Introduction
Driven by patient demands and increased clinical evidence, recent developments in implant dentistry have seen a pronounced trend towards early and immediate procedures7. This trend has been especially pronounced for full-arch rehabilitations that prevent patients from being exposed to a long period of edentulism8–10.
One of the clinically most relevant factors for the prognosis of implant success of immediate procedures is primary implant stability11,12. This factor becomes even more important in patients with compromised bone quality or quantity13. The novel BLX implant with its self-tapping tapered implant body and its protruding thread geometry represents one of the most promising tools to help clinicians achieve a high level of bone engagement and immediate primary stability14.
Although recent research suggests good clinical success rates for full-arch restorations even in periodontally compromised patients, a combination of optimized primary stability, surgical flexibility and long-term tissue level stability could be highly desirable15,16.
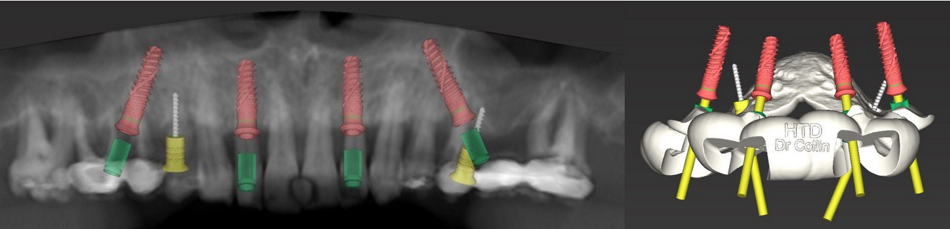
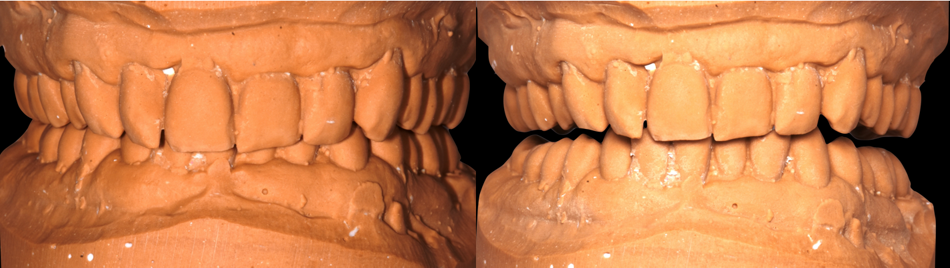
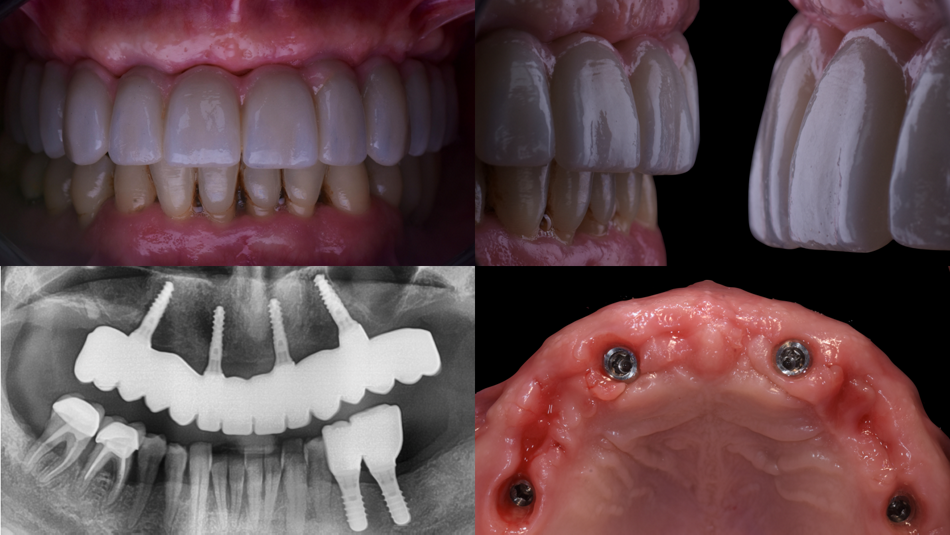
The following case report describes the procedure and 1 year follow-up of a full-arch restoration with the novel Straumann® TLX Implant System, using a straightforward direct-to-implant restorative concept. The novel implant system combines the endosteal design of the BLX implant system for optimal primary stability, with an emergence profile that has proven to deliver successful long-term soft tissue stability. This qualifies the system for immediate procedures in situations with an enhanced hygiene requirement, for example in the illustrated treatment of a periodontally compromised patient.
Initial situation
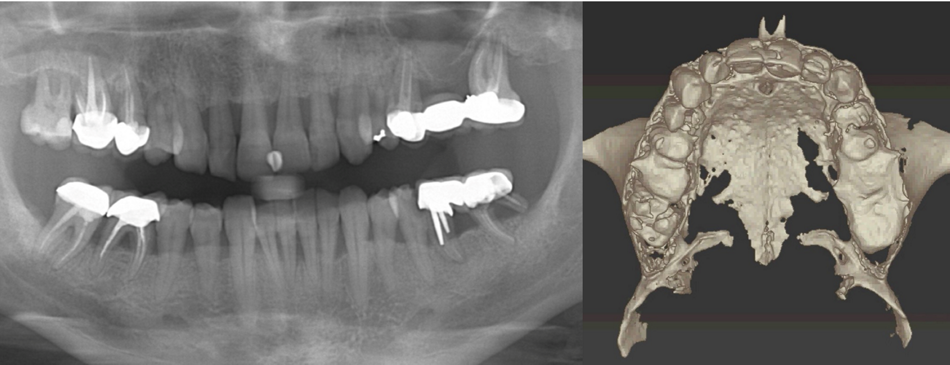
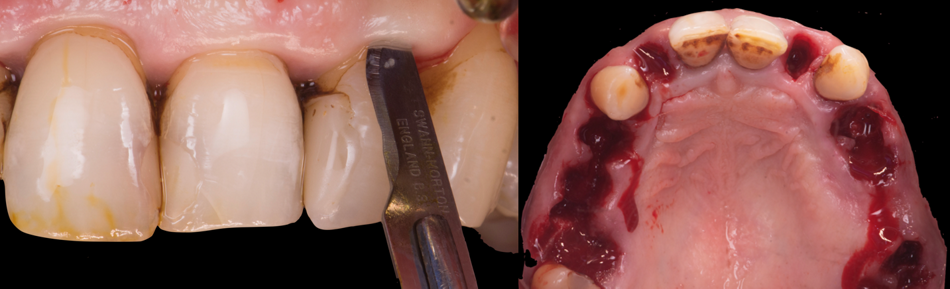
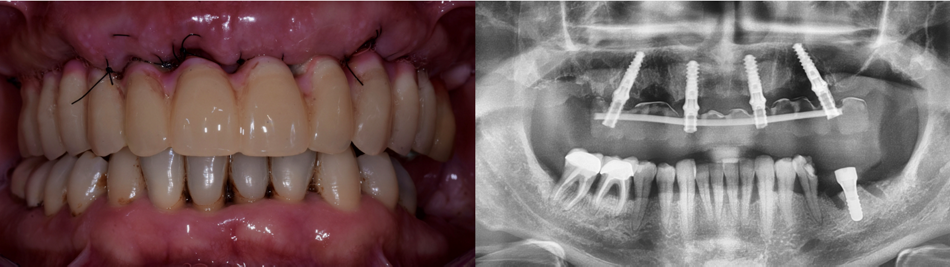
A 49-year-old patient presented in our clinic after a prolonged period without dental check-ups and with a complaint of unsatisfactory esthetics and discomfort while eating due to teeth mobility (Fig. 1). The patient reported that he was a smoker and had limited time available because of his professional activity. Oral examination revealed severe generalized periodontitis (stage III to IV) associated with poor oral hygiene, as evidenced by the presence of advanced gingival recessions, exposed root surfaces, abnormally pale gingival color, loss of interdental papillae and Miller class I tooth mobility17. The patient was in good general health and had no absolute contraindications for implant treatment.