Early developments
Zygomatic implants were first introduced by Per-Ingvar Brånemark in 1998 for maxillectomy patients and later adapted for edentulous patients with severely atrophied maxillae1.
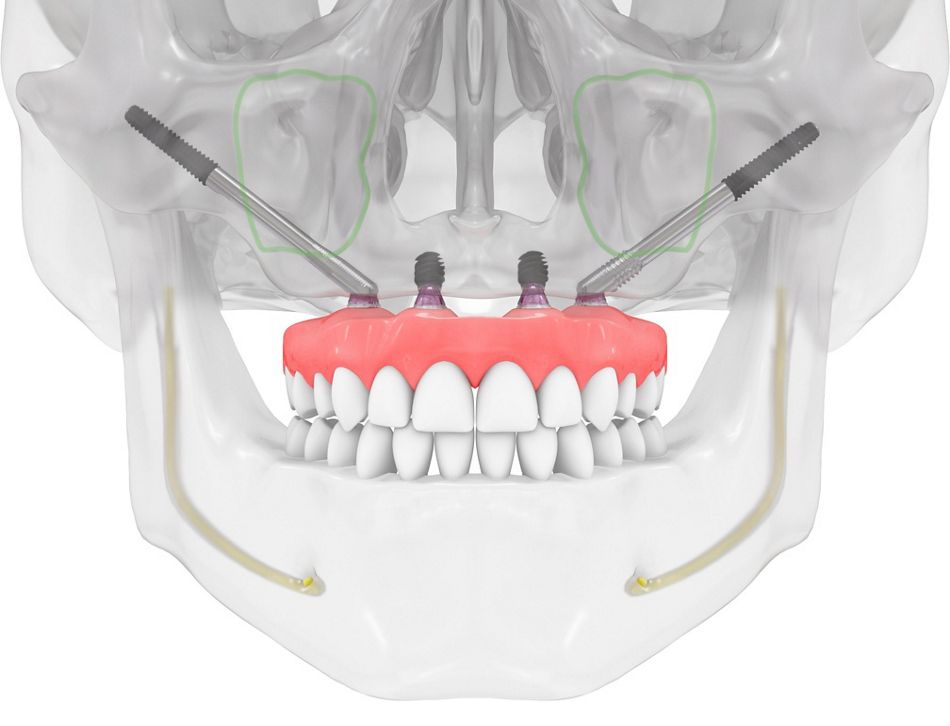
Placement methodologies evolved to the concept of 2 posterior zygomatic implants (one in each quadrant) and the "quad zygoma" approach with four zygomatic implants (two for each quadrant)t, allowing loading within 24 hours. Early studies by Brånemark et al. showed a 96% rehabilitation rate with 52 implants in 28 patients over at least 5 years. However, despite success, complications like rhinosinusitis and soft-tissue infections were common2. To reduce invasiveness, Stella and Warner proposed the “slot technique” in 2000, using a crestal entry to eradicate the problem of bulky prostheses3. In 2006, Migliorança et al. reported outcomes of 150 externally positioned zygomatic implants in 75 patients, reducing rhinosinusitis risk4. Aparicio’s group later proposed an exteriorized implant pathway to avoid sinus perforation5, though buccal soft tissue recession was observed6. In an extension of other studies, Malo et al. introduced a modified extra-maxillary technique, requiring alveolar ridge contouring, which sometimes caused sinus infections7. This led Aparicio to introduce and describe the anatomically guided ZAGA approach in 2011 following his long-term experiences with similar complications while placing zygomatic implants in patients with severe atrophy8.
Patient’s anatomy first, the ZAGAclassification
The zygomatic anatomically guided approach (ZAGA) is an evolution of the above methods devised to provide patients with long-term, complication-free, predictable implant solutions, whatever their anatomical situation8. The rationale is that patients present with differing anatomical variations, and even site variations, within the same patient. Hence, the need to have an adaptable solution rather than a one-size-fits-all protocol is paramount. Treatments can be intra-, extrasinus, or a combination of both. Aparicio developed an anatomical evaluation process known as ZAGA classification to aid the right treatment protocols in any given situation. Initially, in a cross-sectional survey9 based on 200 sites across 100 patients, he identified and classified five anatomical pathway situations as ZAGA 0-4. Classifications range from ZAGA 0 (straight lateral maxillary wall with the implant platform on the crest and the middle portion inside the sinus) to ZAGA 4 (extreme resorption of the maxillary sinus with or without significant concavity of the lateral sinus wall). This allowed for a better understanding of the shape of the maxillary wall and how it would predetermine the implant pathway9.
Such classification aims to provide the right prosthetically driven implant pathway to prevent long-term complications. The implant path is studied to achieve this aim, and three key areas are defined: the anchor zone, the antrostomy zone, and the zygomatic implant critical zone (ZICZ). As a result, everything from the initial incision and the implant path to the closing of the soft tissue is individually tailored, depending upon the classification of the patient. The classifications were identified as ZAGA 0-4 and would later be branded with an “A” or a “P” to determine anterior or posterior atrophy.