Dental implants are constantly exposed to the microbe-laden environment of the oral cavity which leads to a rapid formation and growth of biofilms on the prosthetic and connecting elements of the restoration [13]. Supported by appropriate oral hygiene measures these biofilms are held in a stable balance (homeostasis) by the patient’s immune system with the result of clinical peri-implant health.
Peri-implant mucositis and peri-implantitis represent undesired biological complications that may ultimately lead to implant loss and treatment failures14. Restorative designs, treatment regimens and maintenance protocols have to ensure that conditions can be achieved and maintained that successfully prevent such complications. Here we present 5 simple, but fundamental aspects that should be considered in your clinical practice to ensure the long-term success of full arch restorations.
1. Start at the beginning - Presurgical hygiene
Patients considered for full-arch restorations often present with a failing dentition affected by severely progressed caries and periodontitis. These clinical findings are often associated to a history of poor oral hygiene skills and habits. Implant-placement in such patients seems to be counter-intuitive as any reoccurrence of such pathogen associated conditions may represent a risk-factor to the future implant restoration. Therefore, the reestablishment of an adequate oral health status is as important as the instillation of the fundamentals and habits of good oral hygiene into patients prior to commencing any advanced implant treatment.
Along and following causative treatment of any pathogenic conditions patients may be prepared for implant therapy by thorough instructions for oral hygiene. Reevaluation visit may e.g. not only be used to assess the patient’s response to treatments but also to ensure that adequate levels of plaque control are achieved and maintained by compliance with oral hygiene routines14.
Further treatment planning should comprise a thoughtful analysis of risk factors related to e.g. the recurrence of periodontal disease or the onset of any future peri-implant disease. As a general guideline, any precondition that may interfere or alter the innate or adaptive immune responses to a bacterial challenge, like. e.g. smoking may put the oral health status and any future implant restoration at risk15, 16.
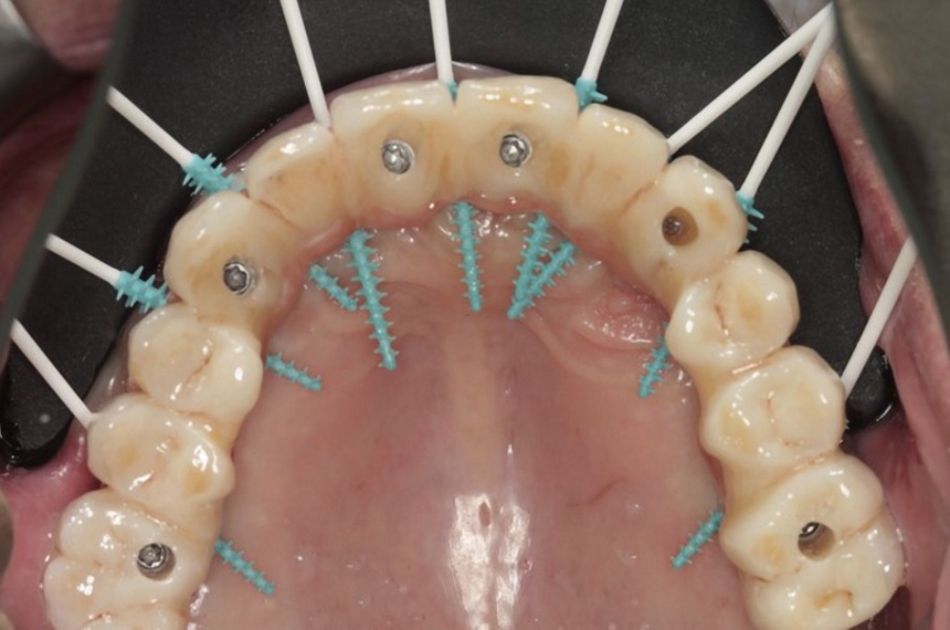
The implementation of an early preoperative hygiene therapy regimen represents an integral part to our treatment approach at Campbell clinic when providing full arch restorations. We routinely provide patient individualized oral hygiene instruction and constantly evaluate patient compliance with oral hygiene principles to improve post-operative outcomes and the results of our maintenance regimes17–19.