Introduction
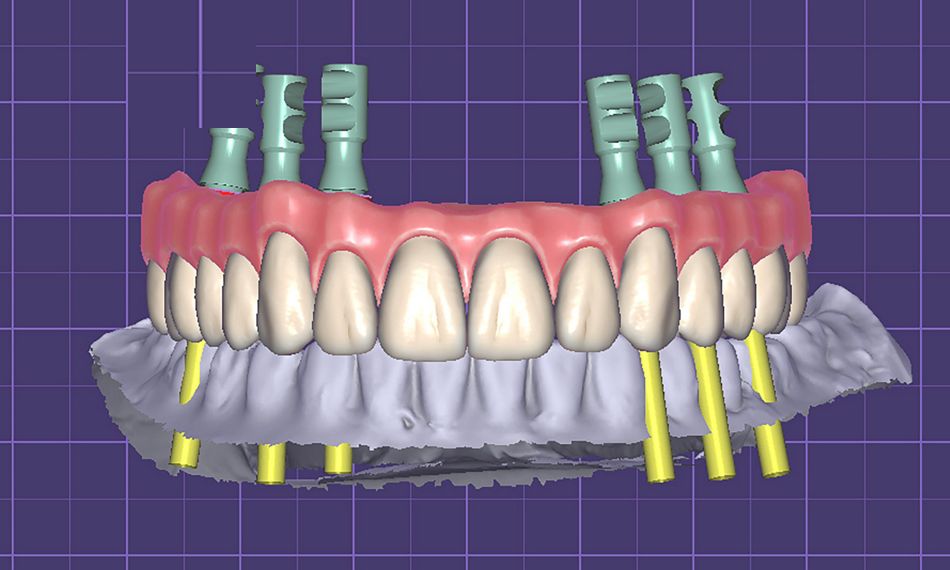
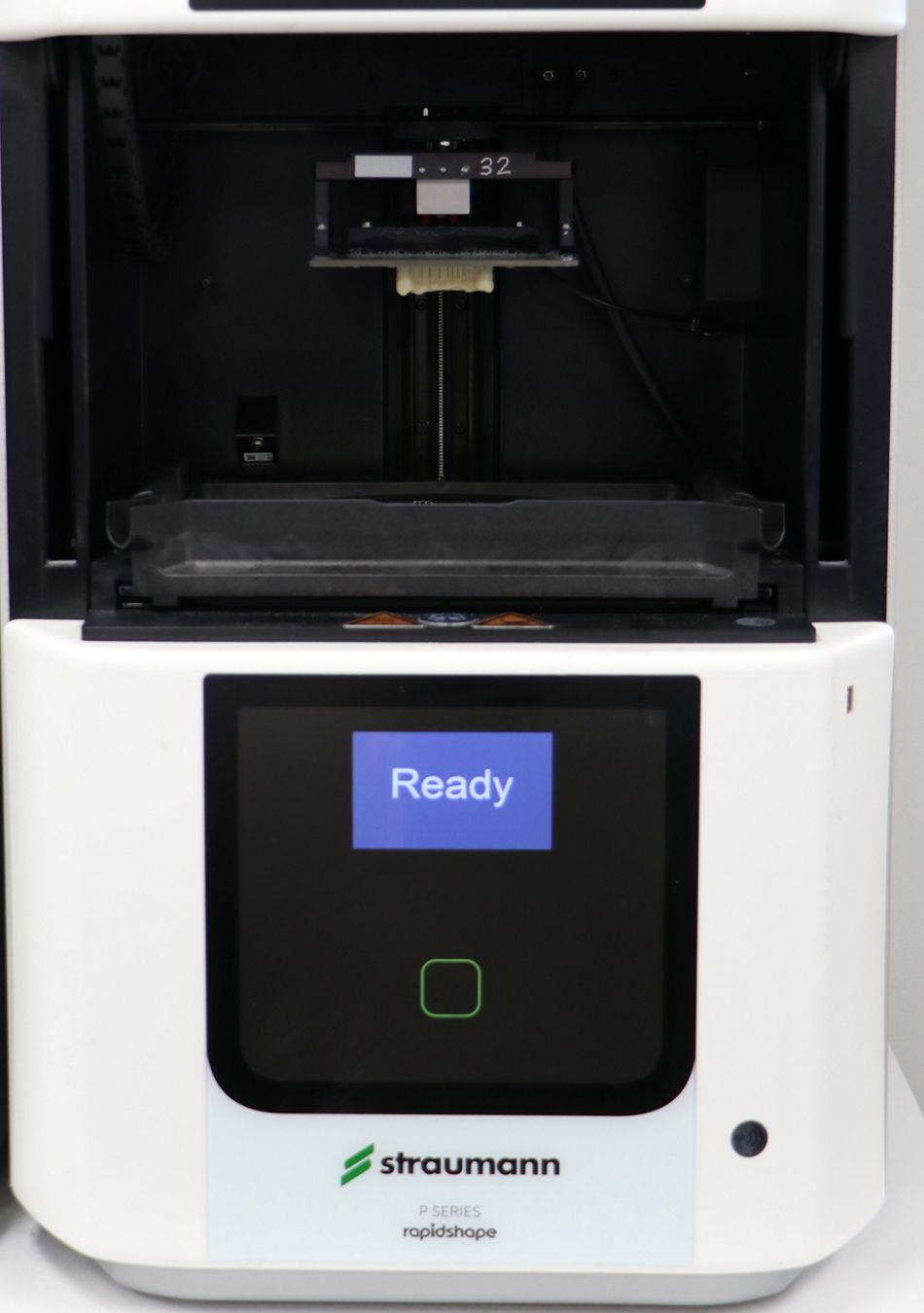
The rise and spread of digital dentistry have significantly influenced clinicians who specialize in implant dentistry and full-arch restorations.3 The continued development of CAD/CAM technology and 3D printing has revolutionized the manufacture of tooth-borne and implant-supported fixed dental prostheses.4
Digital technologies for fabricating fixed full dental prostheses with implants can result in less expensive laboratory and clinical chairside time and lower overall cost.5
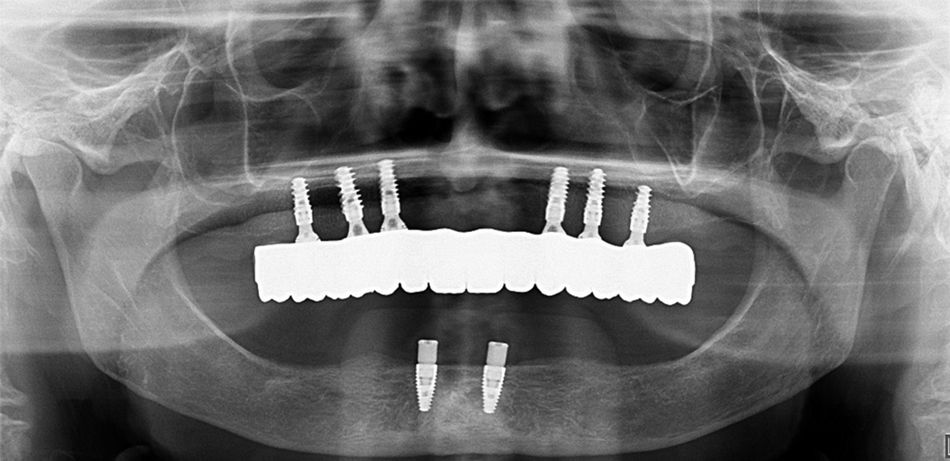
Furthermore, due to its excellent survival rate, immediately loaded implants with a fixed prosthesis have become a feasible choice in the rehabilitation of edentulous patients.6
The following case report aims to show a successful treatment with immediate loading of a final fixed restoration in the edentulous maxilla with Straumann® BLX implants.
Initial situation
A systemically healthy, non-smoking 59-year-old female with no medication or allergies attended our clinic with the following chief complaint: “I have been wearing full dentures for many years, but now I find that they come loose easily, which prevents me from eating and speaking normally. Would it be possible to improve my situation without going through complex surgeries or waiting a long time?“
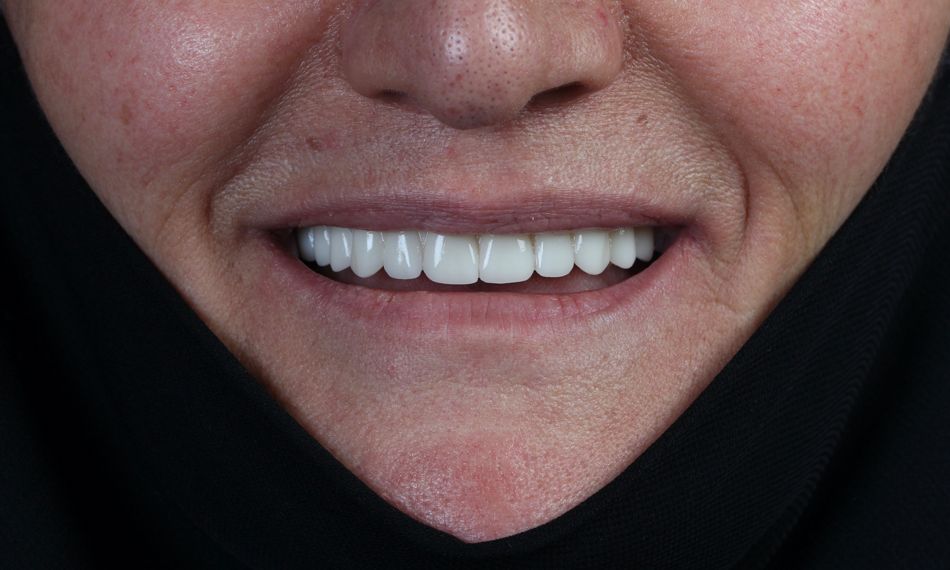
The extraoral examination with the denture depicted a medium smile line and loss of the occluding vertical dimension due to the wear of the denture. Without the denture, inadequate soft tissue support, which affected the facial esthetics, was apparent (Fig. 1).
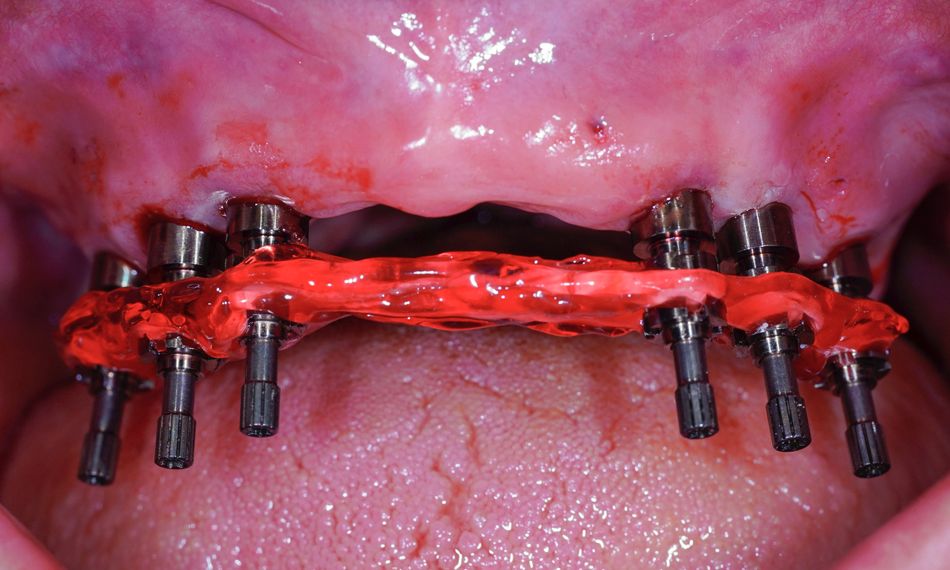
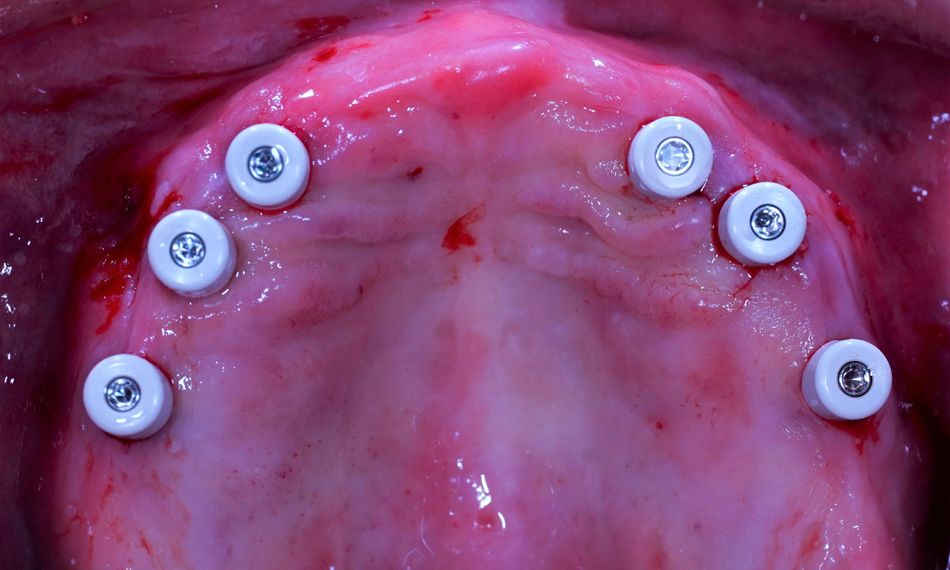
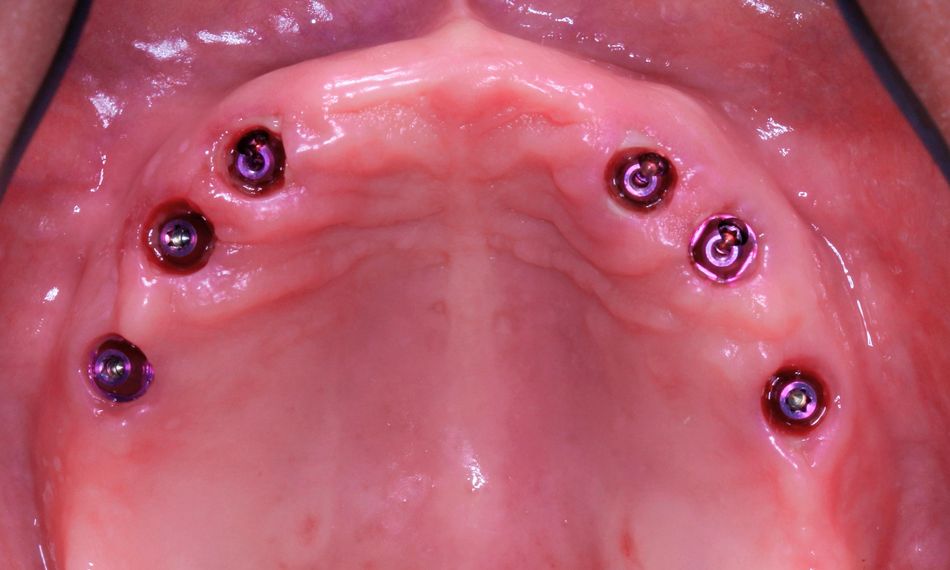
The intraoral examination showed that the supporting soft tissues were slightly inflamed. The alveolar ridge of the maxilla and mandible showed a loss in width and height, although it was still sufficiently wide and covered with relatively healthy keratinized mucosa (Fig. 2).