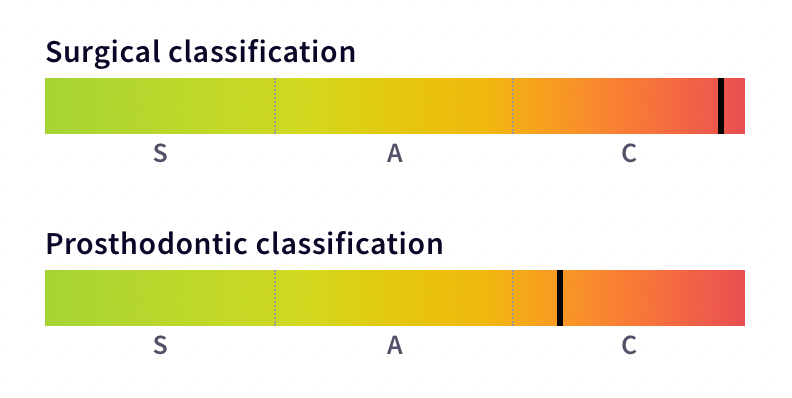
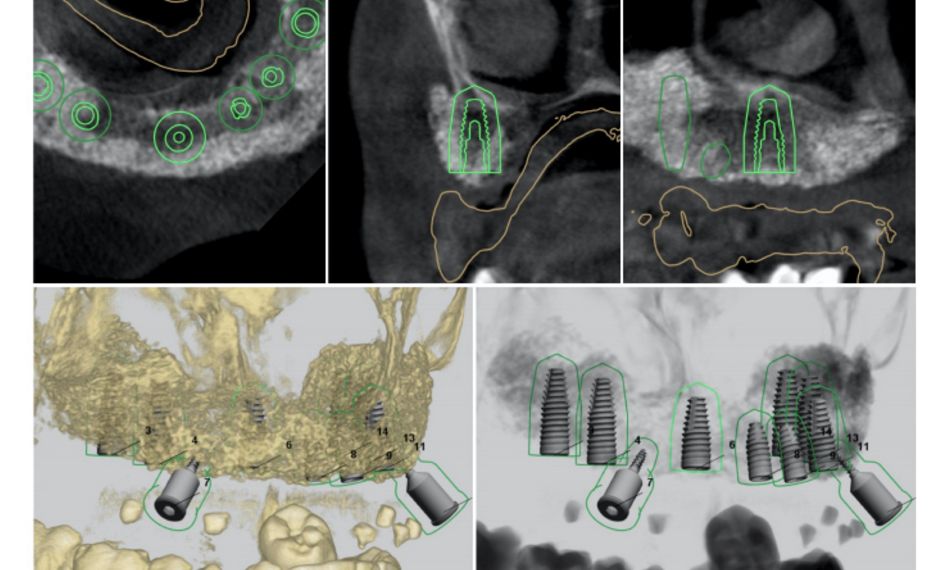
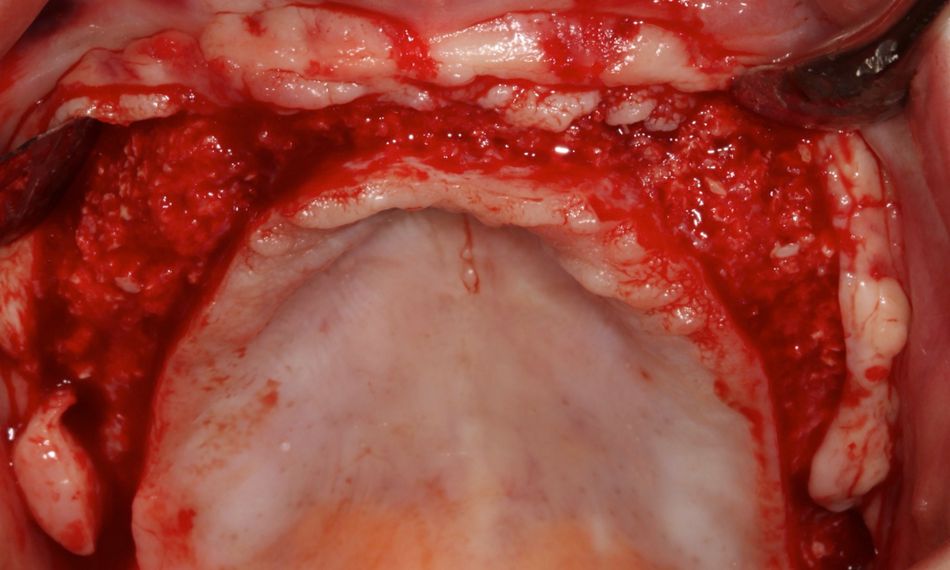
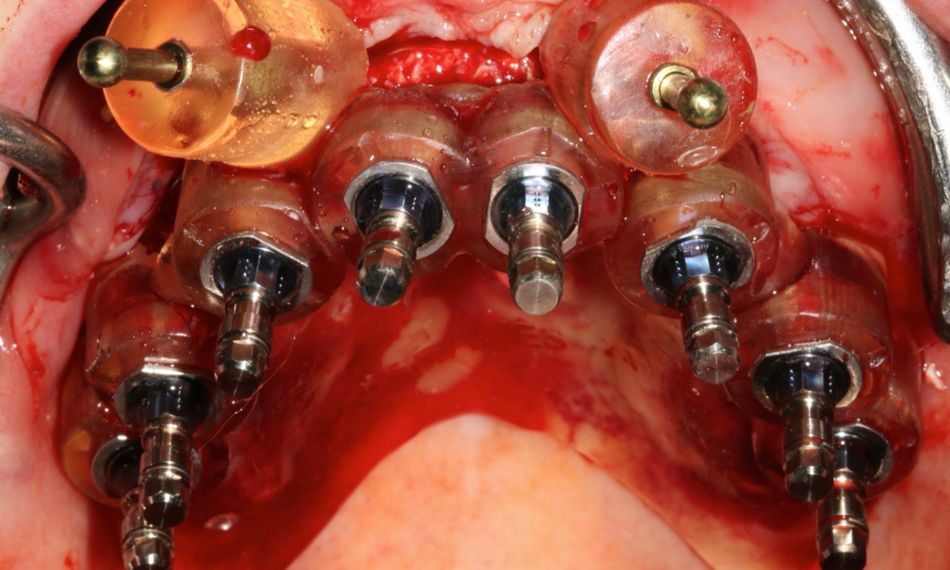
The treatment plan focused on restoring function and esthetics through a combination of bone augmentation, sinus lift, and implant placement using Straumann® Bone Level Tapered (BLT) implants. The surgical workflow included the use of Straumann® Xenograft for ridge augmentation, followed by digital planning for guided implant surgery. A temporary removable denture was provided during the healing phase, after which the patient received a screw-retained monolithic zirconia prosthesis.
Beyond the clinical success of the procedure, the impact on the patient’s quality of life was evident. Prior to treatment, the patient reported considerable difficulties with masticatory function, poor nutrition, and a decline in self-esteem due to the limitations of removable dentures. Following the full-arch rehabilitation, the patient experienced marked improvements in oral function, esthetics, and psychosocial well-being. This case highlights the critical role played by implant-supported restorations in not only addressing dental health issues, but also enhancing overall patient satisfaction and quality of life.
Initial situation
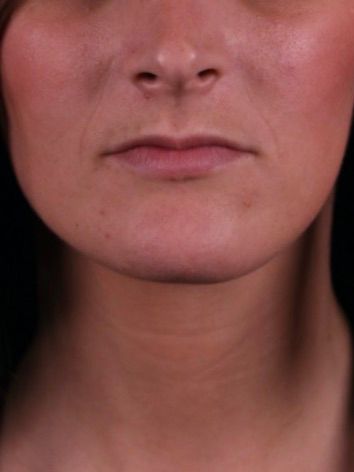
A 20-year-old woman came to our clinic in good health, not taking any medication, and with no allergies. She told us that she had lost her teeth at a young age because of cavities. Although she had tried implants before, the treatment did not work out, and she could not imagine wearing removable dentures for the rest of her life. She wanted to find a fixed solution using dental implants to restore her failing teeth. The extraoral examination showed a flattening of the lower third of the face, attributed to the lack of support from the missing maxillary teeth (Figs. 1-4).
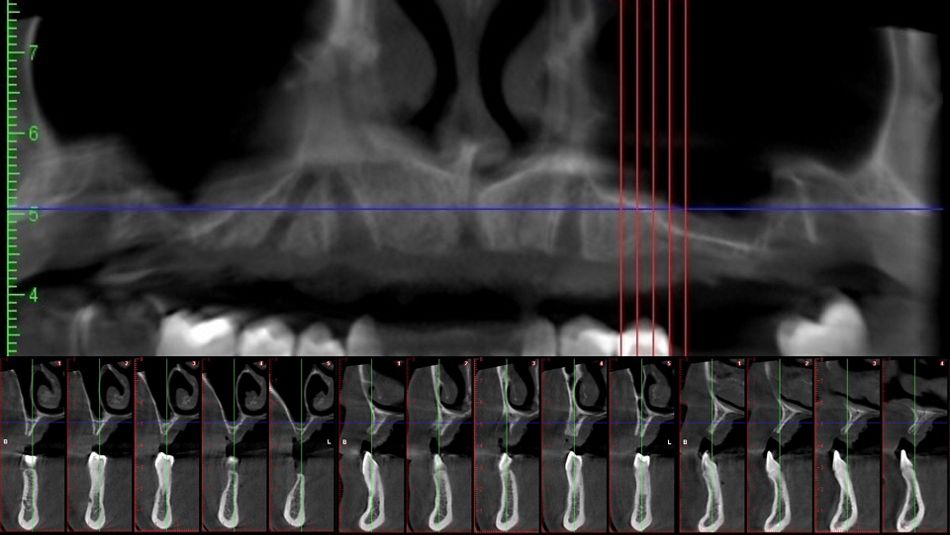
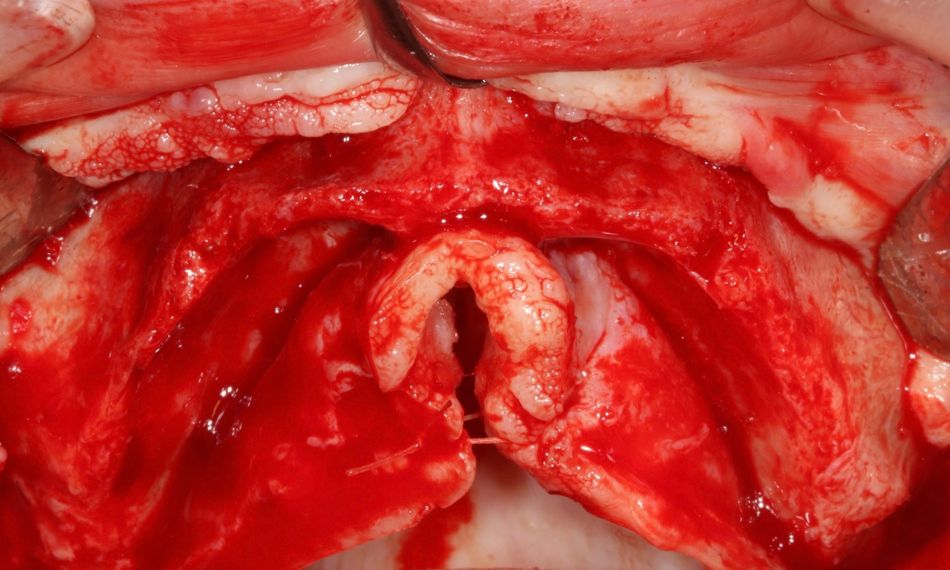
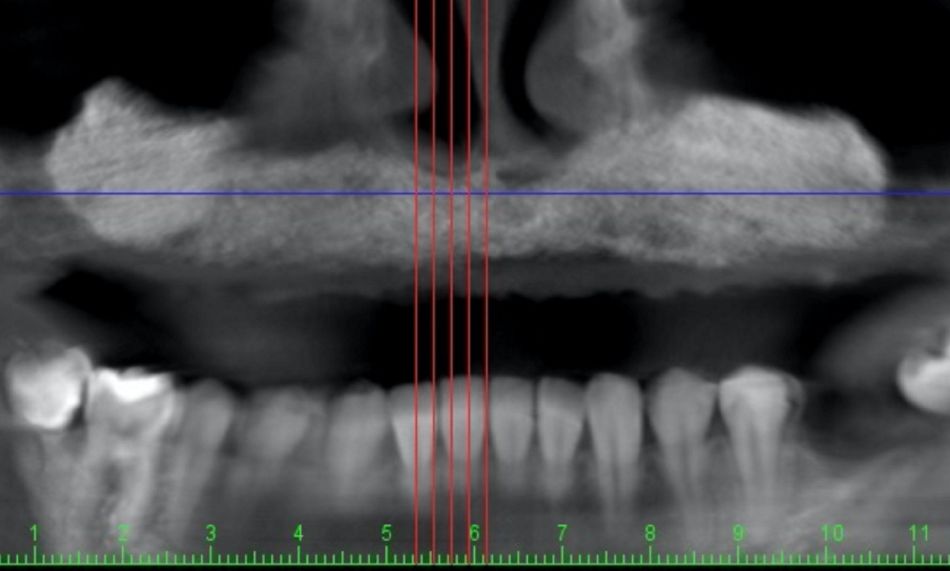
The intraoral examination revealed an edentulous maxilla characterized by significant horizontal and vertical bone resorption. This considerable loss of bone structure presents substantial challenges for implant placement, as it may compromise the necessary stability and support for a successful prosthesis.
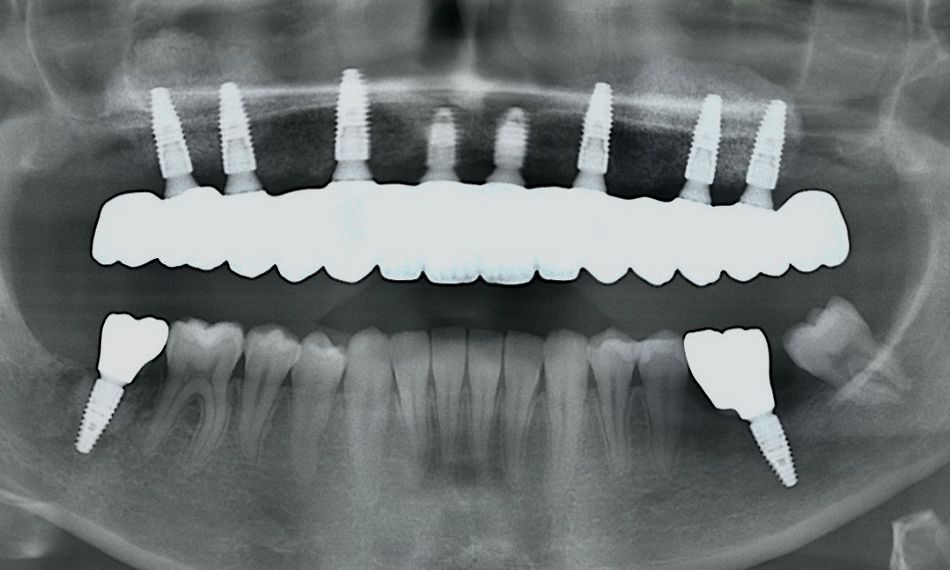
Additionally, the radiographic examination confirmed recent implant loss and demonstrated a critical deficiency of bone in both vertical and horizontal dimensions (Fig. 5). This imaging underscores the necessity for thorough evaluation and intervention to address the underlying bone deficiencies, highlighting the urgent need for a comprehensive treatment plan to effectively restore both function and esthetics.