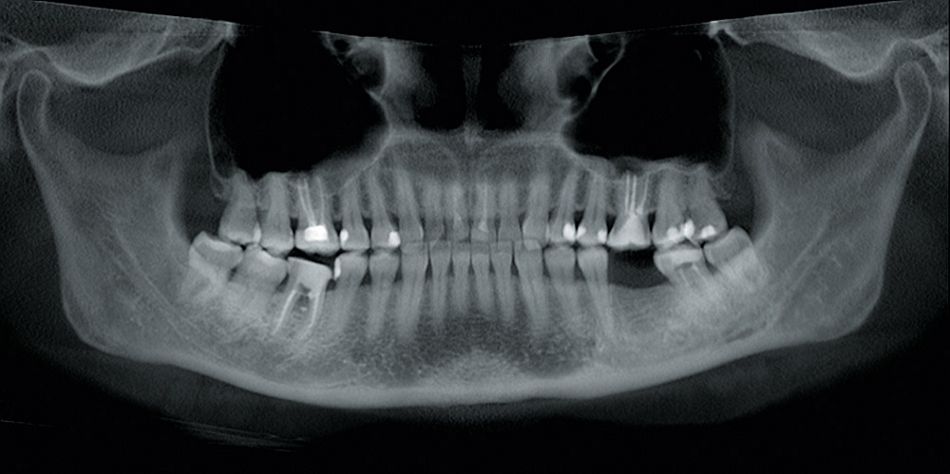
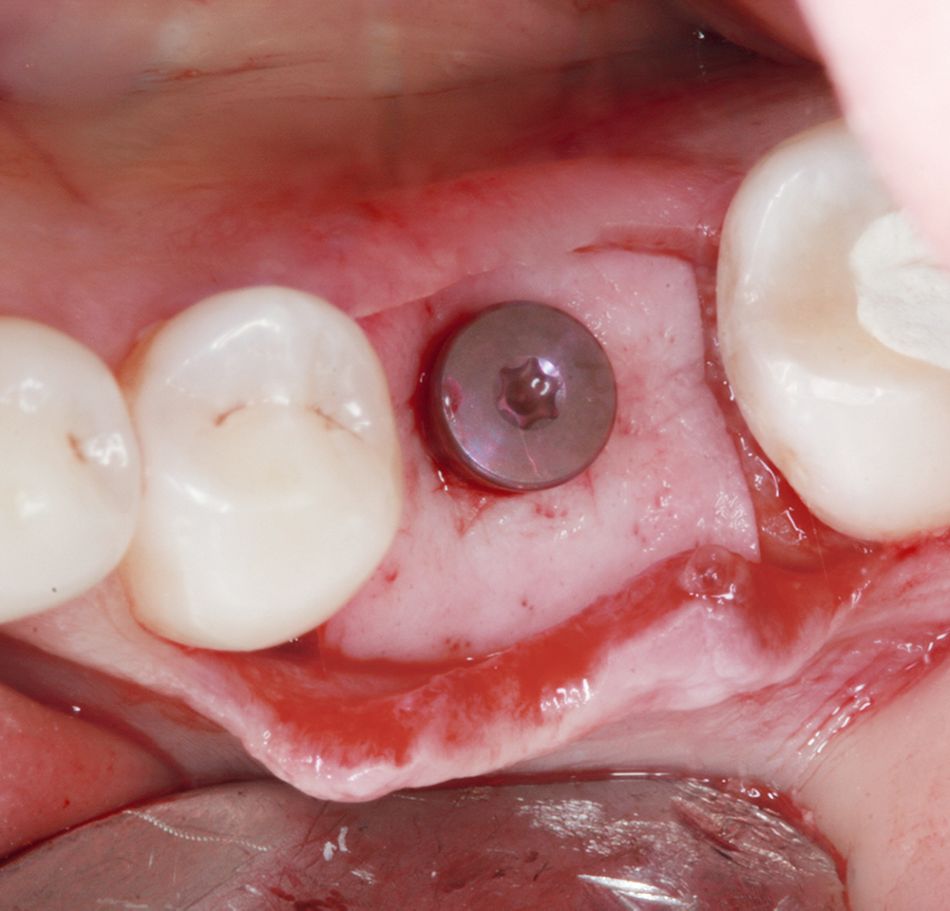
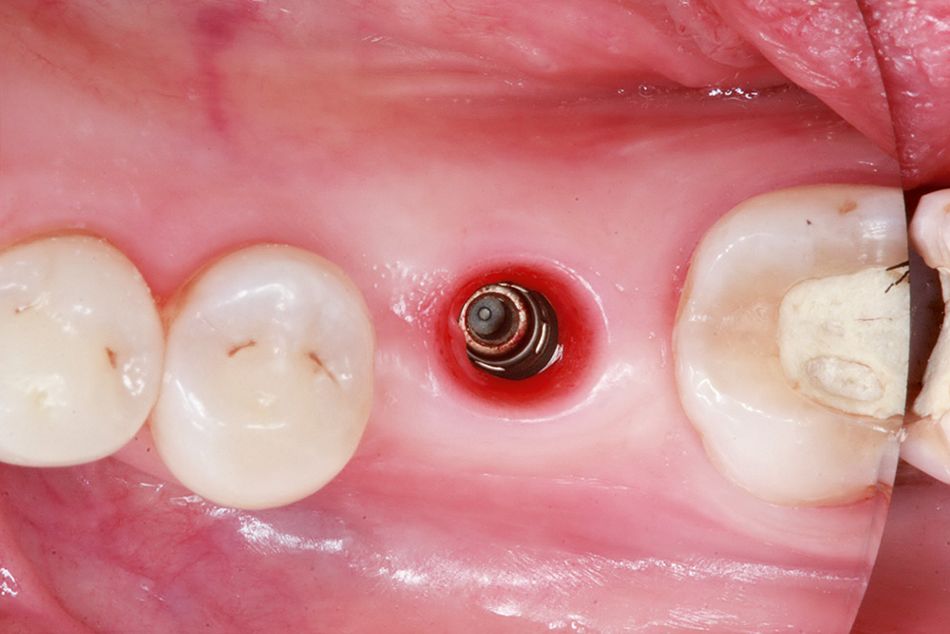
A 54-year old patient with a missing tooth 3.6 came to our clinic and asked for a restoration of an implant-borne crown. He demonstrated good oral and systemic health; no significant health problems that might influence the treatment were marked. Intraorally, the tooth gap in region 3.6 was noted. The alveolar ridge was slightly flattened and a width of the fixed, keratinized mucosa of approximately 7 mm was observed (Figs. 1, 2).
Treatment procedure
The treatment plan included the placement of a Straumann® Bone Level Implant and, if necessary, a simultaneous thickening of the peri-implant mucosa. Mucosal thickness has been shown to be an important factor in the etiology of early crestal bone loss around dental implants. A clinical study demonstrated that a mucosal thickness of 2 mm or less increased the risk of crestal bone loss within the first year after implantation . Consequently, in cases of thin biotypes, we perform a thickening of the soft tissue by application of the acellular porcine collagen matrix botiss mucoderm®. The matrix is applied instead of an autogenous transplant to spare the patient the harvesting from the palate.
Surgical procedure
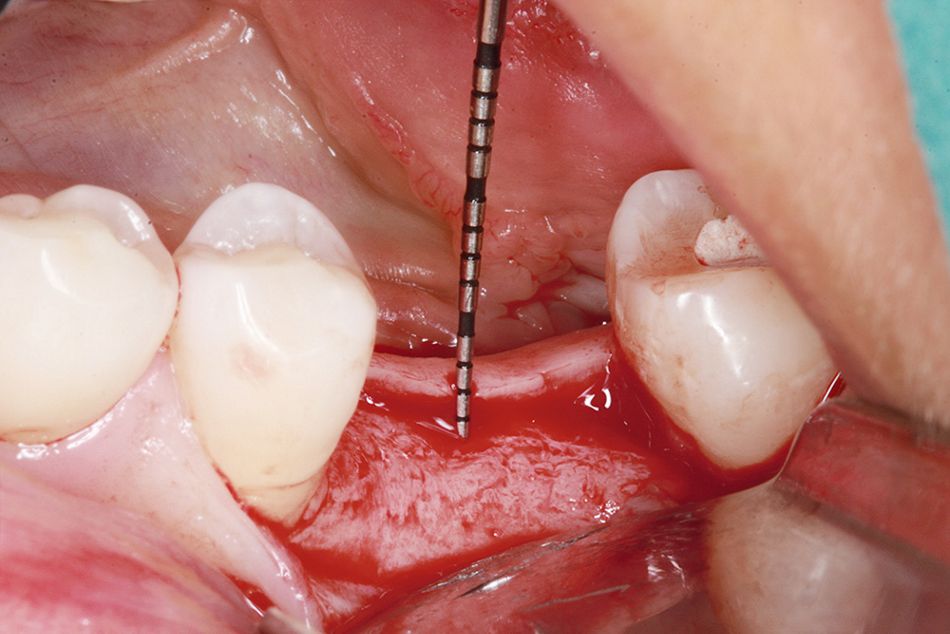
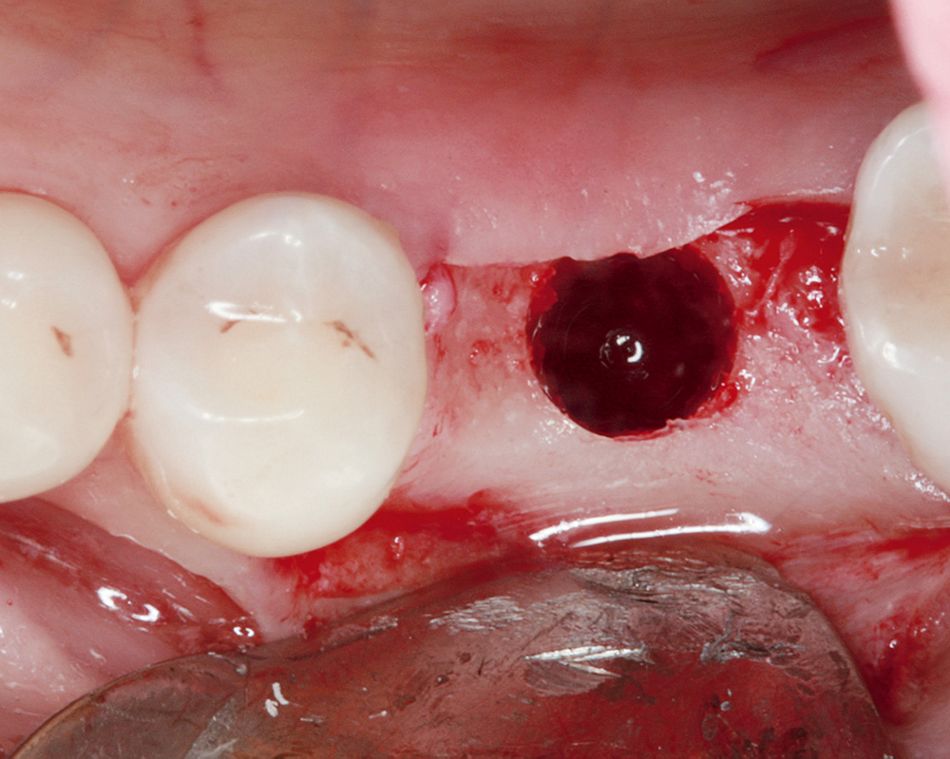
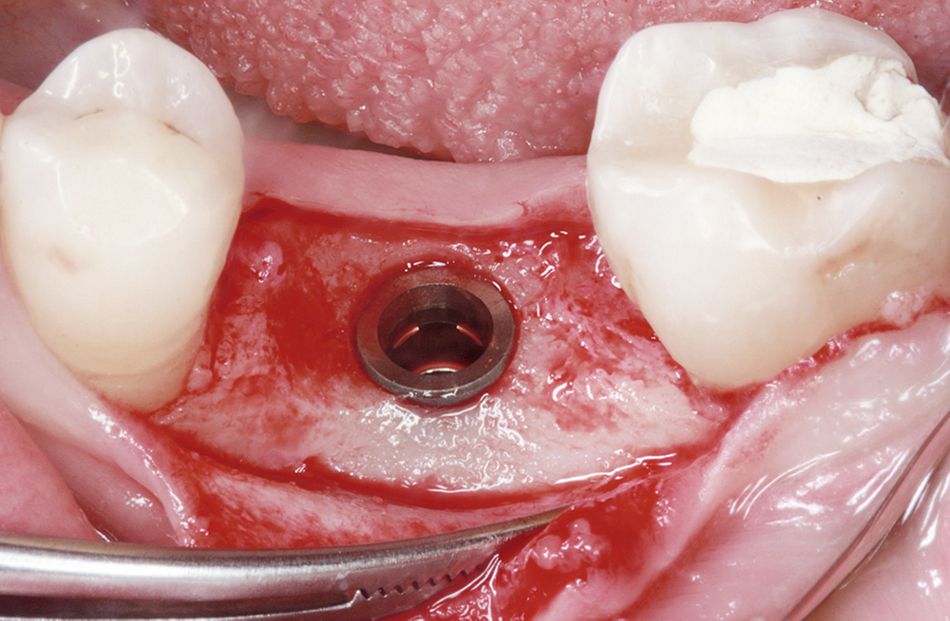
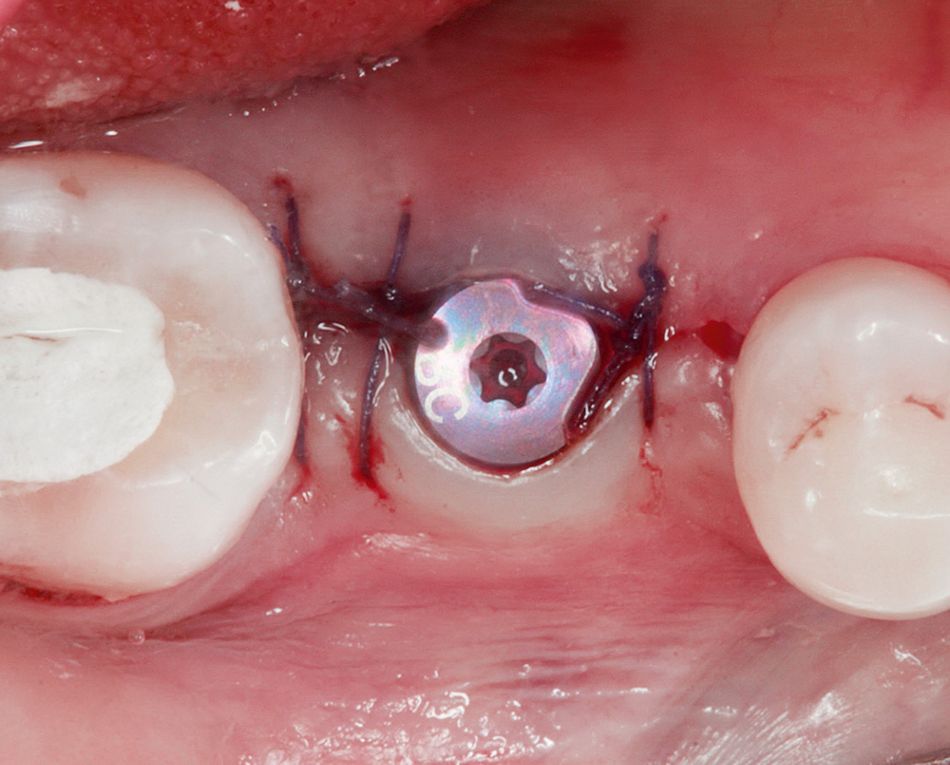
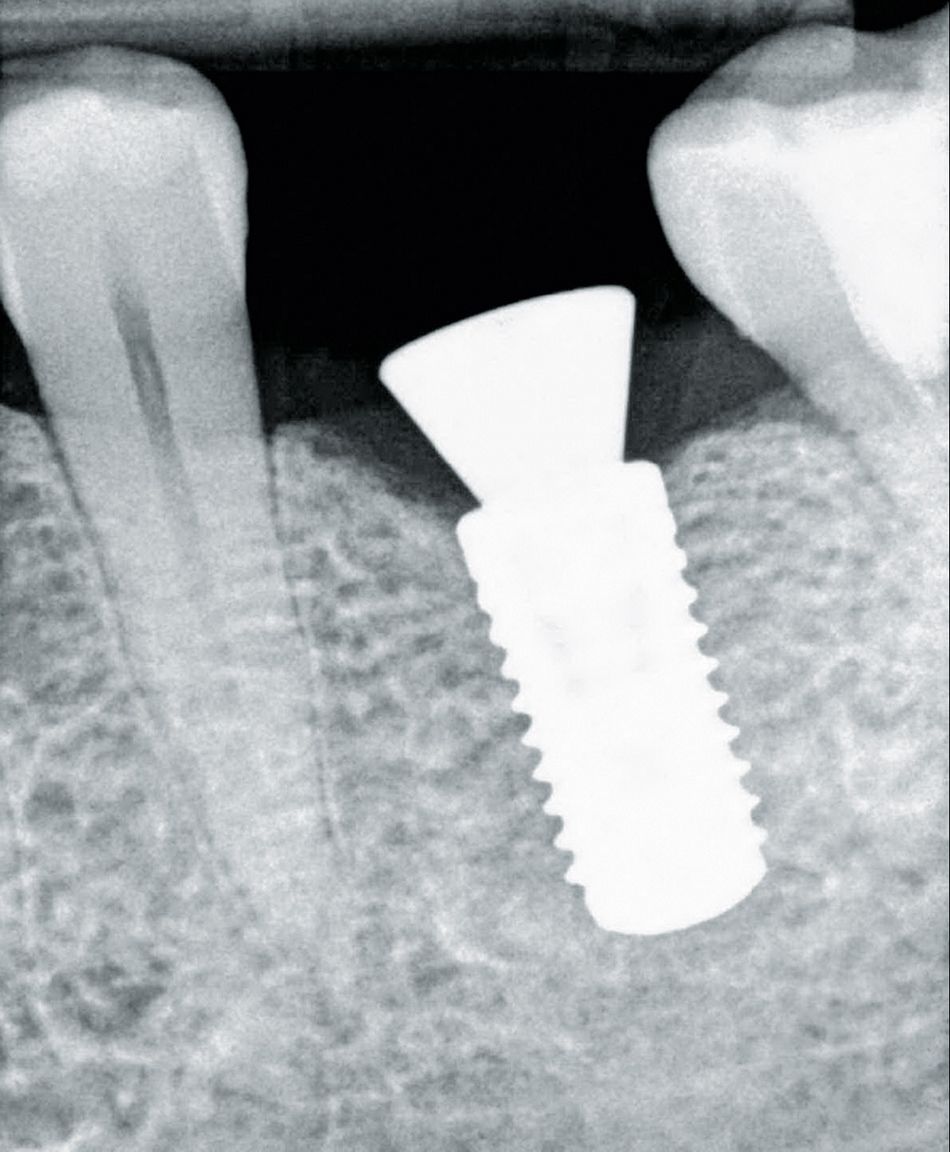
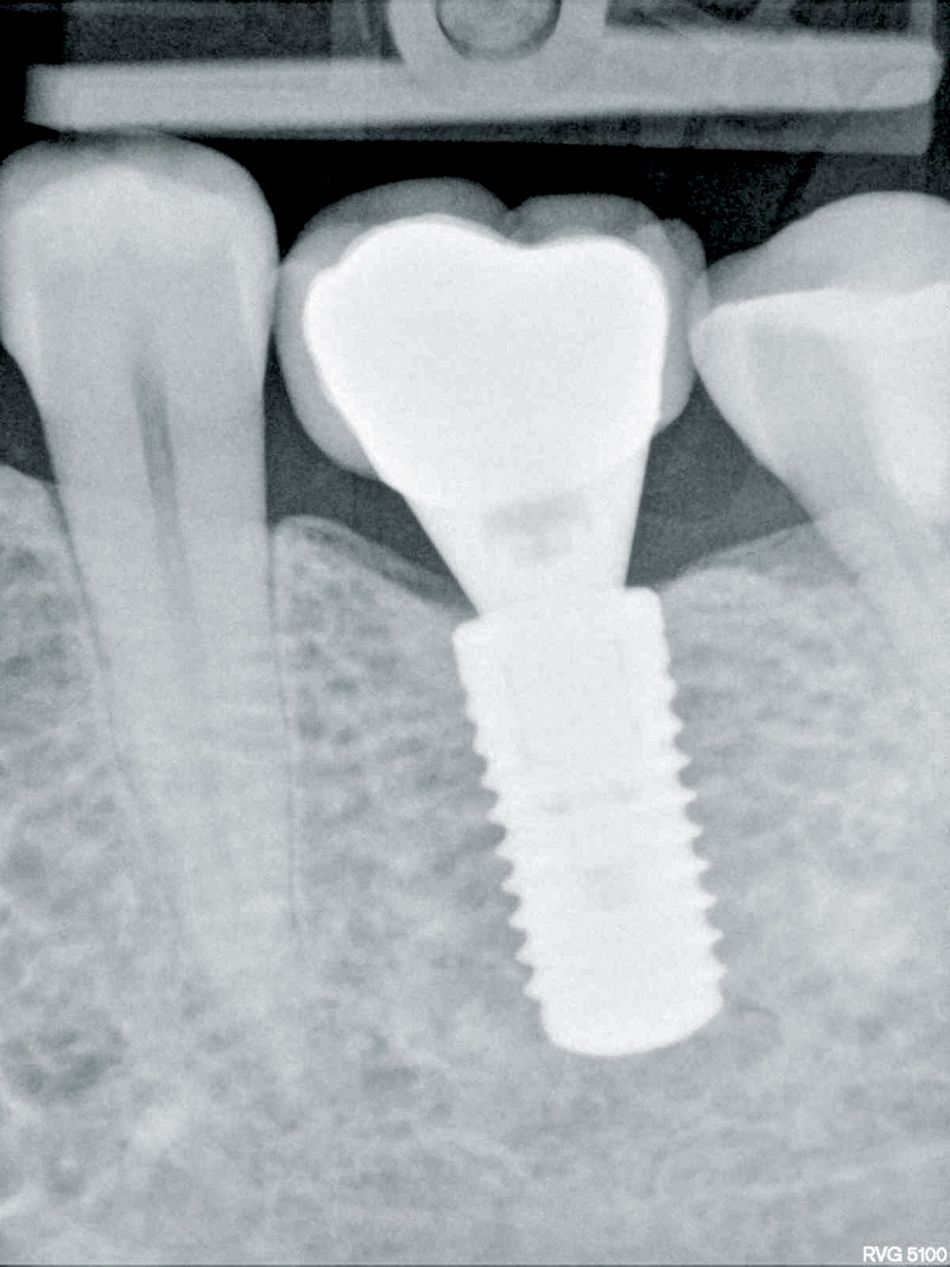
After local anesthesia, a crestal incision in region 3.6 and a sulcular incision from 3.5 to 3.7 were performed and a full-thickness flap was raised. A vertical thickness of the mucosal tissue of 2 mm was measured with a periodontal probe (Fig. 3), indicating the augmentation of the peri-implant mucosa. The bone was prepared and a Straumann® Bone Level Implant (Regular Neck , ∅ 4.8 10 mm, SLActive®) was placed (Figs. 4, 5). After implant placement, the crestal bone around the implant was contoured using a straight hand piece with round bur, and the healing cap was screwed down. The botiss mucoderm® collagen matrix was rehydrated in sterile saline for about 10 minutes to ensure a sufficient flexibility of the graft, and then perforated. After that, the matrix was pulled over the healing cap and placed in direct contact with the bone (Fig. 6). Finally, the margins of the flap were adapted and sutured with Assucryl 4/0, leaving the healing abutment open (Fig. 7).