Introduction
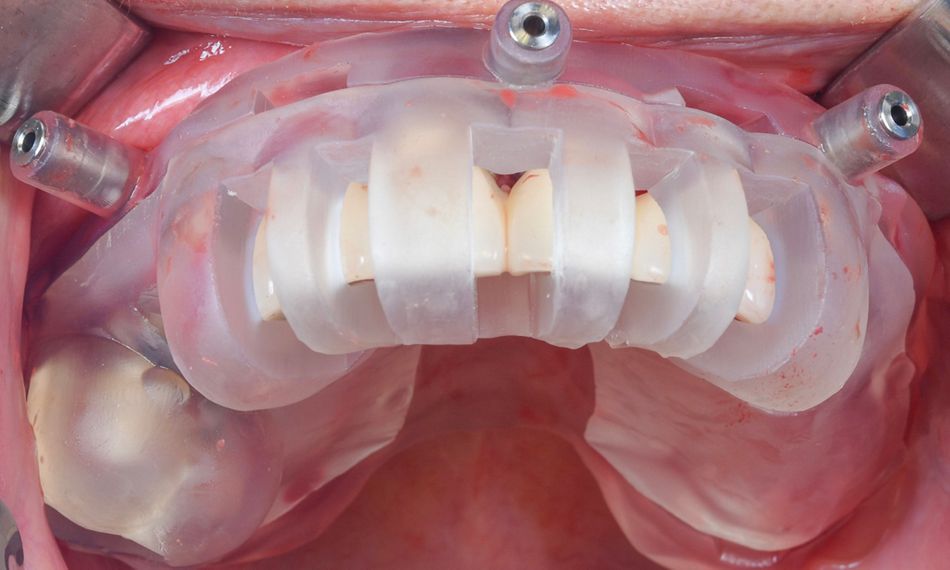
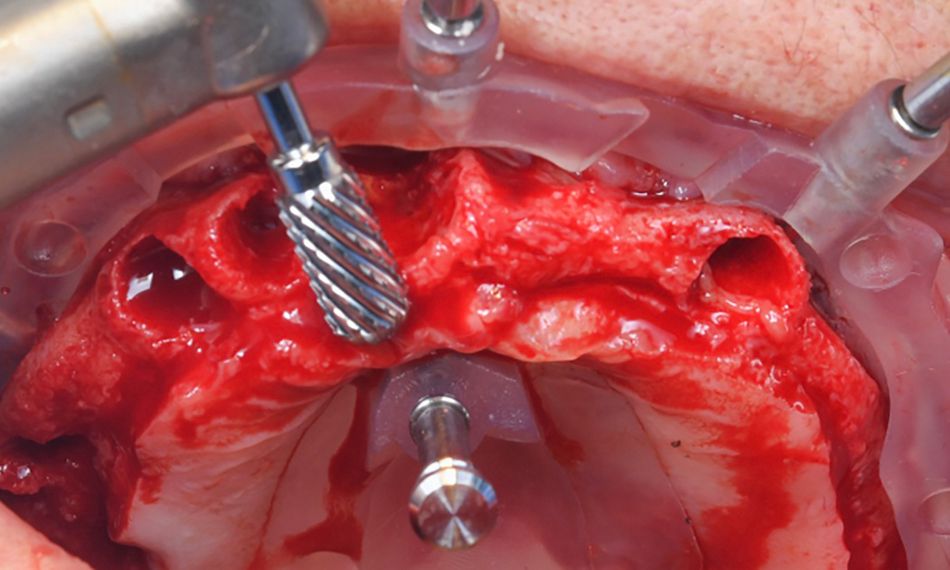
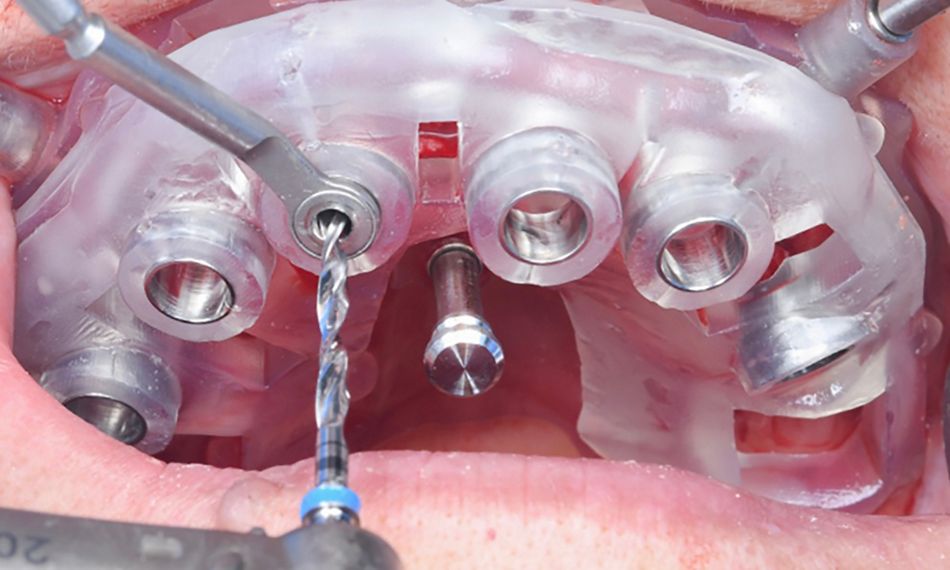
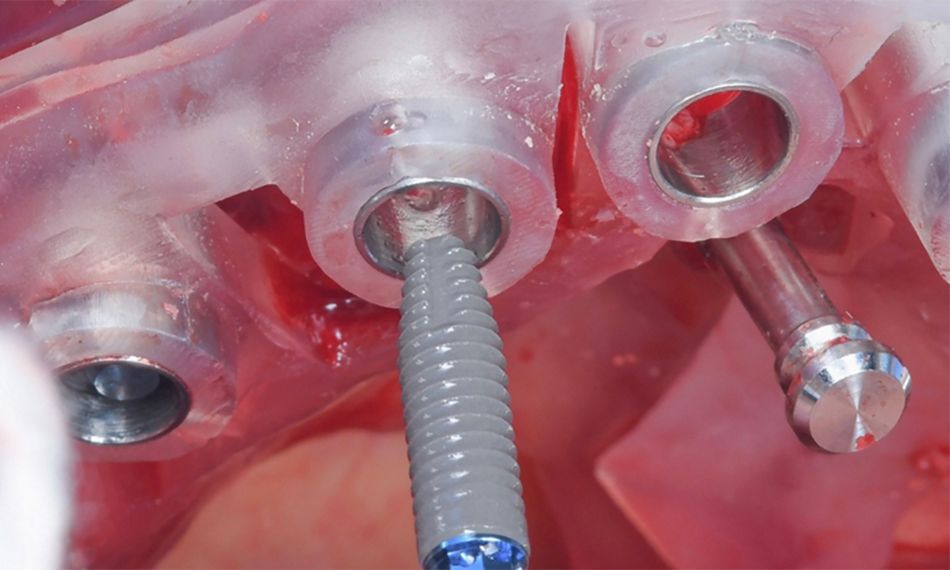
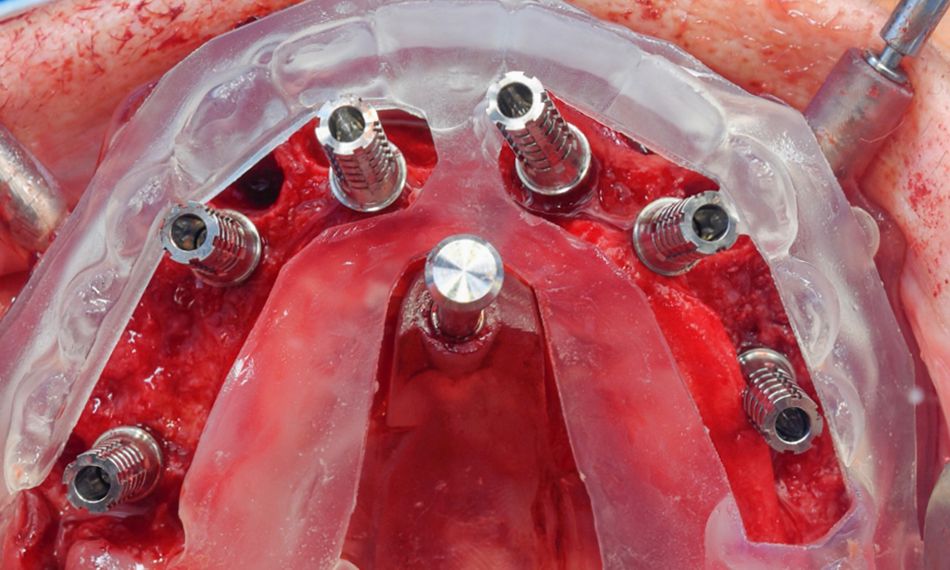
New developments, such as virtual-guided technologies, offer an optimal approach for implant placement, aligning with the accurate prosthetic position and minimizing both intraoperative trauma and procedure duration. 4
The following case report demonstrates the successful management of a 70-year-old patient experiencing chewing difficulties. Through a maxillary full-arch, implant-supported rehabilitation with six Straumann® BLT implants facilitated with a digital workflow, we improved her quality of life and fulfilled her expectations.
Initial situation
A 70-year-old healthy female with no medication, allergies, or smoking habits came to our clinic seeking a resolution for her difficulties with chewing. Additionally, she reported a history of persistent dental and oral malodor issues. The patient expressed a desire to “go back in time” and be able to eat like before and recover her quality of life and confidence.
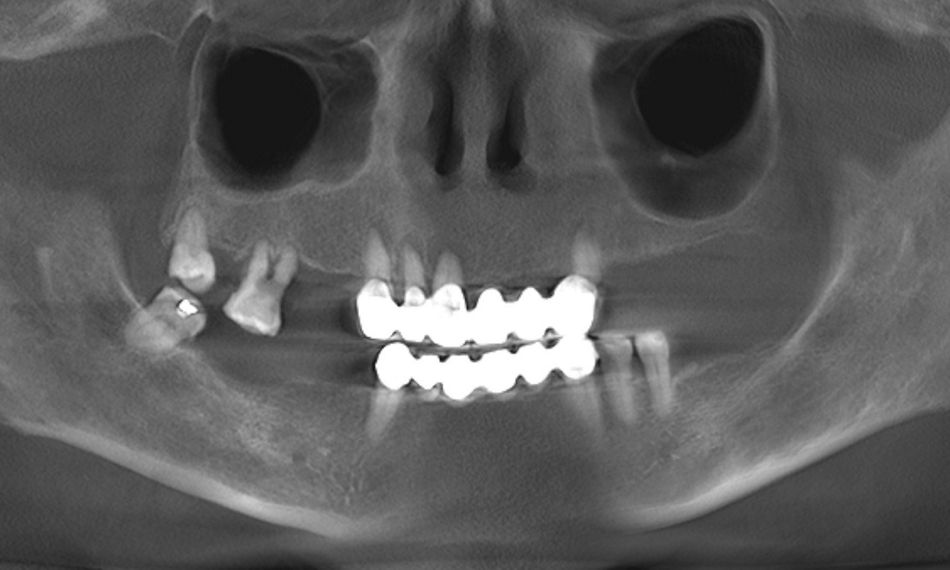
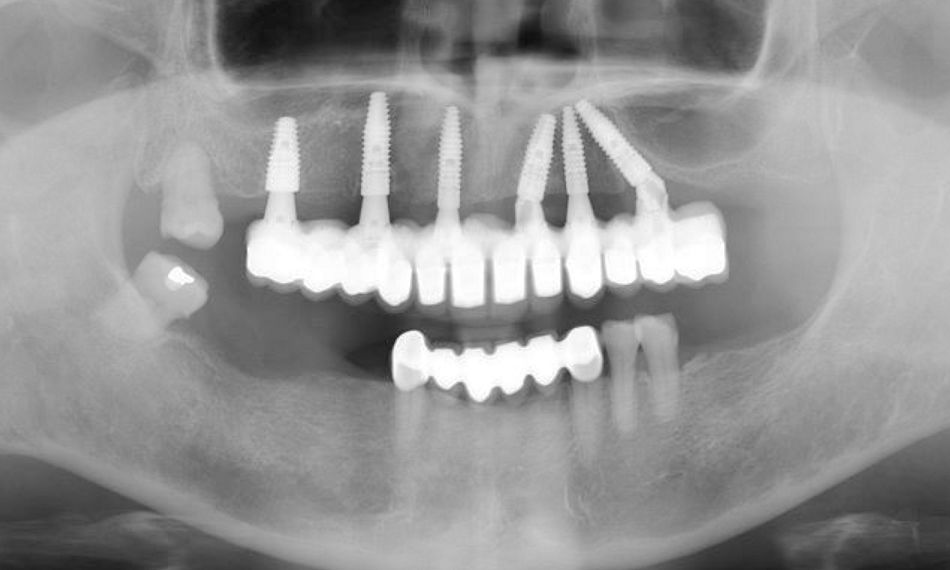
The extraoral examination showed a low smile line. On the other hand, the intraoral examination depicted a bridge from #13-#23 in hopeless conditions. The teeth of the upper jaw, with the exception of #18, were mobile. Generalized gingival inflammation, bleeding on probing and dental caries were also present (Fig. 1). In addition, the patient exhibited a removable prosthesis in the upper jaw that was poorly adapted and showed signs of deterioration. The radiographic examination exposed severe bone loss on the posterior side of the 2nd quadrant. Furthermore, images were also compatible with caries and apical lesions on maxillary teeth (Fig. 2).
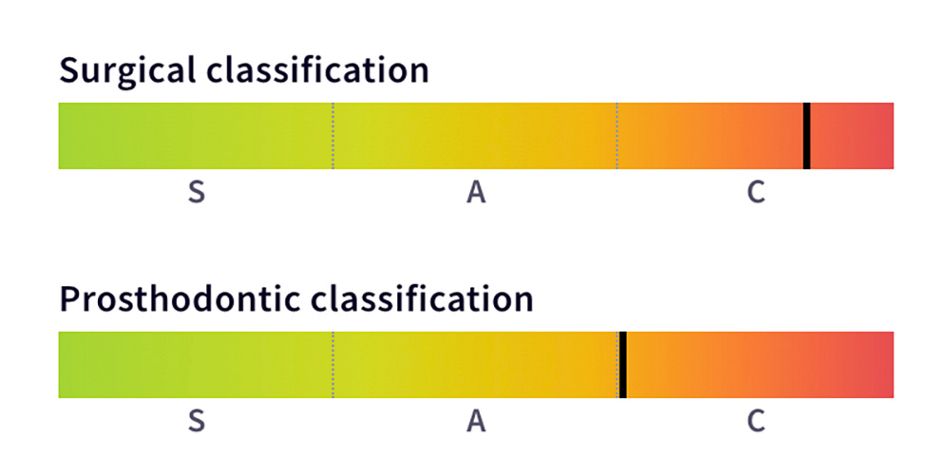
After conducting both radiographic and clinical assessments, the patient was categorized as having a complex condition according to both the surgical and prosthodontic SAC classifications. This classification system assists in evaluating the level of challenge and potential complications linked to implant-related restoration (Fig. 3).