Evolution of dental implant prosthetic concepts
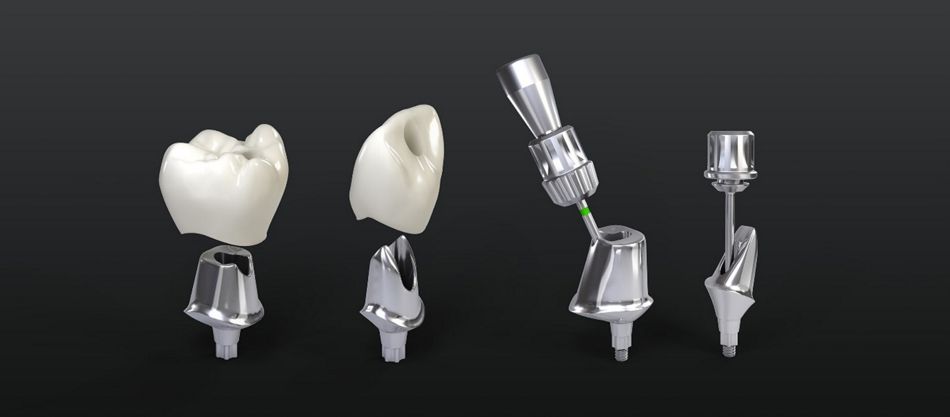
Dental implant prosthetic designs and materials have significantly evolved over the last two decades, delivering lifelike, stable, and efficient tooth rehabilitation. Implant-supported fixed prostheses can be screw-retained utilizing an abutment, cement-retained directly to the implant body, or both. Early concepts of implant-supported prostheses were screw-retained as per the ad-modem Branemark protocol in 1981 (Adell R et al., 1981). Alternatively, cemented prostheses were considered less technically challenging and by the early 2000s, became more popular, incorporating the use of both provisional (temporary) and definitive cement for the retention of the crowns/bridges to the implant (Pasqualini U et al., 2009). The latest advancements in both dental materials and digital workflows have reduced costs and enhanced the ease of design, fabrication and usability of both types of prostheses. (Sarafidou K et al., 2023). Both screw and cement-retained prostheses can be applied to single, multiple, or cross-arch fixed implant restorations. However, the introduction of angulated screw channels substantially enhanced their clinical applicability of screw-retained prostheses. It improved esthetics and functional stability in challenging cases while preserving the advantages of retrievability, ease of maintenance, and reduced cement-related complications.
When, where, and why
Several clinical and technical factors should be considered when choosing the type of prosthetic retention. These include but are not limited to, implant position in the arch, available interocclusal space, retention requirements, esthetic expectations, potential complications, and treatment costs. Numerous systematic reviews, clinical trials, and case studies examined the pros and cons of each approach, emphasizing the need for an objective understanding of these factors in treatment planning. (Wismeijer D, et al., 2014) Screw-retained prostheses offer several advantages over cement-retained options, particularly regarding retrievability, maintenance, and durability in both posterior and anterior regions. Their secure connection reduces complications from residual cement and enhances long-term maintenance. Unlike cement-retained restorations, which rely on principles from natural tooth prosthodontics, such as abutment taper, surface area, height, and roughness, screw retention does not depend on these specific features for stability. Research indicates that cement-retained restorations often have subgingival margins positioned 2-3 mm below the gingiva. However, this approach can complicate maintenance and increase the risk of residual cement, potentially leading to inflammation and peri-implantitis. In contrast, screw-retained options avoid the need for abutment taper or height, making them a reliable choice when interocclusal space is limited, or implants are misaligned, where achieving cement retention is challenging. (Wittneben JG, et al., 2017, Jørgensen KD 1955, Strong SM 2008) Screw-retained restorations can be reliably placed with as little as 4 mm of space between the implant fixture and the opposing dentition. This approach can eliminate the need for pre-prosthetic surgery or invasive restorative procedures to increase restorative space (Wittneben JG, et al., 2017). In cases of limited interocclusal space due to misaligned implants, screw-retained restorations are preferred over cement-retained ones.
Learn more or buy products
Straumann® Angled Solutions (AS): Flexibility and precision from a different angle. Expanded options for screw-retained restorations. Click here
Straumann e-Shop: The quickest way to search, find and purchase the right products across the Straumann Group brands, and all in a single checkout. Click here
Innovations in screw-retained restorations: angulated screw channels (ASCs)
Though studies suggest that larger screw access holes can occupy a significant part of the occlusal surface (Hebel and Gajjar 1997), modern techniques, such as the use of angulated screw channels (ASCs), minimize these issues effectively. ASCs represent a scientifically validated advancement in implant dentistry, enhancing both esthetic outcomes and functional performance. They enable the repositioning of the screw access point within a range of up to 30° from the implant axis in any 360° direction (Rella E et al, 2021). This flexibility is particularly advantageous in anterior regions, where achieving optimal esthetics can be challenging. Therefore, by allowing access from more favorable positions, ASCs integrate restorations more seamlessly within the visual field without compromising functional durability or essential axial loading. By enabling screw-retained restorations, ASCs facilitate retrievability and preserve the axial forces essential for long-term structural integrity.
ASC systems are meticulously engineered with specialized components, including screws and precision screwdrivers that engage at multiple angles. This engineering allows clinicians to apply the necessary torque, even at divergent angles, to ensure the stability and durability of the restoration over time.
The clinical benefits of ASCs are increasingly recognized and applied in a daily clinic. In anterior regions, ASCs support high esthetic standards by offering control over the access point, which improves visual outcomes. In posterior zones, they provide robust functional strength and optimal axial alignment, which are crucial for the longevity and reliability of implant-supported prostheses. Additionally, the adaptability of ASCs minimizes reliance on cement-retained concepts and effectively reduces the risks associated with residual cement, such as peri-implant mucositis and peri-implantitis.
Keep yourself up to date
Straumann Science Newsletter: Keep your finger on the pulse of everything that is happening in the field of implant dentistry. Subscribe
Straumann SKILL: Discover international and regional courses for trainings at all levels. Click here
Managing complications: biological and mechanical considerations
Any type of retention is used, it may be subject to complications, either biological or technical. If not completely removed, the residual cement in cement-retained prostheses can lead to soft tissue inflammation and bone loss. Applying petroleum jelly, using curettes, and flossing during crown cementation can help avoid these issues but may also not completely mitigate them. Screw-retained prostheses face no such issues, though care should be taken to avoid micro gaps between the crown and the implant abutment, which, besides creating the possibility of bacteria infiltration and the development of peri-mucosal inflammation, can also lead to several mechanical issues (Reis INRD et al., 2023). Multiple studies have documented incidence rates ranging from 10% to 65%, depending on the restoration type and study Lee A et al., 2010) While screw loosening and screw fractures remain a primary drawback of screw-retained restorations, the prevalence of this type of complication can, however, be minimized by using the original components.
Research indicates that original prosthetic components significantly outperform non-original or "compatible" alternatives. It was reported that the use of "compatible" abutments that may have compromised internal connections and anti-rotation features could lead to complications and affect long-term stability (Mattheos et al., 2012 & 2015). On the other hand, using original prosthetic components resulted in smaller crown-abutment gaps, reduced screw loosening, and improved fit, thereby enhancing reliability for long-term use (Alonso R et al., 2018). Long-term studies further affirm the reliability of original prosthetic components, reporting on only 1.5-3% of mechanical complications after up to 20 years of function (Wittneben JG et al., 2014, Fischer et al., 2013, Chappuis V et al., 2013). These findings emphasize the durability and low complication rates of original prosthetic components, highlighting their importance in achieving long-term success in dental implants.
In conclusion, advancements in dental implant prosthetic designs and materials have significantly enhanced the predictability, functionality, and esthetics of implant-supported restorations. Screw-retained prostheses offer distinct benefits, particularly regarding retrievability, maintenance, and the reduction of cement-related complications, which makes them a preferred choice for both anterior and posterior applications. The introduction of angulated screw channels further broadens the clinical application of the screw-retained treatment concept. It provides improved esthetics and functional stability, especially in challenging cases.
Conclusions
Advancements in dental implant prosthetic designs and materials have significantly enhanced the predictability, functionality, and esthetics of implant-supported restorations.
Screw-retained prostheses offer distinct benefits, particularly regarding retrievability, maintenance, and the reduction of cement-related complications, which makes them a preferred choice for both anterior and posterior applications.
The introduction of angulated screw channels further broadens the clinical application of the screw-retained treatment concept. It provides improved esthetics and functional stability, especially in challenging cases.
References:
Adell R, Lekholm U, Rockler B, Brånemark P-I. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg. 1981;10(6):387–416.
Alonso R, Muñoz M, Cifuentes J-C. Original vs. non-original abutments for screw-retained single implant crowns: An in vitro evaluation of internal fit, mechanical behaviour and screw loosening. Clin Oral Implants Res. 2018;29(12):1330–8.
Chappuis V, Buser R, Brägger U, Bornstein M-M, Salvi G-E, Buser D. Long-term outcomes of dental implants with a titanium plasma-sprayed surface: A 20-year prospective case series study in partially edentulous patients. Clin Implant Dent Relat Res. 2013;15(6):780–90.
Fischer K, Stenberg T. Prospective 10-year cohort study based on a randomized, controlled trial (RCT) on implant-supported full-arch maxillary prostheses. Part II: Prosthetic outcomes and maintenance. Clin Implant Dent Relat Res. 2013;15(4):498–508.
Mattheos N, Janda M-S. Exotic encounters with dental implants: Managing complications with unidentified systems. Aust Dent J. 2012;57(2):236–42.
Mattheos N, Li X, Zampelis A, Ma L, Janda M. Investigating the micromorphological differences of the implant-abutment junction and their clinical implications: A pilot study. Clin Oral Implants Res. 2015;26(8):915–21.
Jørgensen K D. The relationship between retention and convergence angle in cemented veneer crowns. Acta Odontol Scand. 1955;13(1):35–40.
Rella E, De Angelis P, Damis G, D'Addona A, Manicone P F. The application of angulated screw-channels in metal-free, implant-supported restorations: A retrospective survival analysis. Materials (Basel). 2021;14(22):7006.
Reis I N R D, Fukuoka G L, Nagay B E, Pannuti C M, Spin-Neto R, da Silva E V F. Incidence of peri-implant disease associated with cement- and screw-retained implant-supported prostheses: A systematic review and meta-analysis. J Prosthet Dent. 2023;130(1):35–47.
Sarafidou K, Zoidis A P, Polyzois S E. Screwmentable implant-supported prostheses: A systematic review. J Prosthet Dent. 2023;130(1):35–47.
Strong S M. What's your choice: cement- or screw-retained implant restorations? Gen Dent. 2008;56(1):15–8.
Wismeijer D, et al. Consensus statements and recommended clinical procedures regarding restorative materials and techniques for implant dentistry. Int J Oral Maxillofac Implants. 2014;29(suppl):137–40.
Wittneben J G, Buser D, Salvi G E, Bürgin W. Complication and failure rates with implant-supported fixed dental prostheses and single crowns: A 10-year retrospective study. Clin Implant Dent Relat Res. 2014;16(3):356–64.
Wittneben J G, Millen C, Brägger U. Clinical performance of screw- versus cement-retained fixed implant-supported reconstructions: A systematic review. Int J Oral Maxillofac Implants. 2014;29(suppl):84–98.

