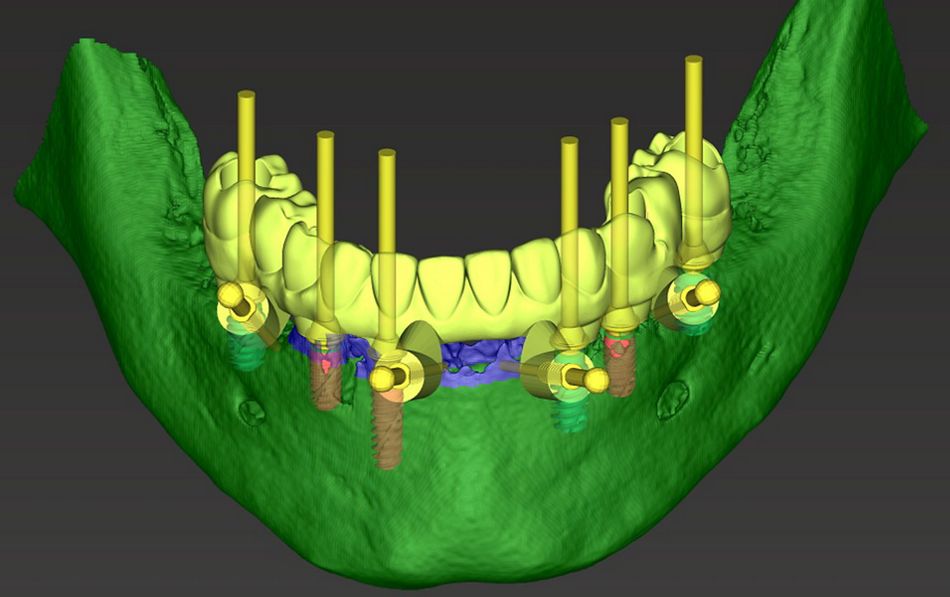
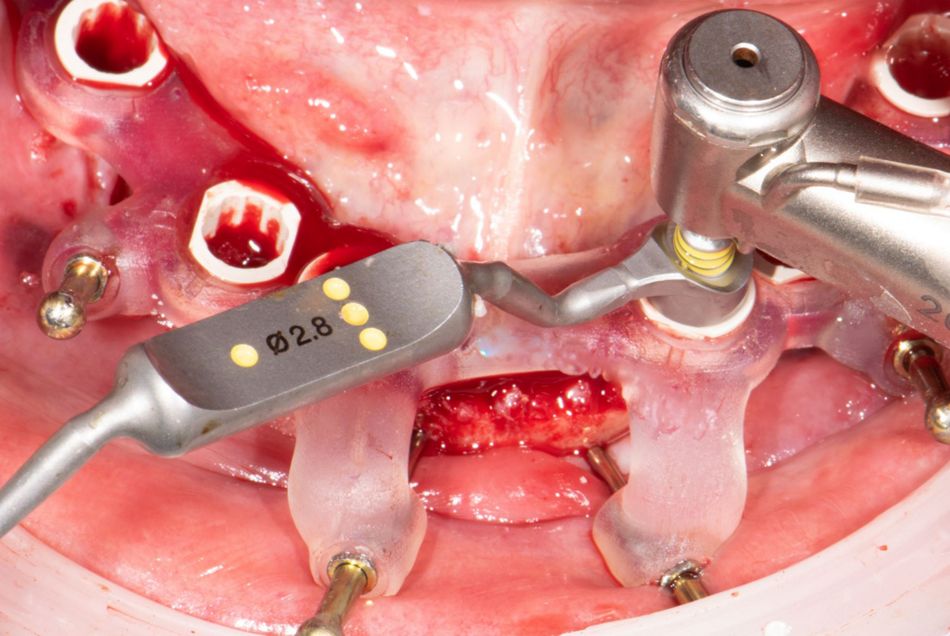
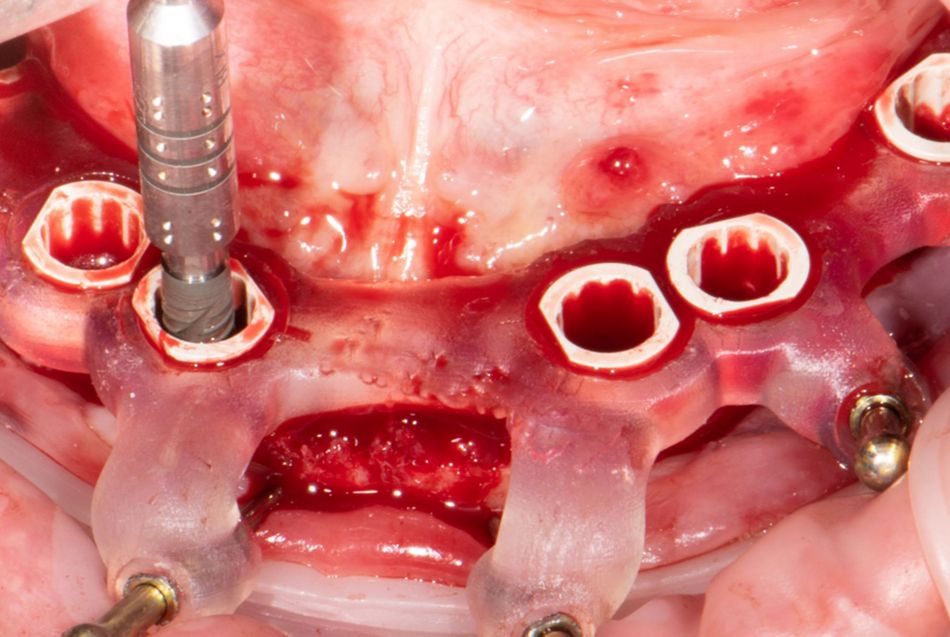
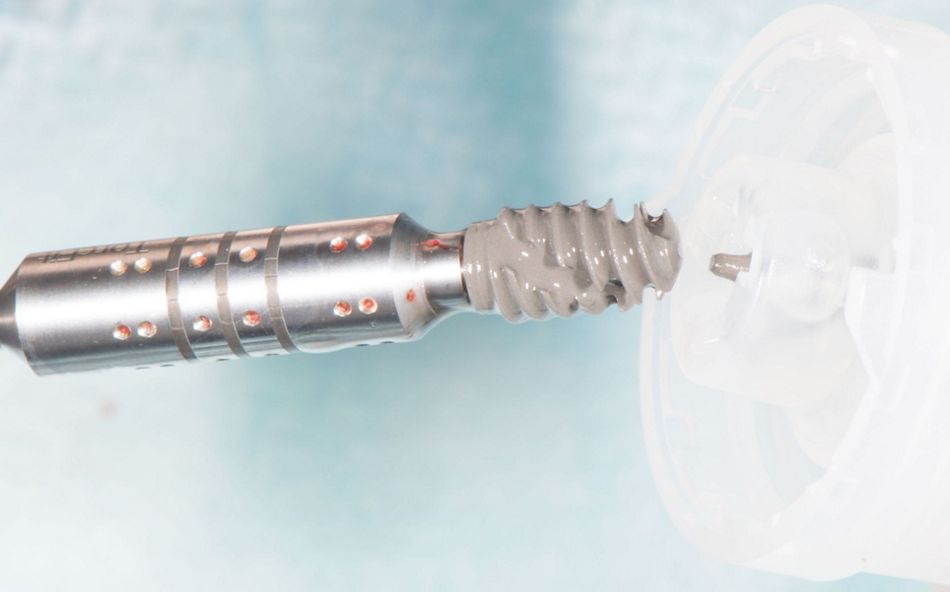
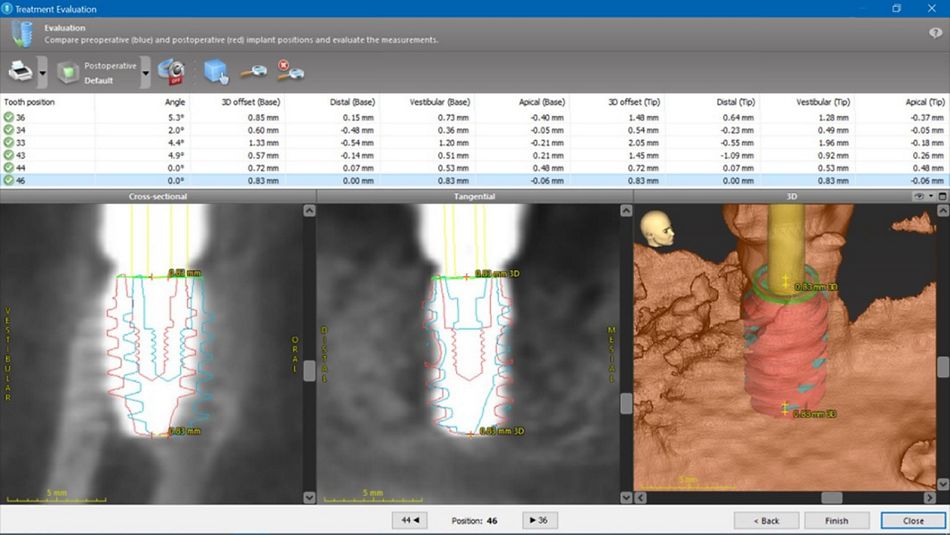
Treating patients with a Straumann® Pro Arch concept requires the procedure of immediate loading. In author’s opinion, in edentulous patients and patients with hopeless dentition it is also fundamental to place the implants with computer-guidance in prosthetically-oriented planned positions. There are several options to deliver an immediate prosthesis: either a conventional impression is taken for lab manufacturing, or conversion of a pre-existing or immediate removable denture. Both techniques are time consuming and depending on the material can carry risk of prosthesis fracture. In this case report the alternative treatment modality is presented. The new Smile in a Box TM service from Straumann can be used in a flexible way e.g. for creation of the provisional prosthesis by a centralized service and delivered on the day of surgery. It becomes possible with planning the case and treating the patient with digital technologies and aims to be beneficial in terms of clinical outcome, treatment time, but also of the durability of the material.
Initial situation
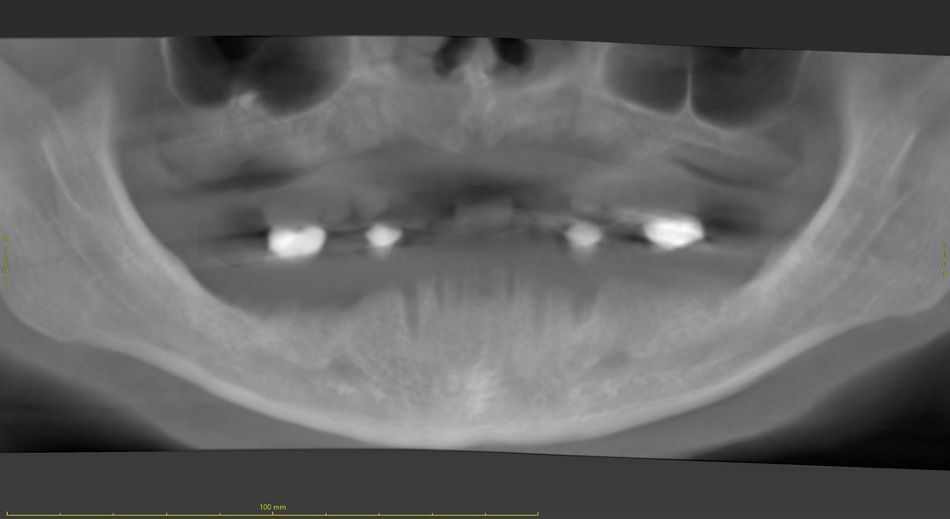
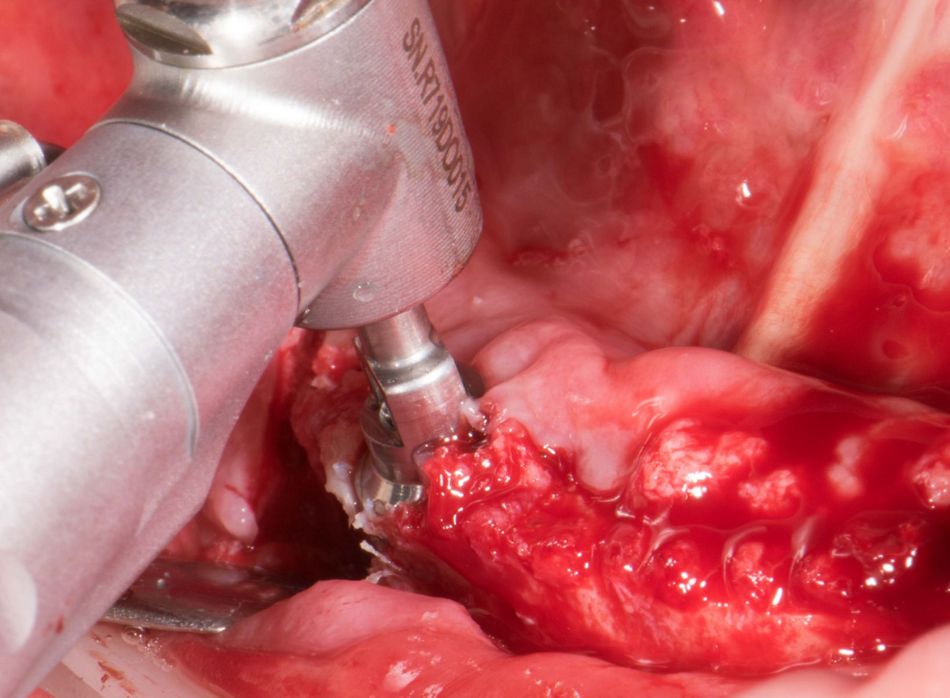
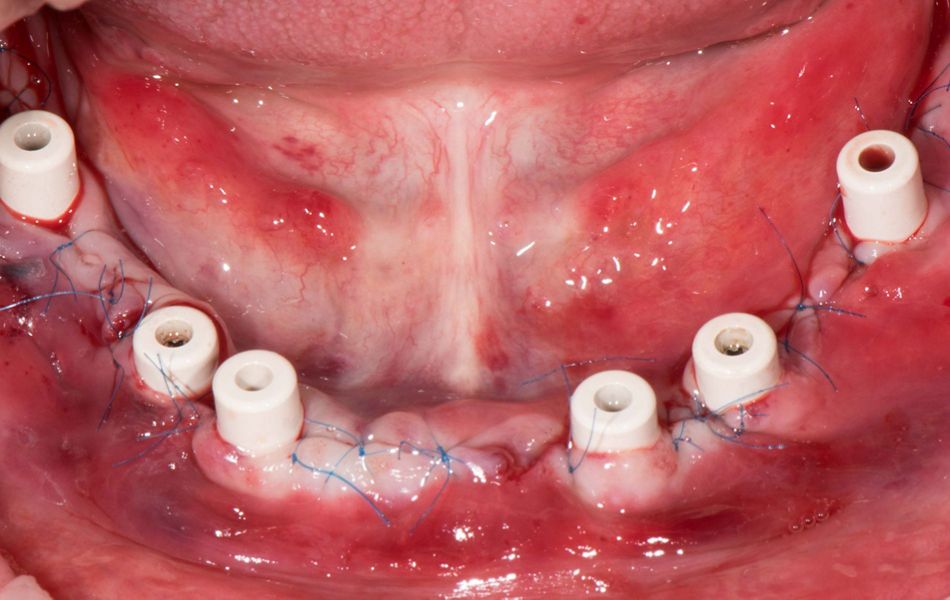
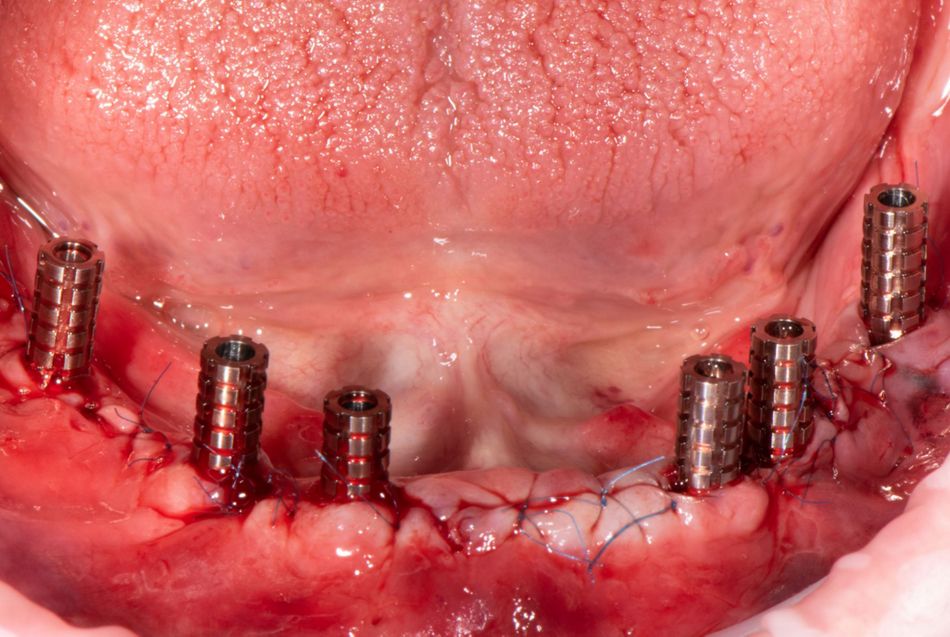
A 65 y.o. patient in good health required a full mouth rehabilitation. He presented with failing dentition both in maxilla and in mandible (Fig. 1). At this stage, the first CBCT was performed to evaluate the possibility of implant placement (Fig. 2). The situation in maxilla revealed an extremely thin crest which required large GBR procedures to place the implants; this treatment scenario was refused by the patient; a removable complete denture was chosen as a treatment option. While in the mandible bone conditions allowed placement of six implants and further restoring them with a fixed prosthesis. The tooth in the maxilla was out of the occlusal plane, and the teeth in the mandible were mobile, which did not allow the precise fit of a surgical template. So, it was decided to go for a staged approach. The remaining teeth were extracted (Fig. 3), and the patient then received immediate complete dentures for both maxilla and mandible.
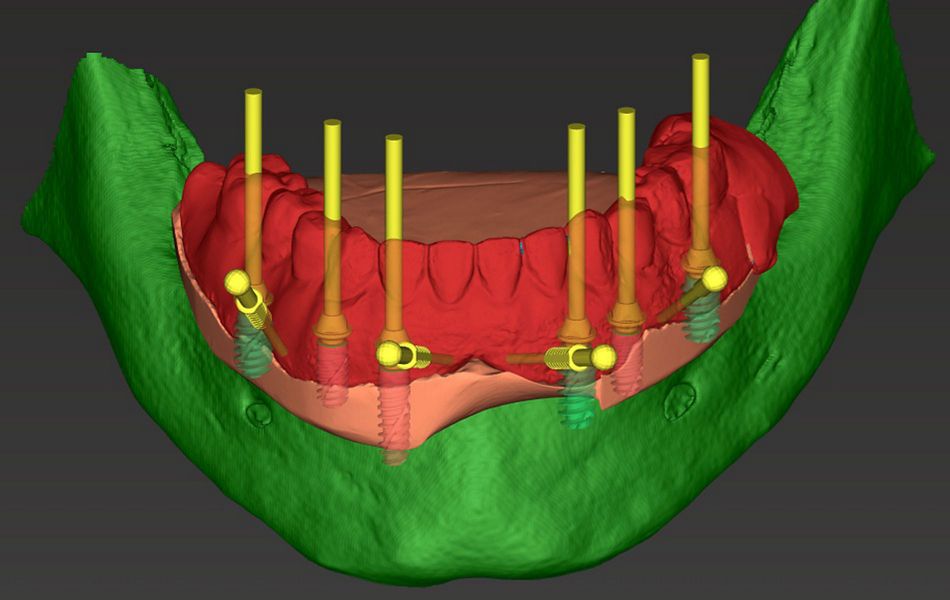
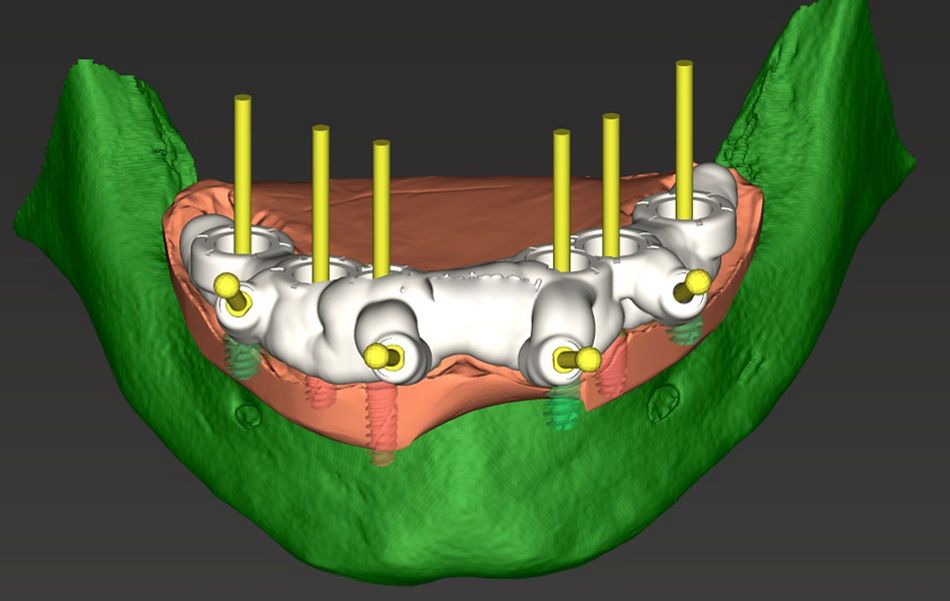
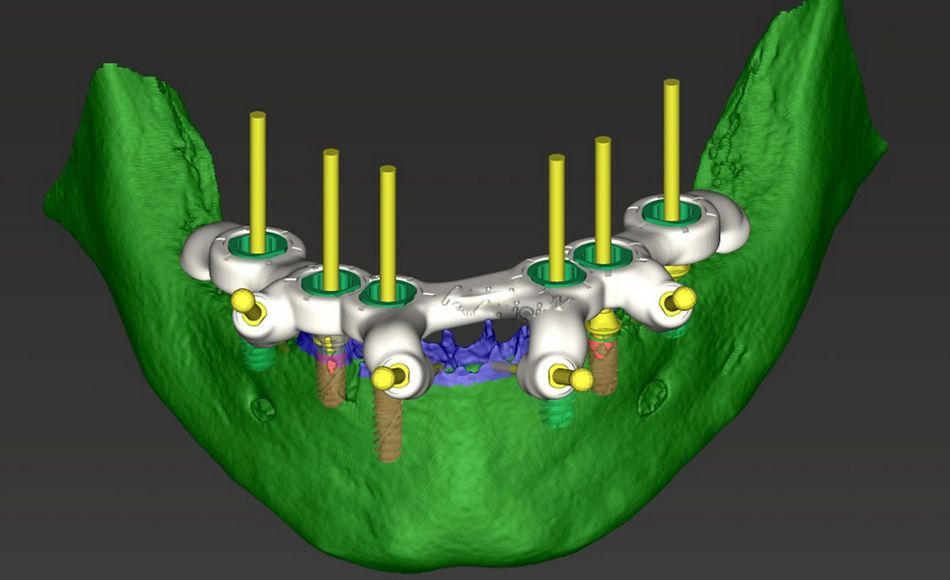
Treatment planning