Introduction
This clinical case represents a three-dimensional bone regeneration of an atrophic tooth in the molar region. The hopeless tooth was extracted, and an immediate implant placement was performed. During implant placement, the novel resorbable magnesium metal NOVAMag® membrane was applied to regenerate the missing buccal bone wall. The fully resorbable magnesium membrane was cut to fit the morphology of the defect and was placed between the periosteum and the bone without fixation.
Initial situation
A systemically healthy 49-year-old male patient came to our clinic complaining of pain and swelling in the right mandibular region. He reported being a non smoker with no medication or allergies. His dental history revealed an endodontic treatment to the right lower first molar due to an advanced carious lesion 5 years ago. He was afraid of losing his tooth. Therefore, his main request entailed an esthetic, safe, predictable, and minimally invasive solution to his problem. The intraoral examination revealed an ovoid elevation of gingiva on the lateral aspect of the root and suppuration on probing, with a pathological probing depth on the lower right first molar #46 (Fig. 1).
The radiographic assessments were performed; the intraoral radiograph showed a periapical lesion on the tooth (previously treated endodontically), and the CBCT revealed a buccal bone dehiscence (Figs. 2,3).
Treatment planning
It was determined that immediate implant placement with bone augmentation would be the course of therapy that met all of the patient's needs.
As a result, the treatment process comprised:
- Pre/extractive interradicular implant bed preparation
- Atraumatic tooth extraction
- Immediate placement of a ø4.3 mm, 11.5 mm long implant
- Augmentation of the post-extraction socket with Cerabone® Plus, NOVAMag® membrane, and a connective tissue graft
- Final impression
- Fabrication of a customized healing abutment
- Final restoration delivery after 3 months.
Surgical procedure
The region of tooth 46 was anesthetized with local infiltration anesthesia (articaine 2% with epinephrine 1:100,000).
The alveolus, according to the Ellian classification in 2007, was classified as a Type 2 socket, where the soft tissue was present, but a dehiscence bony defect existed.
The first molar was decoronated using a Lindemann bur at the level of the gingival margin.
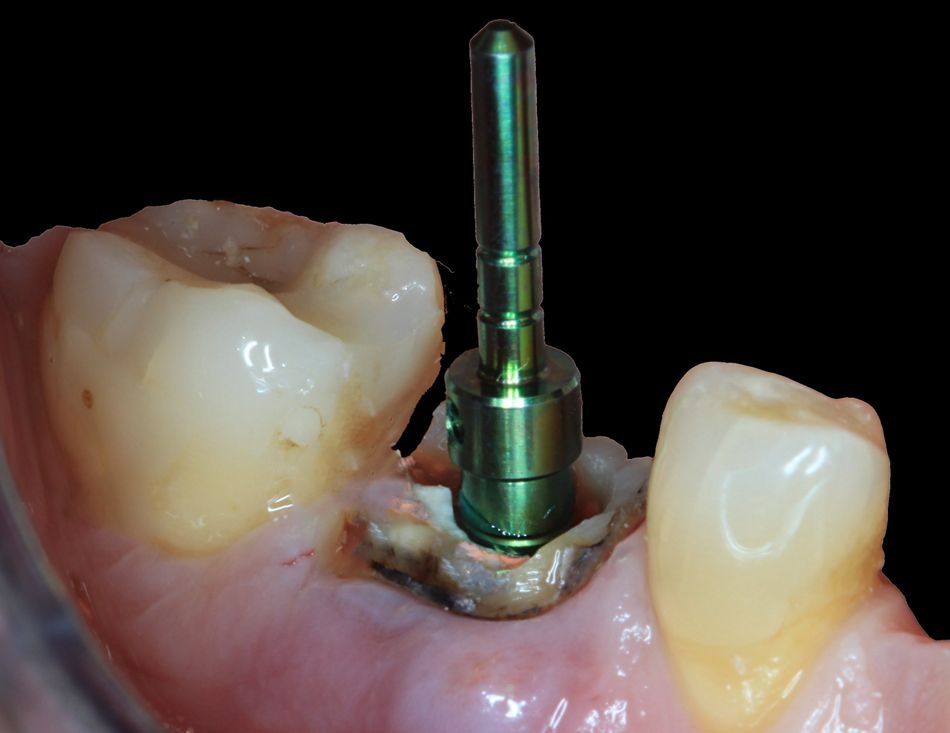
Subsequently, and without any flap elevation, the osteotomies were performed directly through the tooth's initially retained root complex, pre-extractive interradicular implant bed preparation (Fig. 4).
The osteotomy drills were guided by the retained root features, which also made it possible to precisely position and angle the implant bed preparation in relation to the tooth's emerging profile. The drilling procedure was completed in accordance with the manufacturer's instructions .
The residual root components were meticulously removed using clamps and desmotomes.
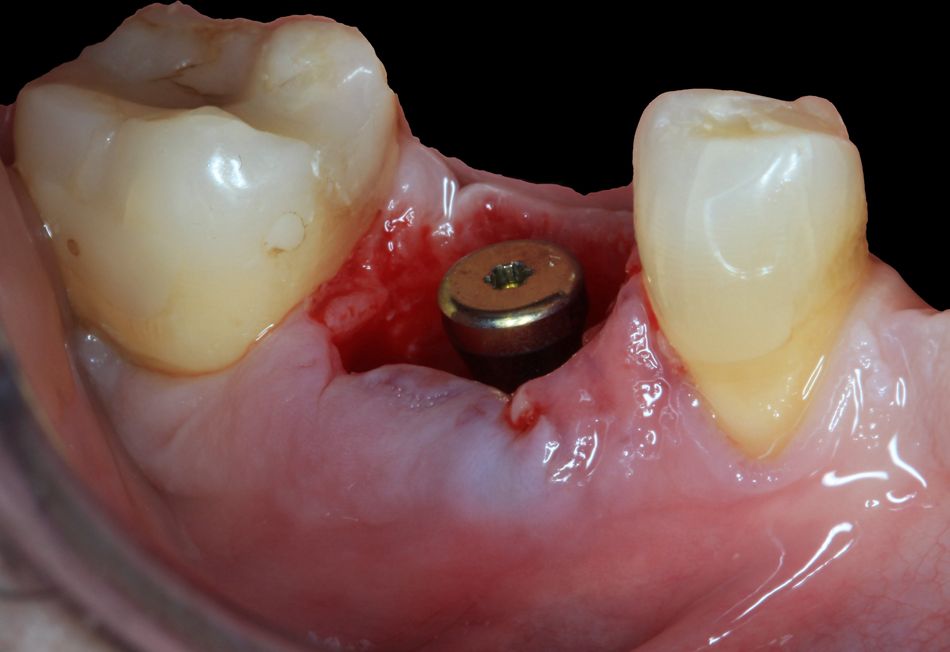
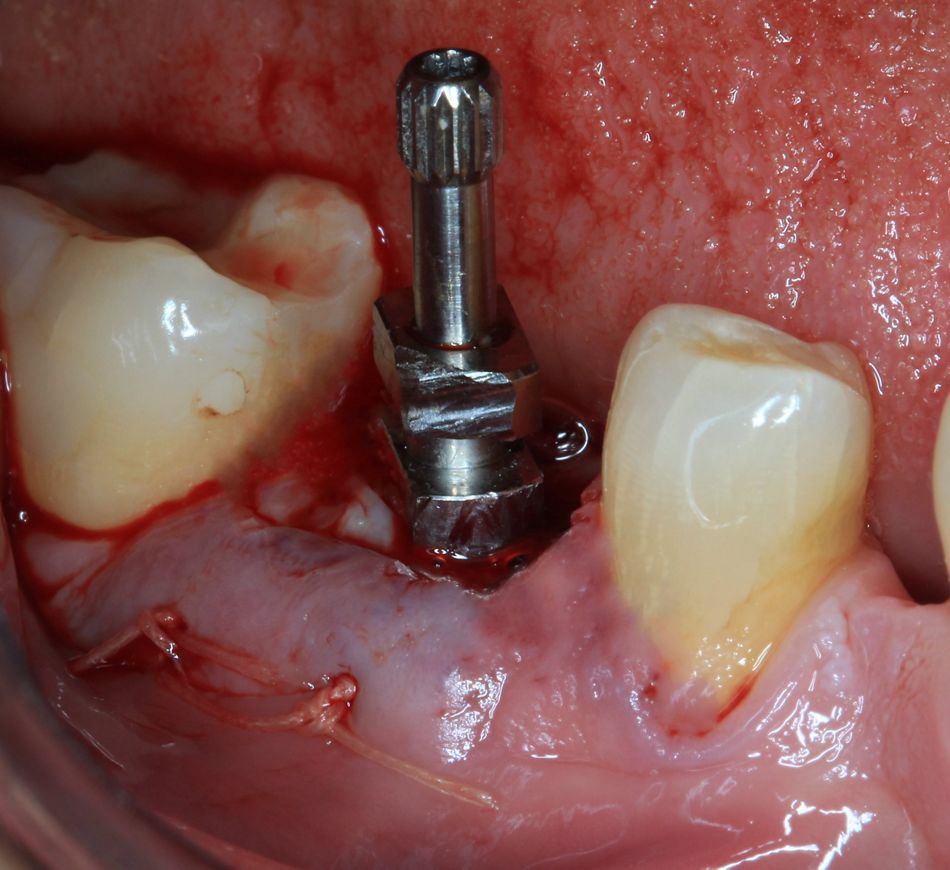
The extraction socket was thoroughly curetted and rinsed with chlorhexidine 0.20%, and a tapered implant was inserted as described by Hürzeler in 2013 (Fig. 5).
The implant shoulder was located at 3.5 mm to the facial free gingival margin. Primary stability was obtained and confirmed with hand torque (minimum of 35 Ncm) to facilitate immediate custom-healing abutments.
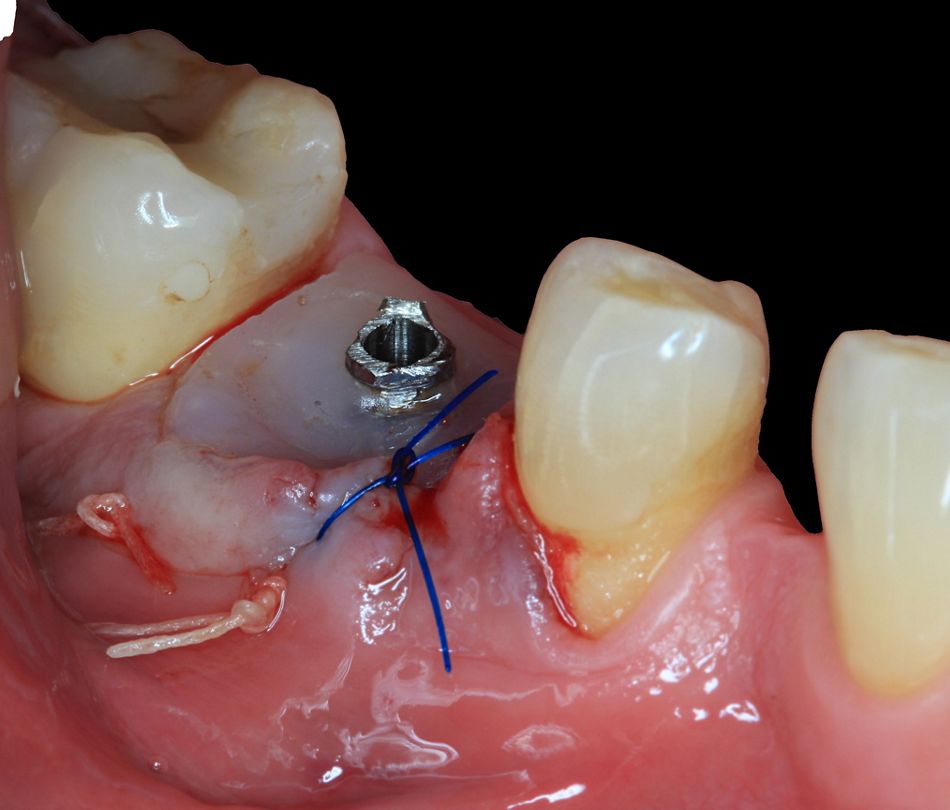
The NOVAMag® membrane was trimmed and contoured, conforming to the size and shape of the labial bone deficiency previously assessed. The membrane was then tucked between the bone and soft tissue without requiring any fixation (Fig. 6).
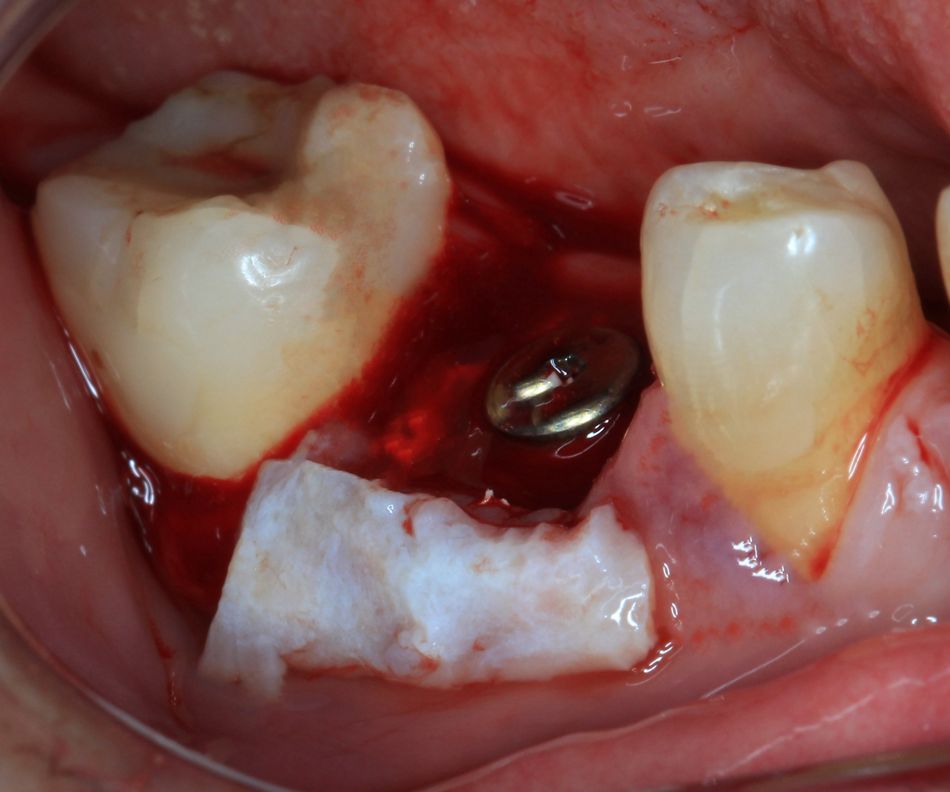
According to the findings of a study on soft tissue augmentation surrounding implants by Stefanini 2023, surgical sites undergoing soft tissue augmentation usually maintain their marginal bone levels and soft tissue margins over time. A graft of subepithelial connective tissue was performed, removed from the palate, and positioned on the recipient area by tunneling the peri-implant tissues on the buccal side (Fig. 7).
A healing abutment was temporarily placed to occlude the screw access hole of the implant during grafting, preventing xenograft particles from entering the implant. Following the manufacturer’s instructions, 1.0 mL cerabone® plus (Botiss) was mixed with autogenous bone (1:1 ratio) to increase the space between the granules and hydrated with 0.5 mL saline until a sticky ball was obtained. The patient was instructed to rinse with a 0.12% chlorhexidine solution twice daily for the next two weeks. The sutures were removed two weeks after the surgery, and control visits were performed after 4 and 8 weeks.
At 7 days, the magnesium membrane experienced an inflammatory response, but this quickly decreased, and after 14 days the inflammatory response was comparable to that of the collagen membrane, as described by Kačarević in 2023.
Prosthetic procedure
Using a polyester impression material with impression post for an implant-level impression, we obtained complete upper and lower arch impressions for the final crown immediately after implant insertion (Fig. 8).
Screw-retained customized healing abutments were fabricated using titanium temporary cylinders ( and autopolymerizing acrylic resin (Fig. 9).
The customized healing abutments were steam-cleaned and inserted using hand torque. Adequate support of the soft tissues and gingival architecture was ensured immediately postoperatively.
According to Chu in 2014, the customized healing abutments possessed the subgingival contours that conform to the pre-extraction state of the tooth root cervix to support the soft-tissue emergence profile and help protect the blood clot and contain the bone graft particles.
The final monolithic zirconia crown (by Saletta MDT) was fabricated in the laboratory.
Twelve weeks after the implant placement, the crown was seated and tightened to 20 Ncm in accordance with the manufacturer's instructions (Fig. 10).
Final results
At 16 weeks, examination revealed a clinically healthy tissue with no bleeding on probing (BOP).
Radiographic examination showed the presence of marginal bone levels coronal to the implant-abutment junction and the absence of peri-implant radiolucency (Fig. 11).
The CBCT, after 4 months of final prosthesis delivery, revealed complete formation of the buccal bone plate (Fig. 12).
Conclusion
Bone tissue regeneration has been demonstrated by the NOVAMag® magnesium membrane shield approach. The new bone has developed a thick layer of cortical bone.