Introduction
Technological progress, including the proliferation of internet access worldwide, has given patients access to a wealth of information about their oral health and has raised awareness of the range of available treatments, materials and techniques. As a result, patients’ expectations and behaviors have changed and an ever-increasing number are requesting less invasive, affordable, efficient, and immediate solutions.
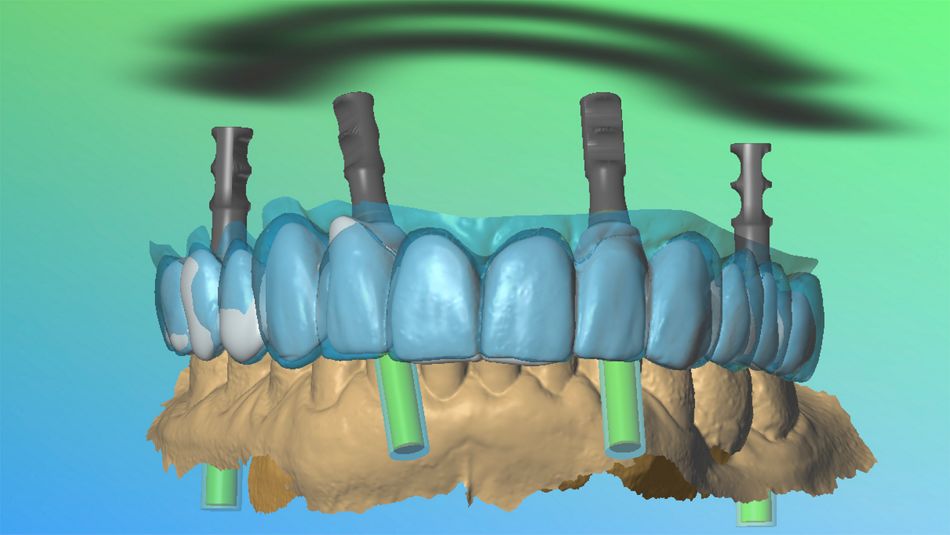
The Straumann® Pro Arch Concept enables personalized treatment protocols with various treatment options to address specific indications and clinical scenarios. This concept covers all stages of an immediate full arch treatment and includes the use of implants specifically designed for immediate procedures, with a flexible prosthetic portfolio that considers patients’ esthetic expectations and financial resources.
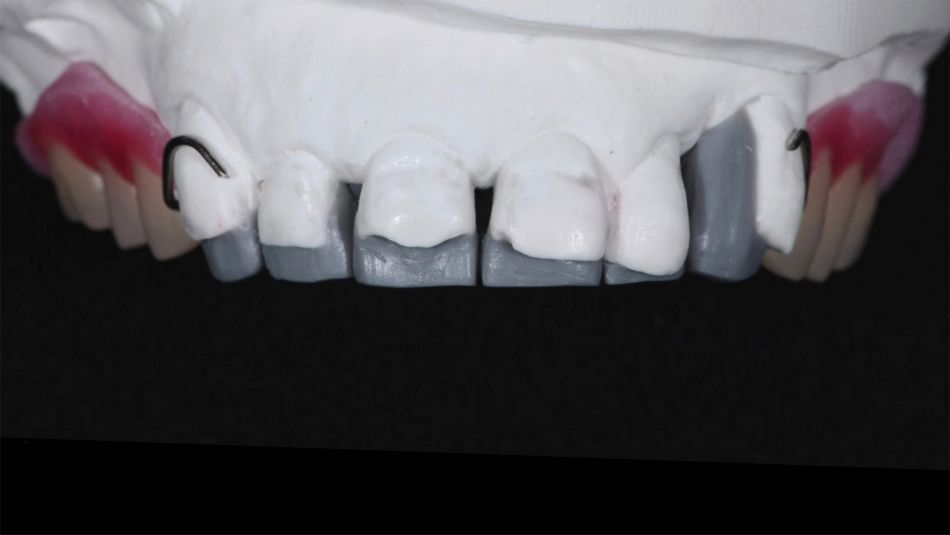
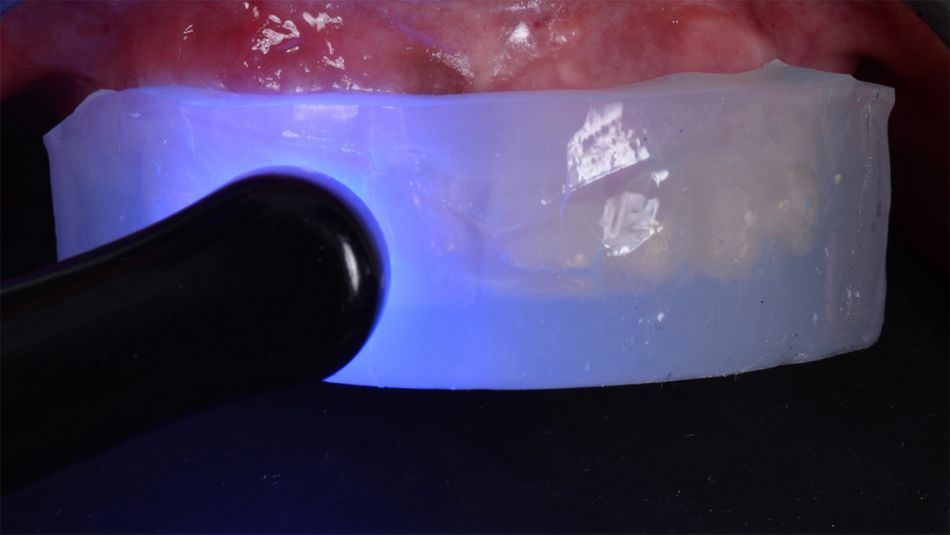
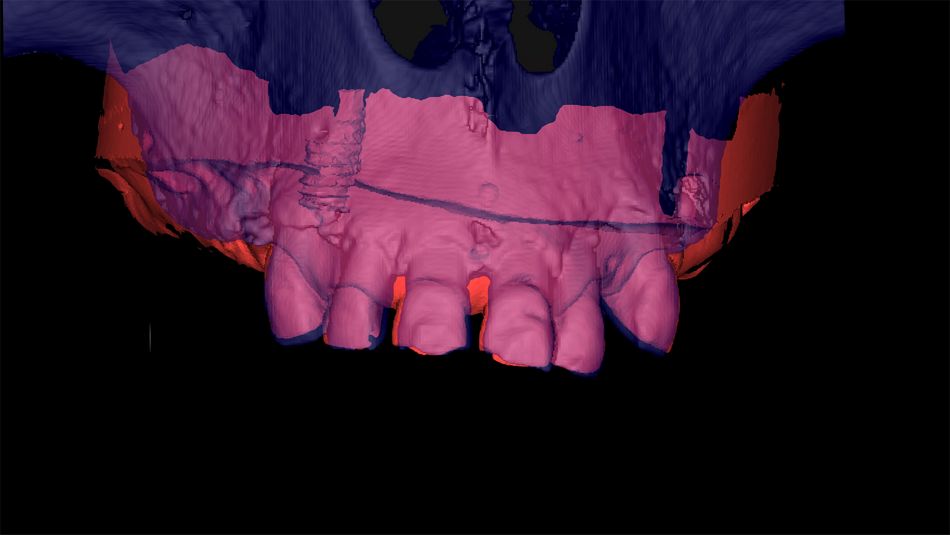
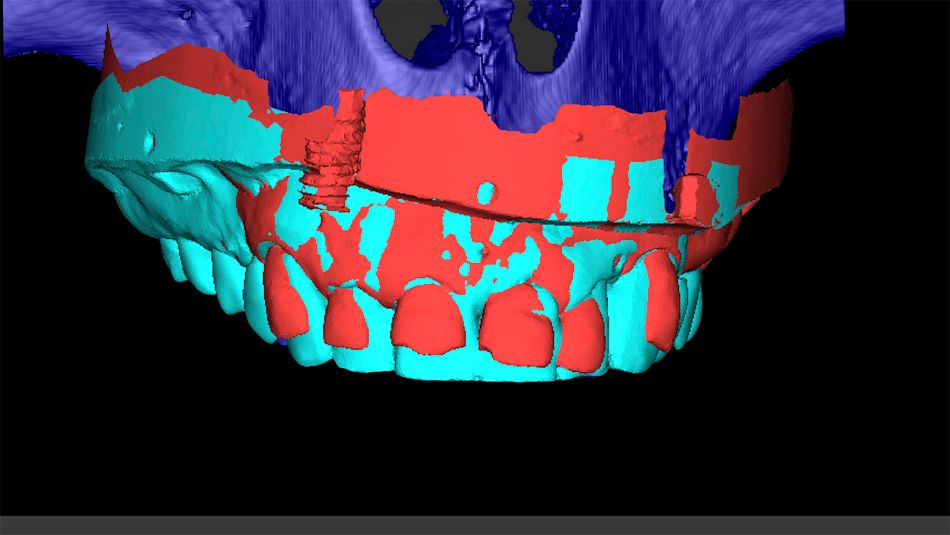
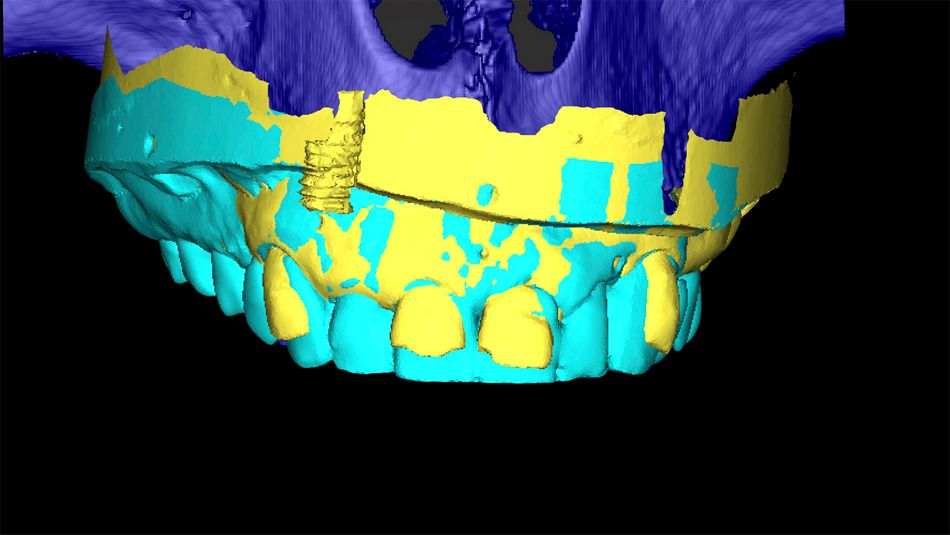
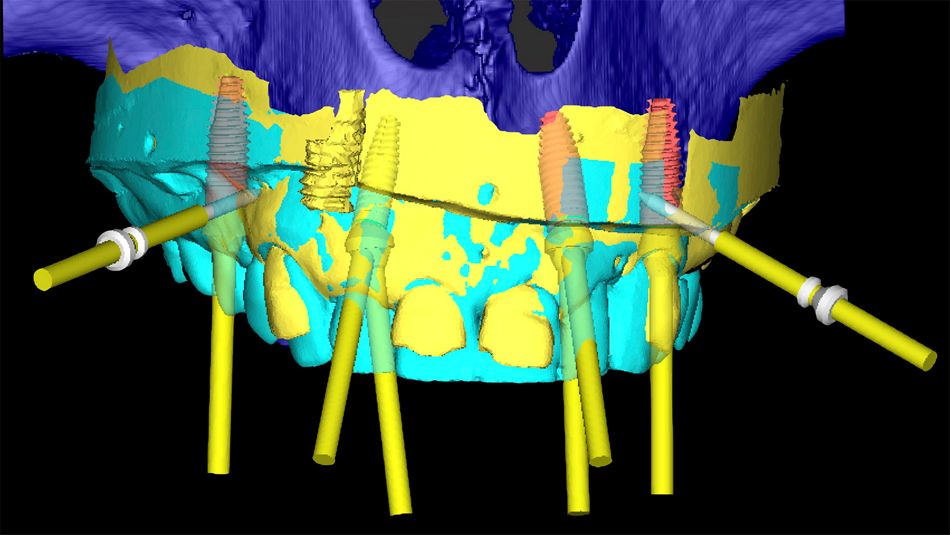
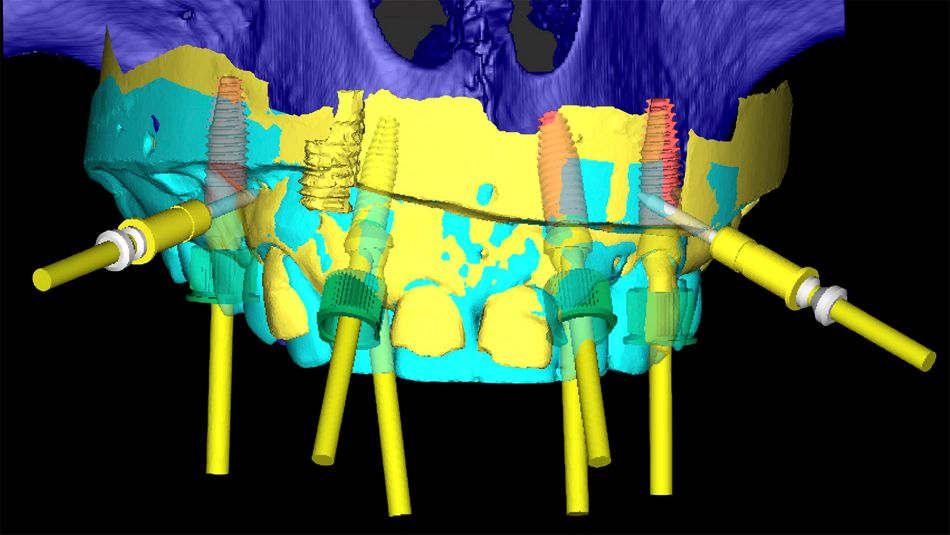
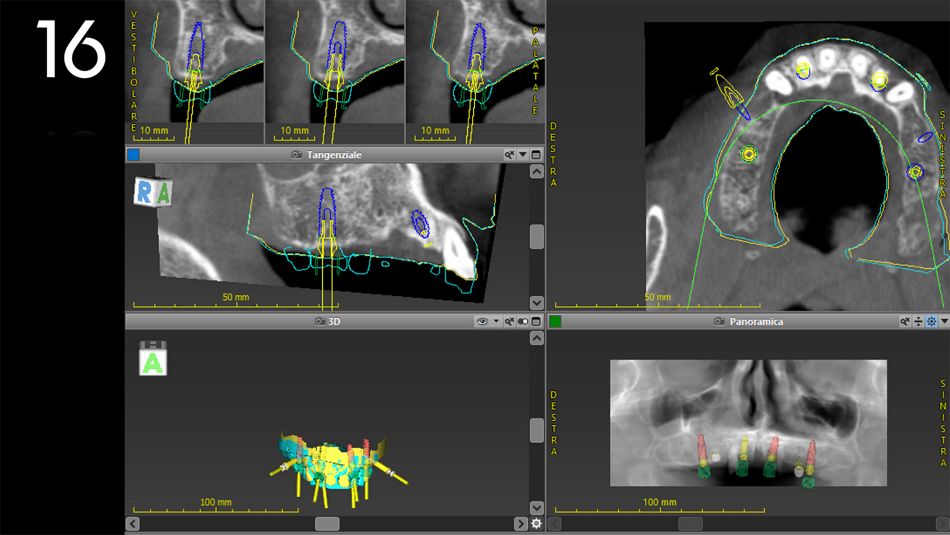
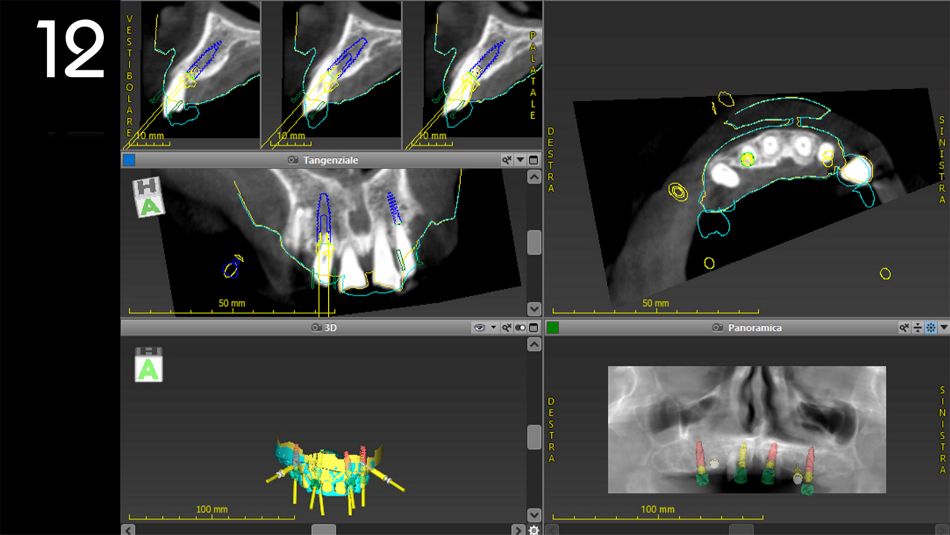
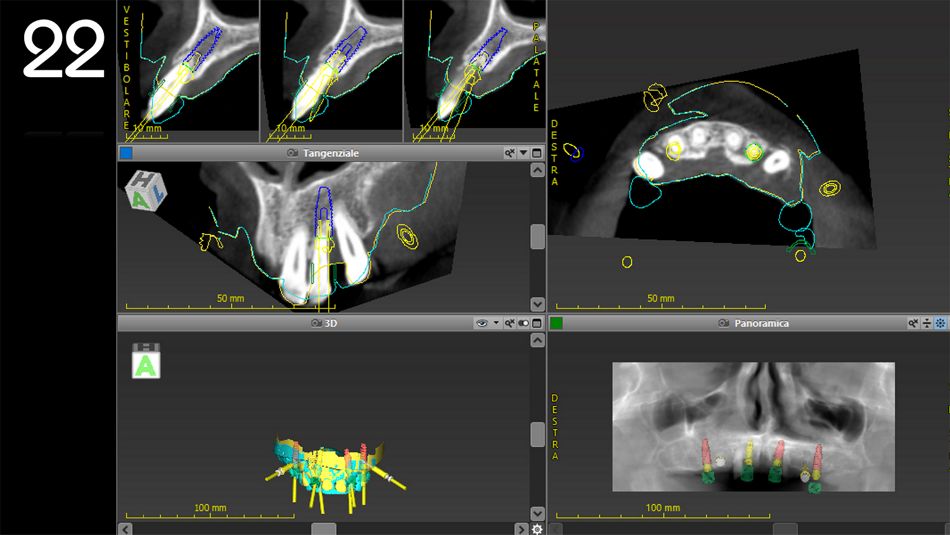
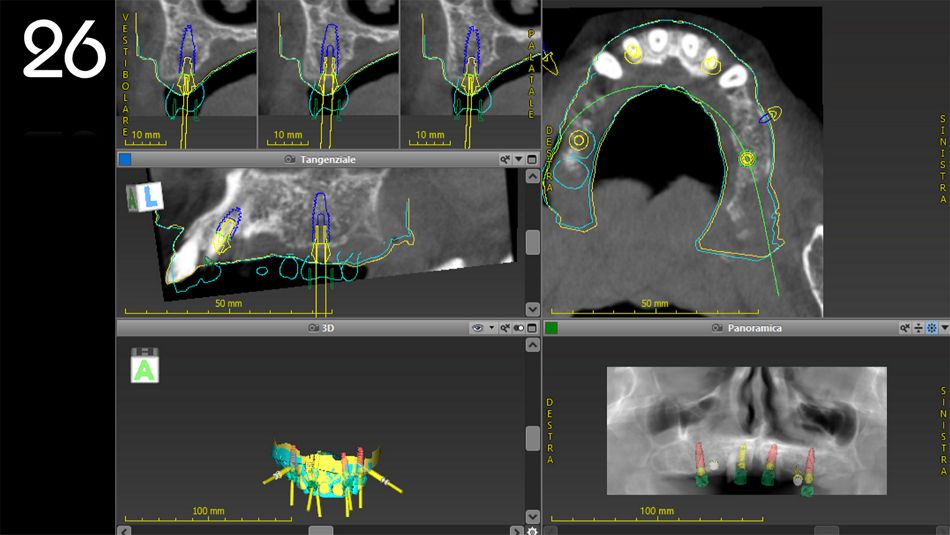
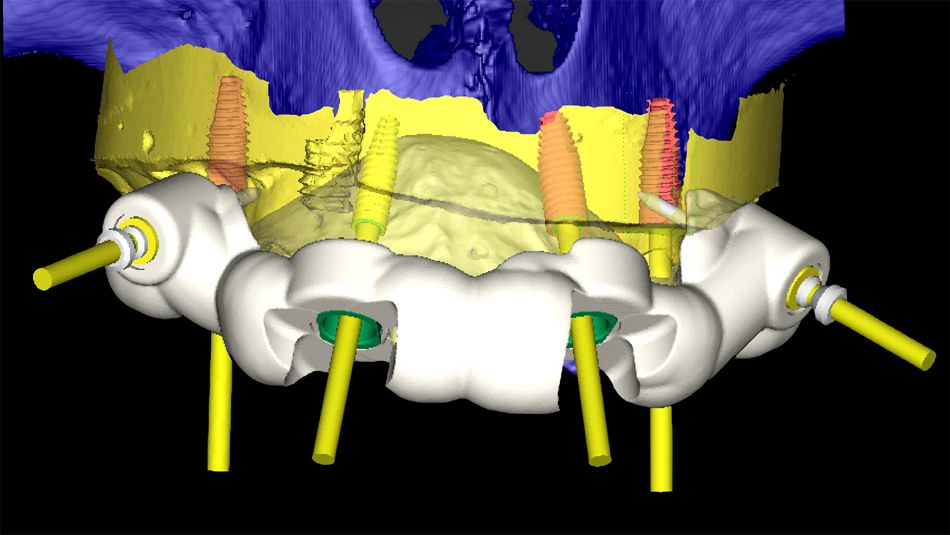
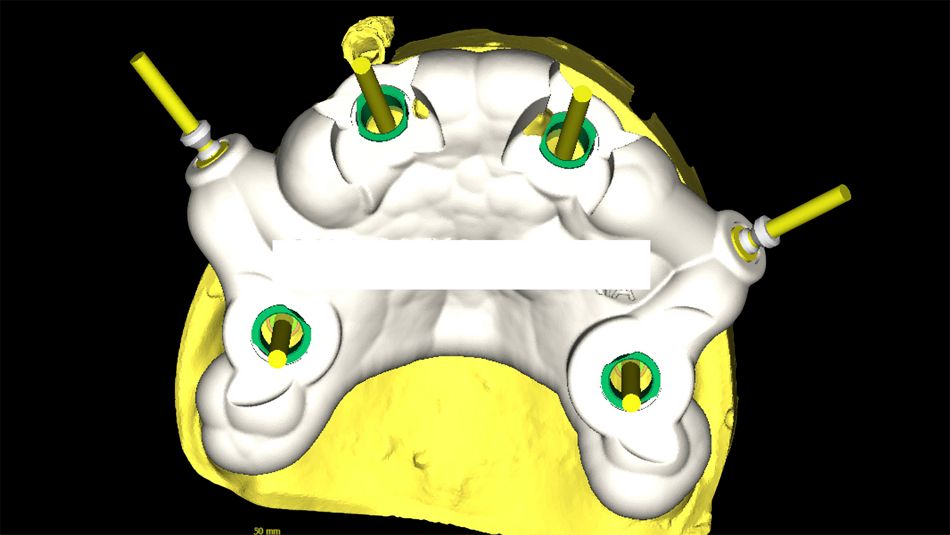
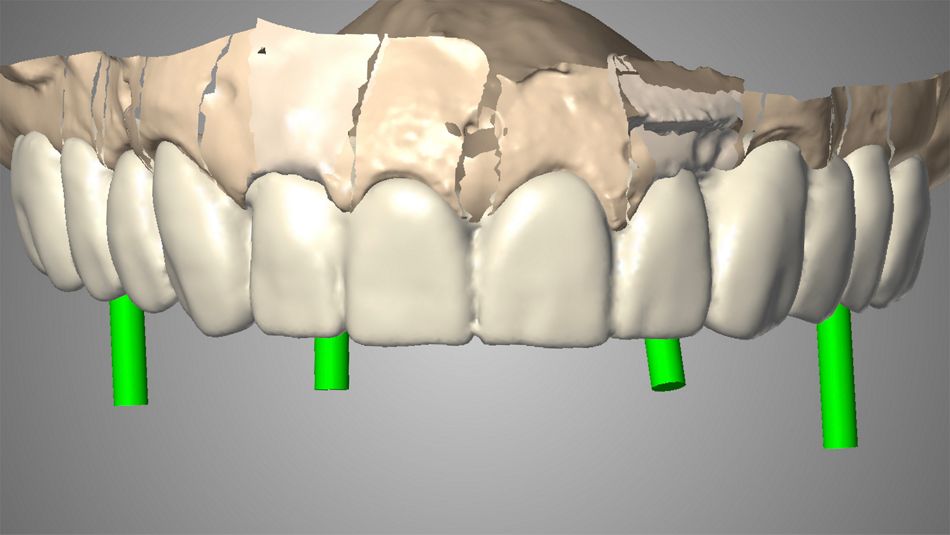
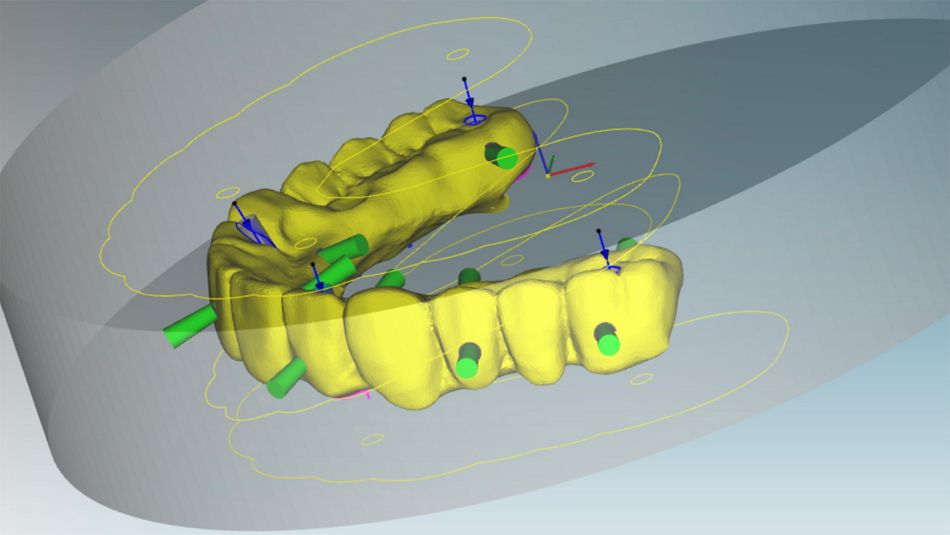
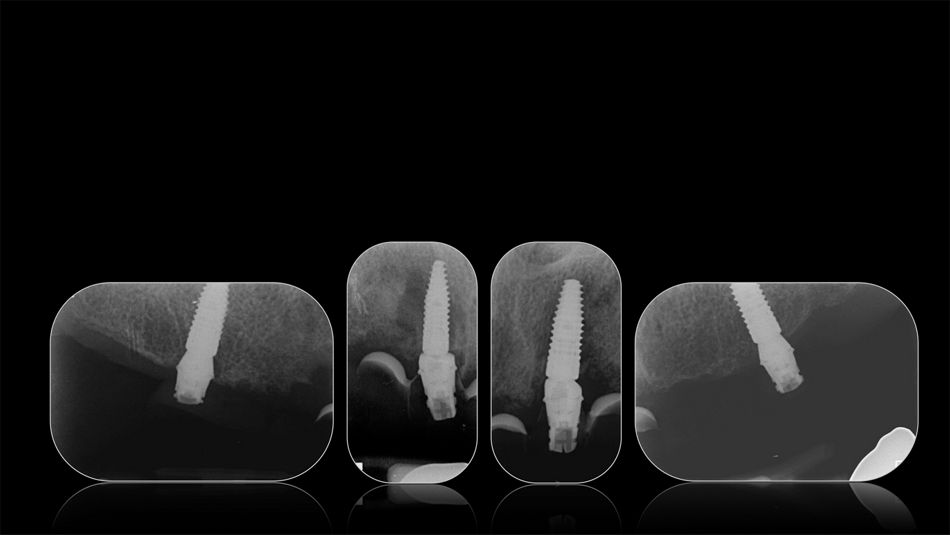
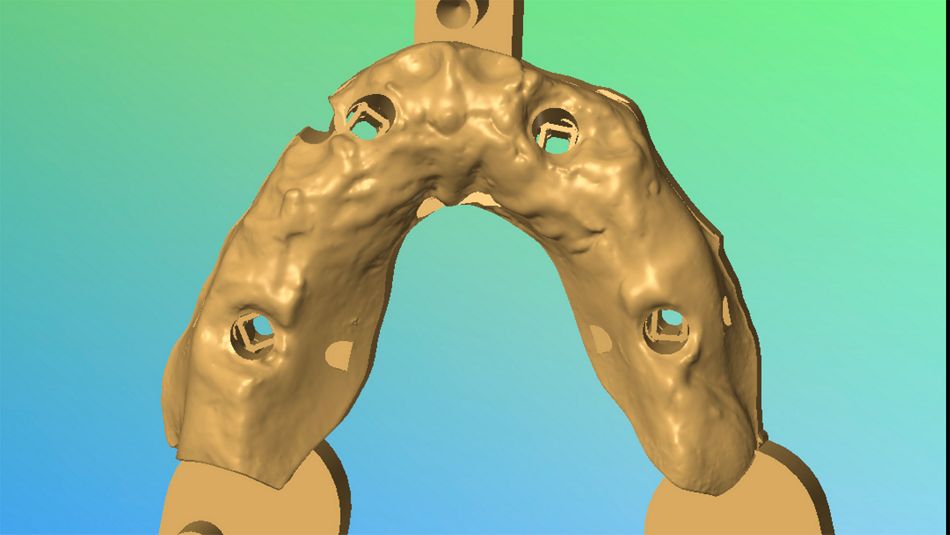
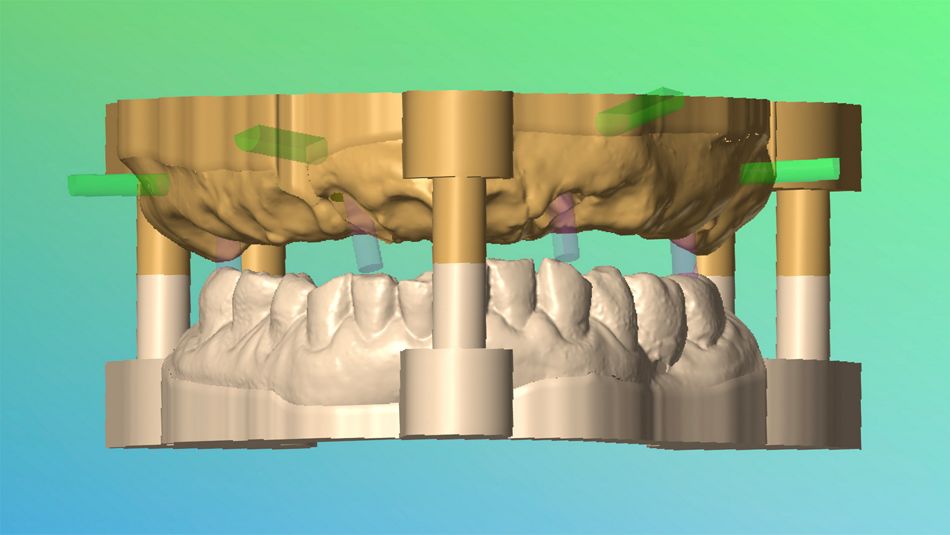
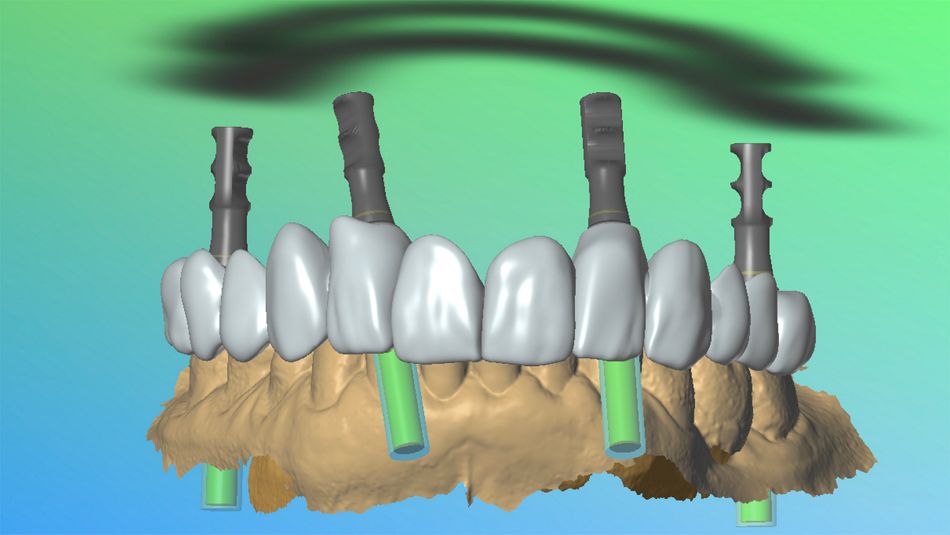
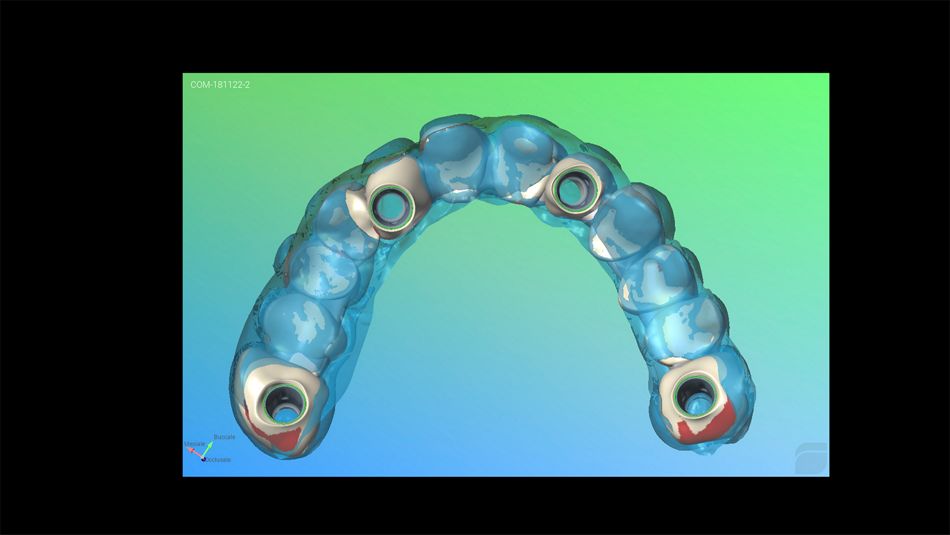
The following case report describes a successful functional and esthetic prosthetic full-arch implant rehabilitation of a patient with a hopeless maxillary dentition and decreased quality of life due to impaired masticatory function and poor esthetics. The Straumann® Pro Arch Concept with Straumann® Bone Level Tapered (BLT) implants and Straumann® Screw Retained abutments (SRA) allowed us to address our patient’s chief complaints by providing an efficient and predictable solution. The immediate treatment workflow involved 4 steps; 1) accurately creating a pre- operative dental model; 2) surgical and prosthetic planning with coDiagnostiX® software; 3) placing the dental implants with computer-guided and flapless technique; and 4) finally performing an immediate loading procedure.
This clinical outcome was achieved in a single day and with no complications. The patient was highly satisfied with the positive impact the treatment had on her quality of life due to significantly improved esthetics and recovery of masticatory function.
Initial situation
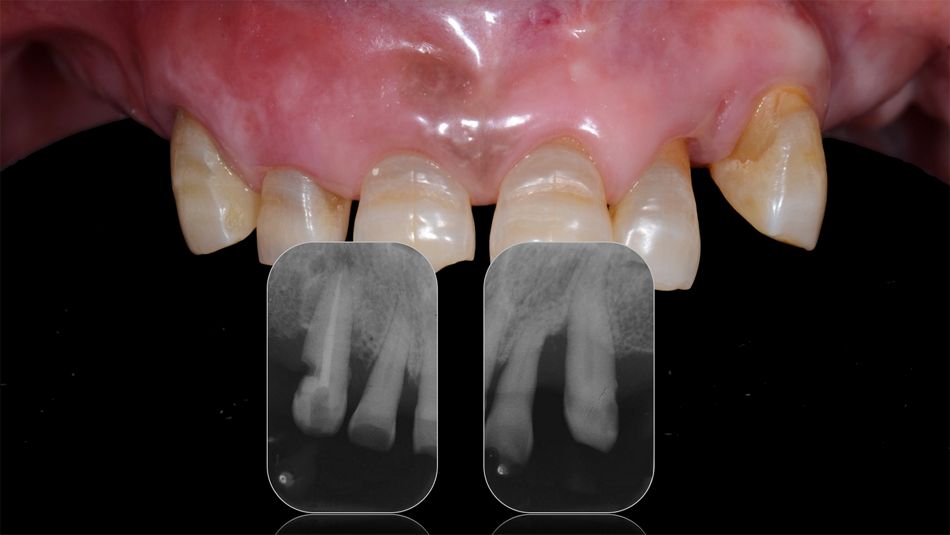
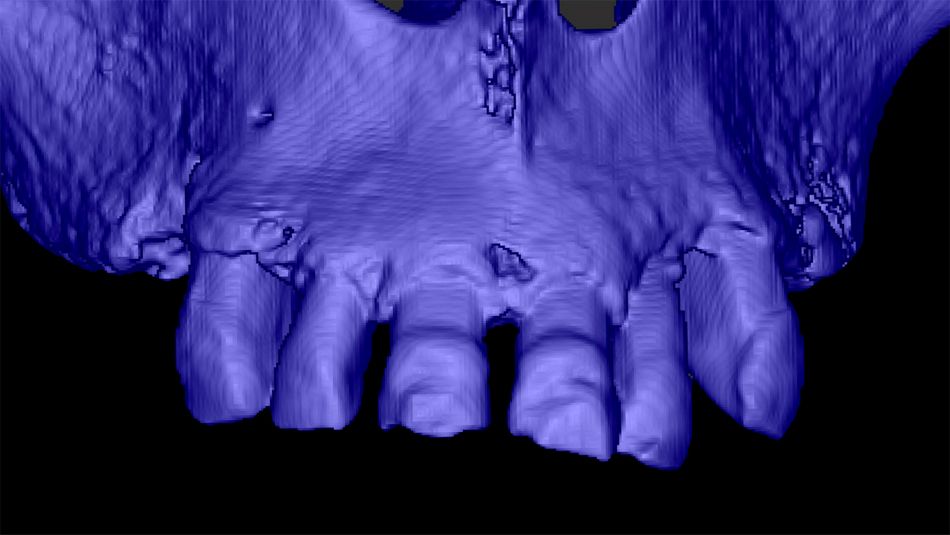
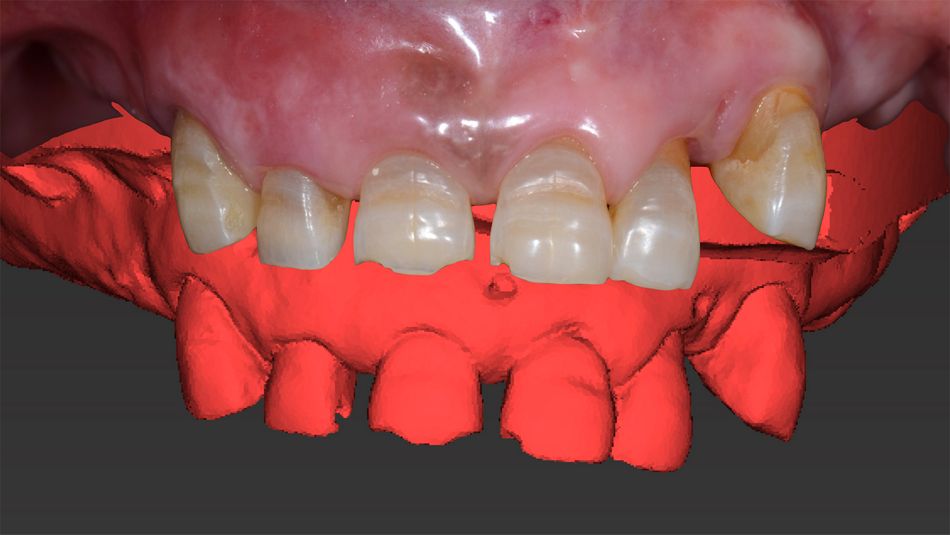
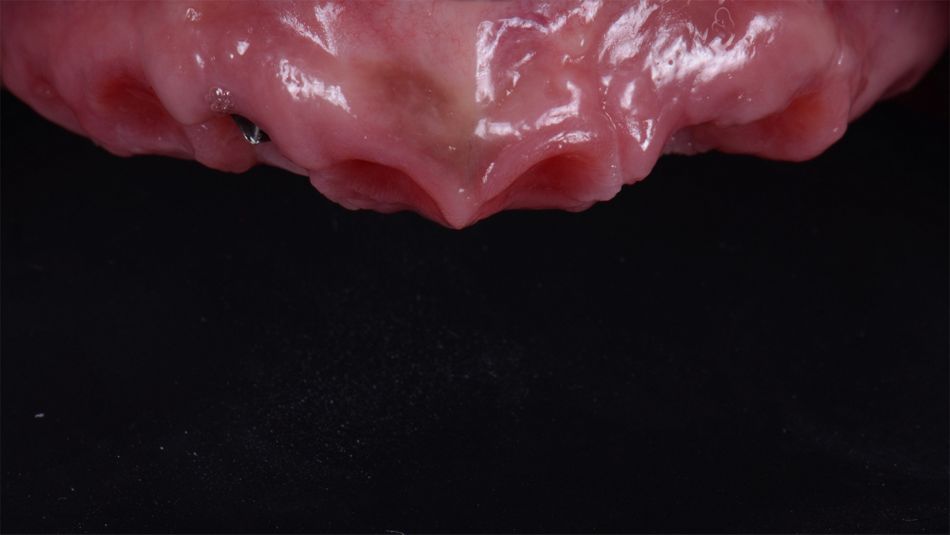
A systematically healthy 58-year-old female patient presented to our office with the chief complaint of esthetic dissatisfaction and impaired masticatory function due to an unstable removable partial denture (Fig. 1).
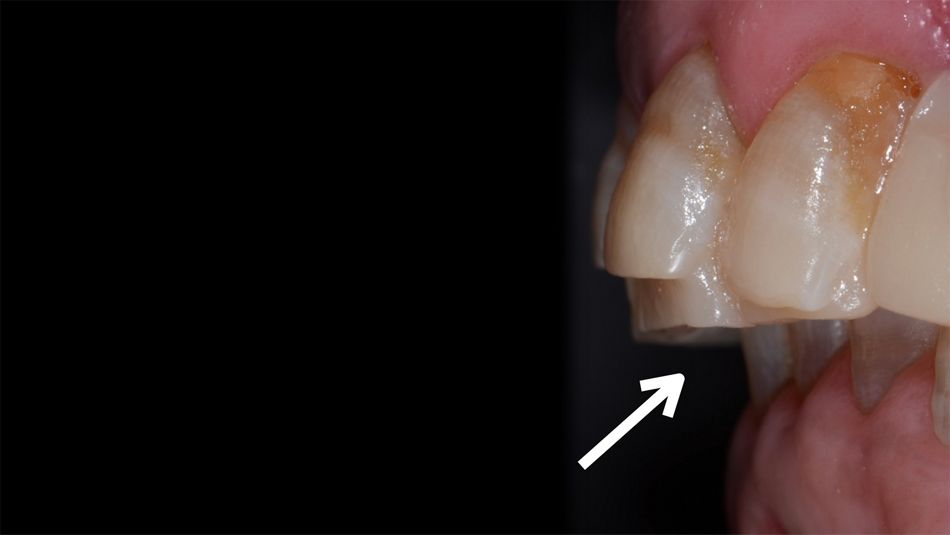
The initial comprehensive clinical evaluations revealed partial edentulism, a deep overbite with the lower incisors impinging upon the palatal gingiva and increased overjet. The upper incisors were buccally tilted and presented tooth wear and mobility. Moreover, there was interference between the lower lip and the anterior teeth in the smile position (Figs. 2-5).