerabone®).