Introduction
The RevEX™ scanbody, characterized by its digital and user-friendly design, significantly streamlines the process of acquiring accurate digital impressions. These impressions are critical for the fabrication of precise prostheses. The implementation of the RevEX™ scanbody can reduce the number of patient visits by approximately 40%, positioning it as a key component in a fully digital workflow for final full-arch restorations.
This case report describes the application of the RevEX™ protocol within a complete digital workflow for double full-arch FP1 and FP3 zirconia prostheses. It aims to demonstrate the clinical efficacy of the RevEX™ scanbody, emphasizing its role in reducing chair time, enhancing patient comfort, and improving the precision of prosthetic outcomes. The adoption of this protocol represents a significant advancement in full-arch rehabilitation, offering substantial benefits to both practitioners and patients.
Through the clinical outcomes, treatment workflow, and patient feedback, this clinical case report highlights the potential of the RevEX™ scanbody in modern dental practice. The integration of this innovation optimizes the prosthetic workflow and sets a new benchmark for digital dentistry, encouraging future advancements in patient care.
Initial situation
A 43-year-old healthy male (ASA I), a non-smoker with no current medications or known allergies, presented to our clinic with existing complete dentures seeking rehabilitation with dental implants. A comprehensive diagnostic work-up was conducted, including intraoral, extraoral, and radiographic examinations, along with photographic, video, and scan records. Parameters such as vertical dimension of occlusion, maxillomandibular relationship, midline, incisal edge position, esthetics, phonetics, function were evaluated (Fig. 1). The patient presented an Angle Class II skeletal relationship. The existing complete dentures were deemed acceptable.
Treatment planning
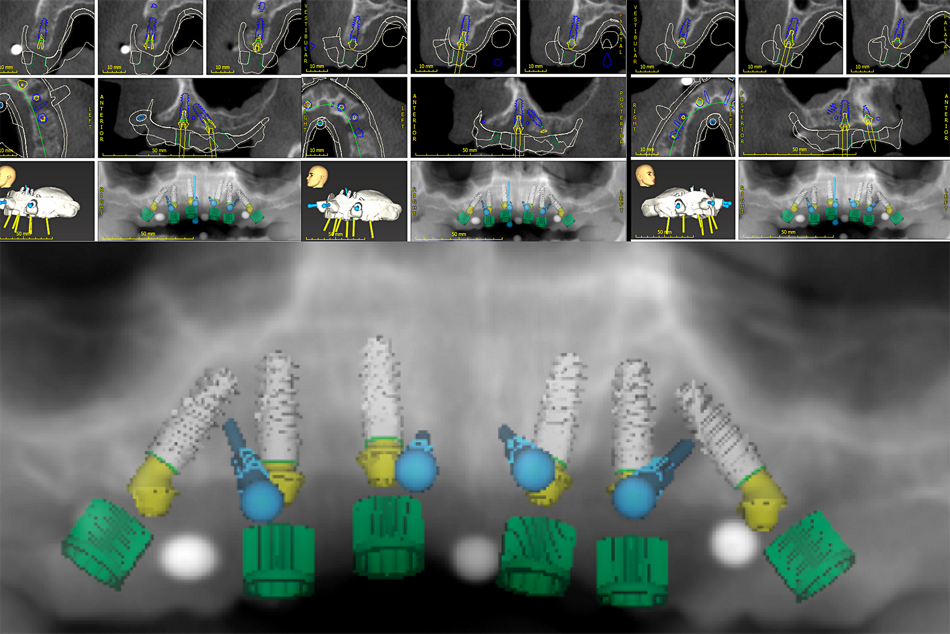
Treatment options were discussed, and the patient opted for double complete-arch implant rehabilitation. Based on diagnostic data acquisition, Full-Arch FP1 for the upper jaw and FP3 Zirconia Prostheses for the lower jaw were envisioned. A digital workflow was employed to plan, design, and execute computer-guided surgery, as well as the conversion of prefabricated interim prostheses for the immediate fixed rehabilitation using the RevEX™ protocol.
The treatment workflow included:
1. Digital implant planning and design (Fig. 2).
2. Mandible:
• Use of Smile in a Box®.
• Flap approach with simultaneous implant and bone grafting.
• Guided surgery using Straumann® BLX implants.
3. Maxilla:
• Use of Smile in a Box®.
• Flapless approach.
• Guided surgery using Straumann® BLX implants.
4. Passive fit of conversion (provisional) prostheses.
5. RevEX™ Protocol
First appointment: using an intraoral scanner (TRIOS® 3, 3Shape A/S, Copenhagen, Denmark)
• Intraoral scanning of the conversion prostheses and occlusion.
• Intraoral scanning of the maxillary and mandibular soft tissues.
• Extraoral scanning using RevEX™ with the reverse scanning technique.
Second appointment:
• Milled prototype and verification jig try-in. Third appointment:
• Delivery of the final zirconia prosthetic rehabilitation.
6. Follow-ups: maintenance program
Surgical procedure
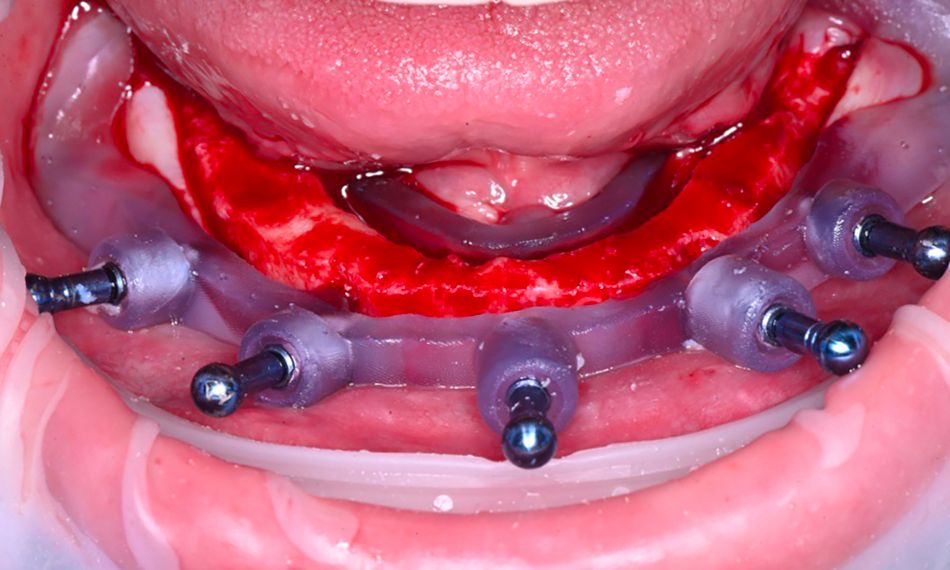
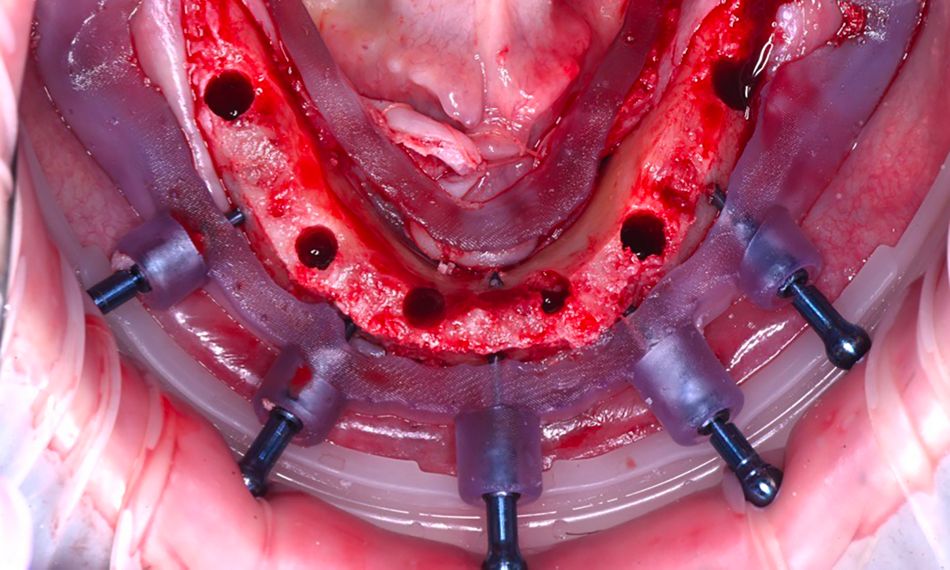
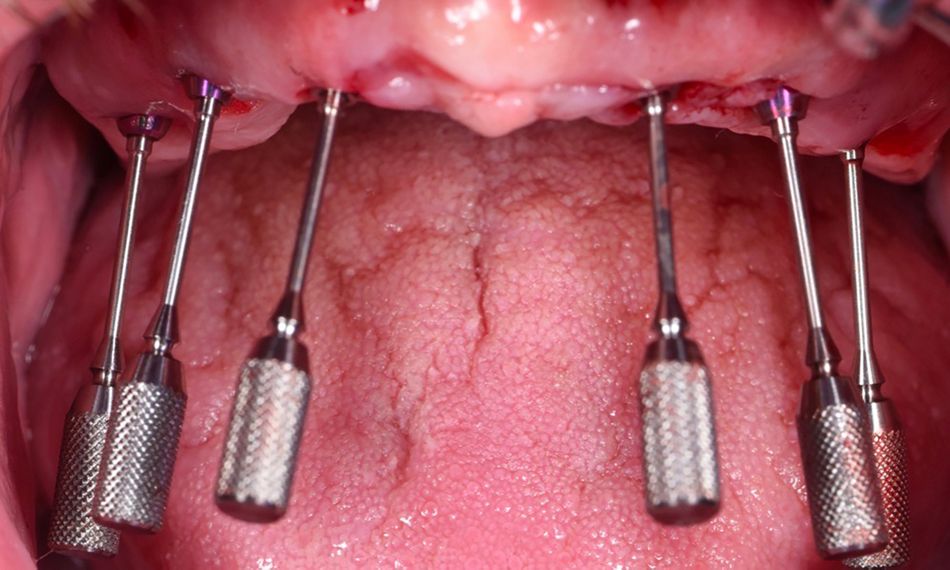
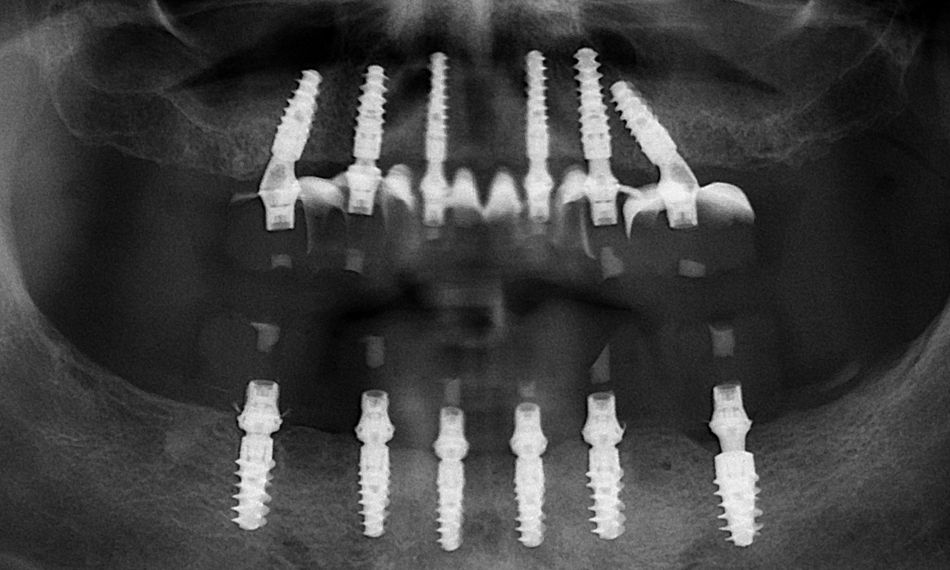
The patient received an inferior alveolar nerve block as well as local anesthesia with 2% lidocaine and 1:100k epinephrine. The mandibular jaw was treated first using the stackable guide concept (Smile in a Box®, Institut Straumann AG, Basel, Switzerland). A mucoperiosteal flap with a crestal incision was raised. The surgical guide was fixed, bone reduction was performed, and six dental implants were placed (Straumann® BLX implant, ∅4.0 mm RB, SLActive® 12 mm Roxolid®) with high primary stability exceeding 45 Ncm. Following this, 2.5 mm Straumann® Screw-retained Abutments (SRA) were inserted and torqued to 35 Ncm. Temporary abutments were fitted, rubber dam isolation was carried out and the temporary abutments were subsequently picked up with the prefabricated interim prosthesis (conversion prosthesis technique) with PMMA resin. The implants were immediately loaded with the prefabricated interim prosthesis (Figs. 3-6). A radiograph was taken for control. Occlusion, esthetics, phonetics, and vertical dimension of occlusion (VDO) were checked, and hygiene instructions were provided. Follow-up appointments were scheduled.
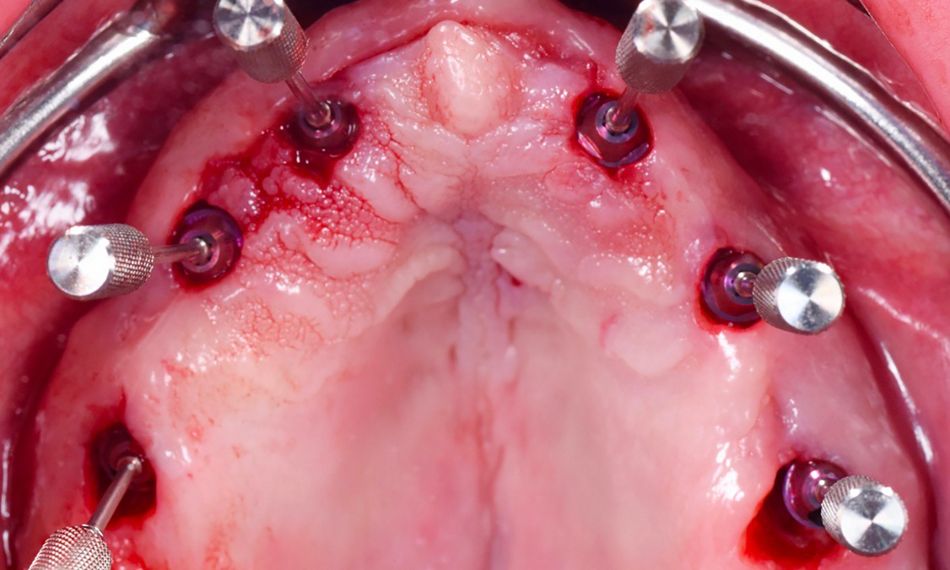
After six weeks of healing, the maxillary jaw was treated with the same approach as the mandible (Figs. 7-10).
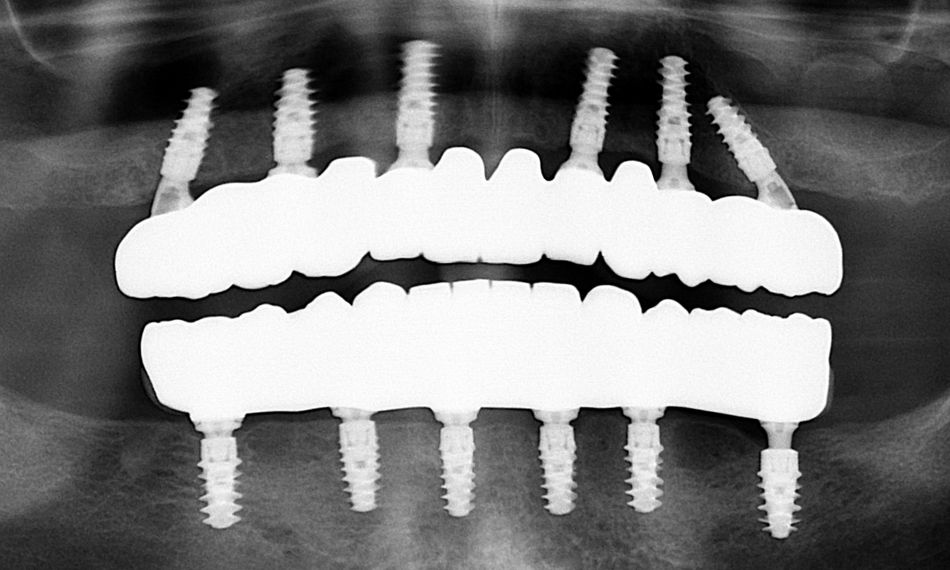
Following an uneventful healing period of three months, the patient returned for assessment of osseointegration. The conversion prostheses were removed, the straight and angled multi-unit abutments (SRA, Institut Straumann AG, Basel, Switzerland) were torque tested, and the interim prostheses were evaluated for proper fit clinically, visually, and radiographically (Figs. 11-12).
Prosthetic procedure
After scalloping and contouring certain areas, selective pressure was applied to the alveoli, resulting in an optimal contour (Fig. 13). The conversion interim prostheses were passively fitting and were additionally assessed for appropriate esthetics, phonetics, and vertical dimension of occlusion. It is crucial to ensure the passive fit of the temporary restoration before it can be used with the RevEX™ workflow. All aspects were found to be adequate, allowing the progression to the final restorative phase.
The final restorative phase was completed in three appointments with the RevEX™ workflow.
At the first clinical appointment, the extraoral reverse scanning technique was used for the digital acquisition of the implant positions to allow fabrication of prototype prostheses. A series of three sets of digital scans with an IOS (TRIOS® 4, 3Shape A/S, Copenhagen, Denmark) were taken with a previously published protocol.
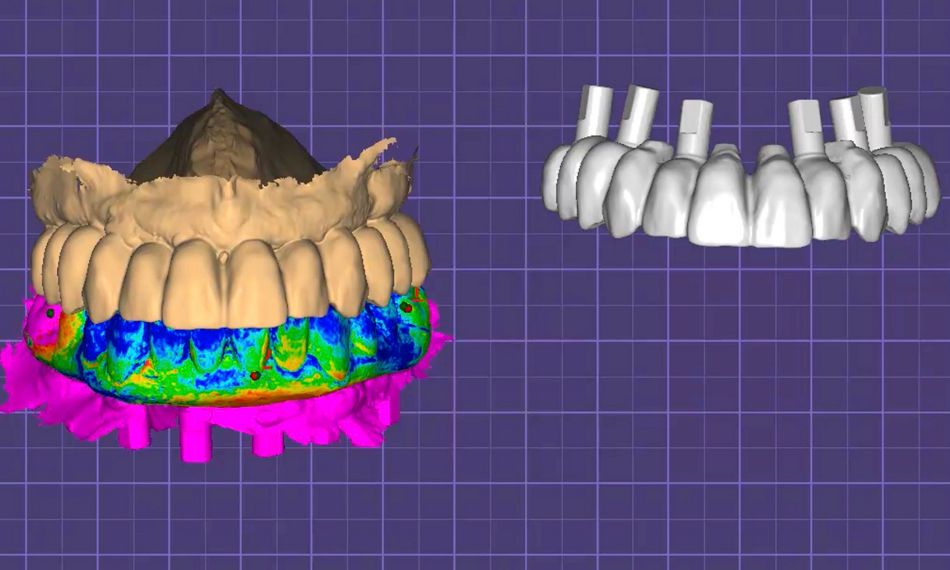
The first set of scans were recorded using OptraGate and a retractor, and included scanning of the conversion prostheses intraorally, with occlusal, palatal/lingual and buccal views, and the patient’s occlusion, to obtain the tooth position, maxillomandibular relationship and vertical dimension that had been established and verified for the patient.
Subsequently, the conversion prostheses were removed, and a second set of scans was taken that included only the maxillary and the mandibular soft tissues of the edentulous jaws with the screw-retained abutments in place, to obtain the soft tissue morphology to aid the technician in designing hygienic, yet intimate, intaglio contours of the prototype prostheses and, later on, the definitive prostheses.
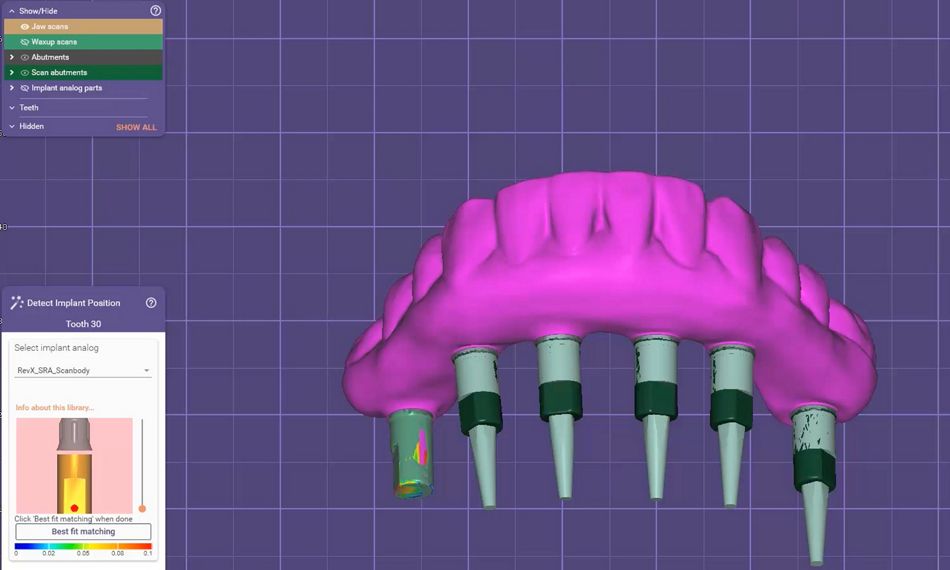
Finally, a third set of scans was recorded extraorally with the reverse scanning technique. Reverse scanbodies (Straumann® RevEX™ Scanbody) were attached to the conversion prostheses and they were digitally scanned extraorally with the same IOS, to obtain the 3D implant positions (Figs. 14-15).
The three sets of scans were then imported into a computer-aided design (CAD) software (exocad DentalCAD, Exocad GmbH, Darmstadt, Germany), and aligned to one another to digitally articulate and cross mount the STL files. An implant library for the reverse scanbodies was used to inform the software about what implants were used and allow for the connection of the prostheses to receive the respective titanium bases. A digital technique was used for a CAD/CAM verification jig from the IOS data, to verify that the STL file of the implant positions was accurately captured (Figs. 16,17).
At the second clinical appointment, the CAD/CAM milled verification jigs, which were previously digitally designed, were tried-in to confirm successful complete and passive seating (Figs. 18,19). Next, milled prototype prostheses were tried-in, and fit was assessed clinically by the screw resistance test. The prototype prostheses were evaluated to confirm the desired design, esthetics, phonetics, and occlusion. Minor esthetic adjustments were made. The patient’s ability to access the intaglio surface of the prosthesis for adequate hygiene was confirmed prior to completing the definitive prostheses (Fig. 20).
After they were deemed adequate, the STL files were sent to the lab, where the technician designed and fabricated the maxillary and mandibular screw-retained definitive zirconia prostheses. The zirconia was cemented to titanium bases for the screw-retained prostheses (Figs. 21,22).
At the third clinical appointment, the screw-retained definitive zirconia prostheses were delivered and torqued (Figs. 23,24).
At the 1-year follow-up, the patient was very satisfied with the function and esthetics of the rehabilitation (Fig. 25)
Treatment outcomes
The patient was regularly monitored over a 1-year follow-up period. Clinical and radiographic assessments indicated stable peri-implant conditions, with no evidence of inflammation or bone loss. The patient expressed high satisfaction with both the functional and esthetic results of the treatment at the 1-year follow-up.
Author’s testimonial
“Extraoral scanning with the novel Straumann® RevEX™ is a game changer. It facilitates a complete digital full-arch workflow in a precise and efficient manner.”
Learn more about Straumann RevEX® here: