Initial Situation
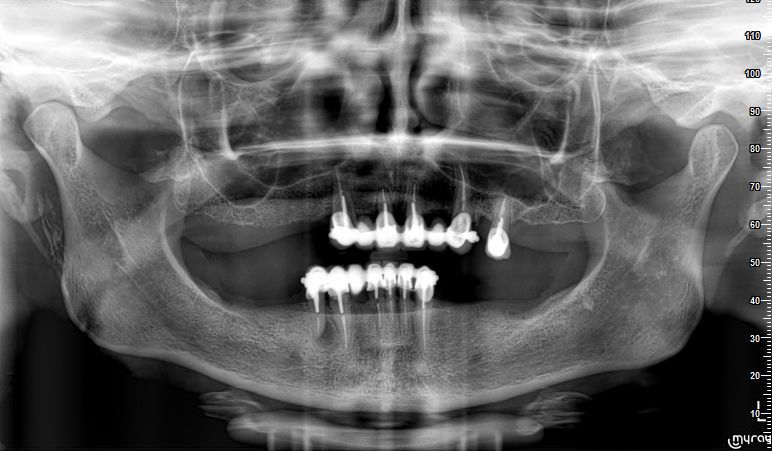
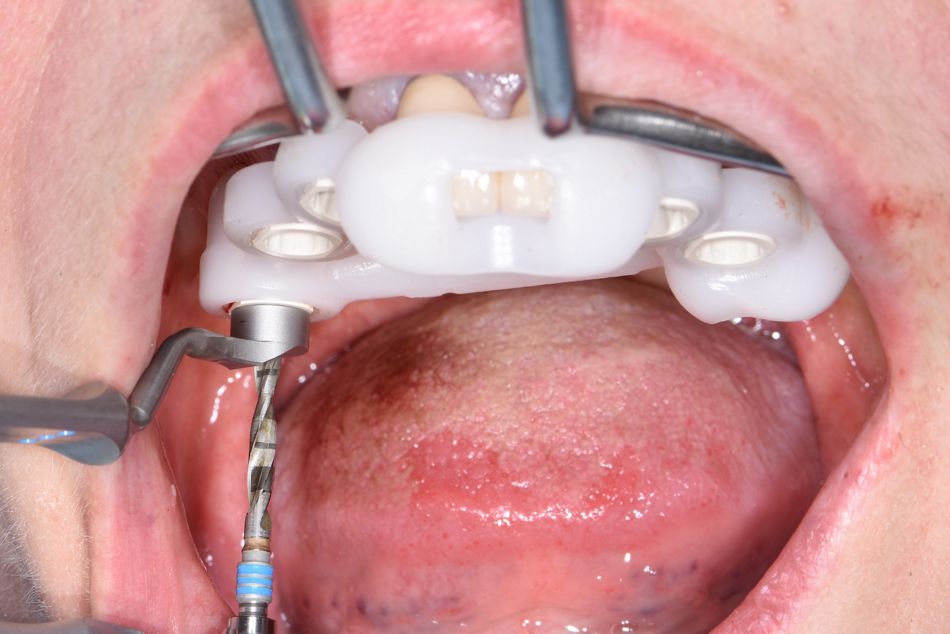
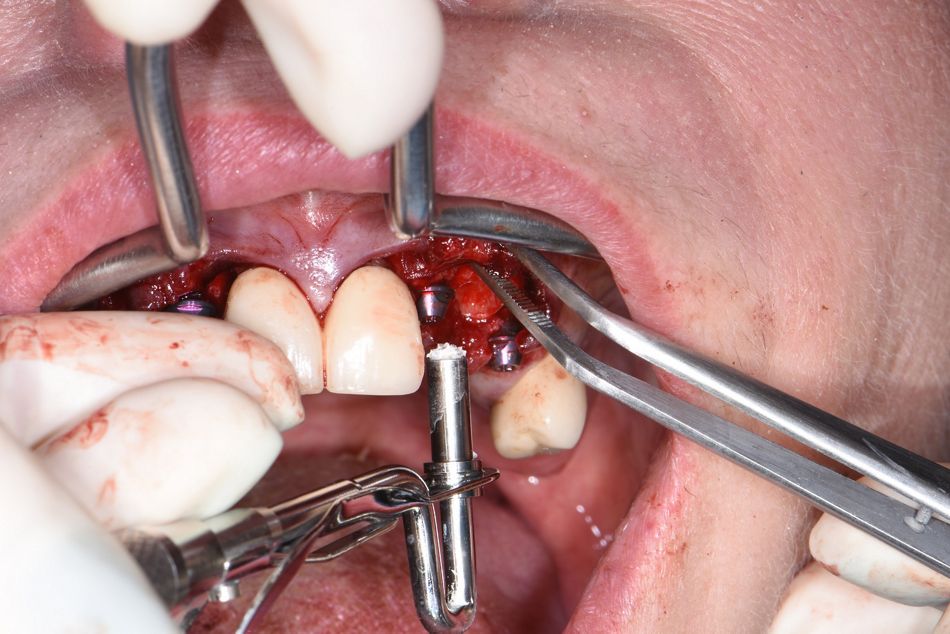
A 62-year-old patient presented to the clinic with a porcelain fused to metal (PFM) bridge supported by teeth #13, #23 and #25; and a partial removable denture (Fig. 1-2). The patient suffered from the constant de-cementation of the bridge due to severe secondary caries of the roots.
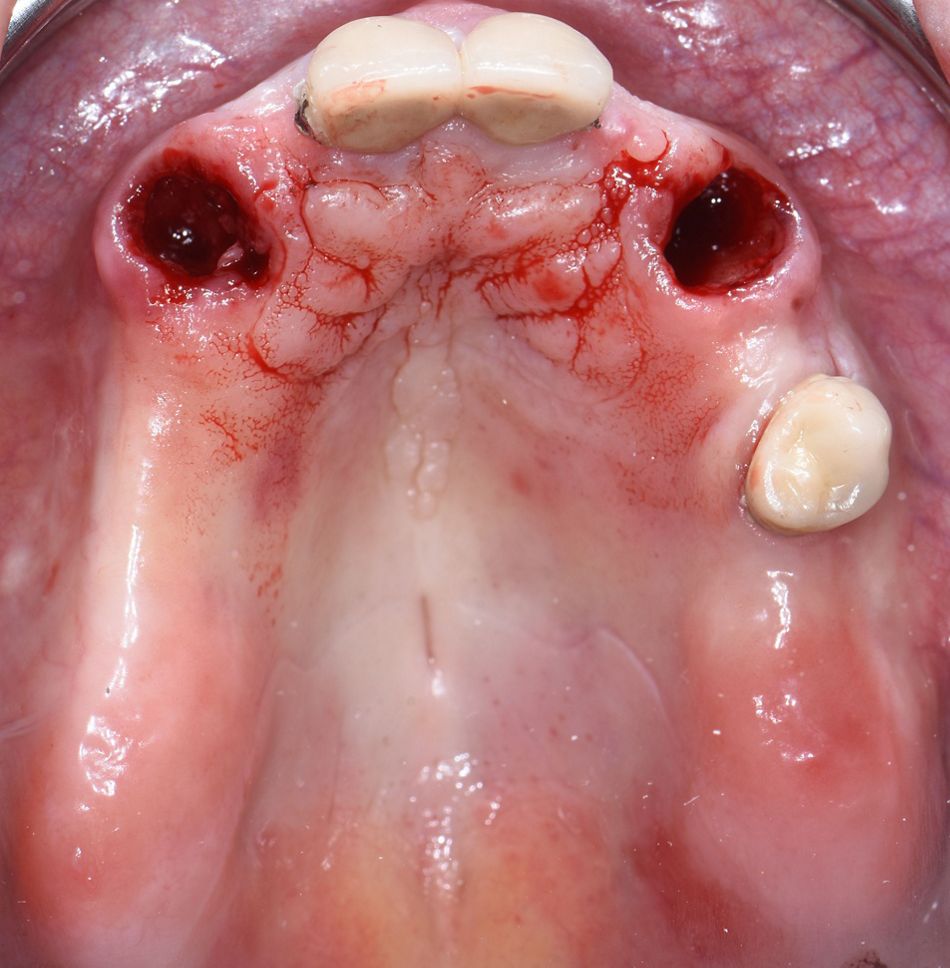
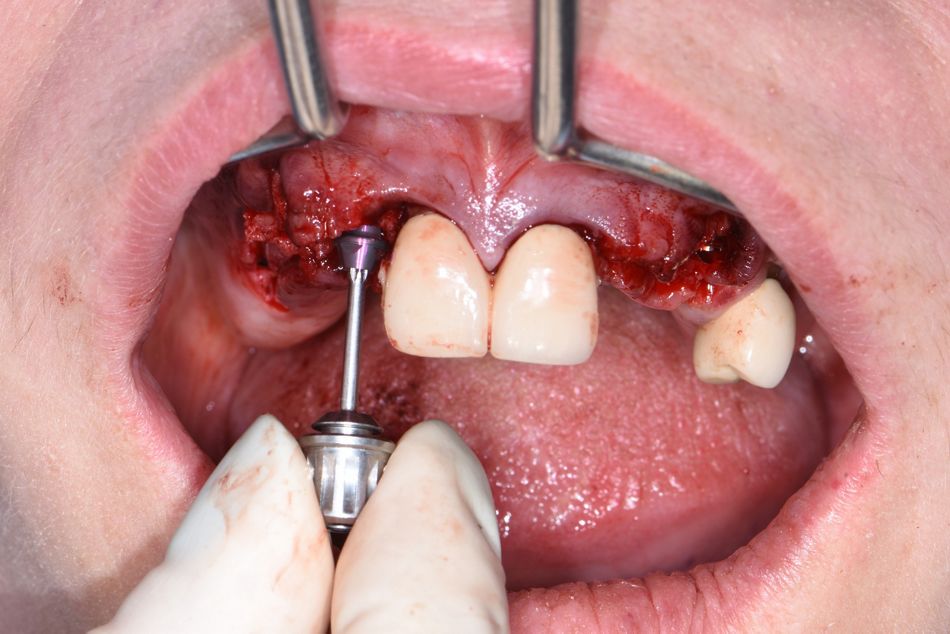
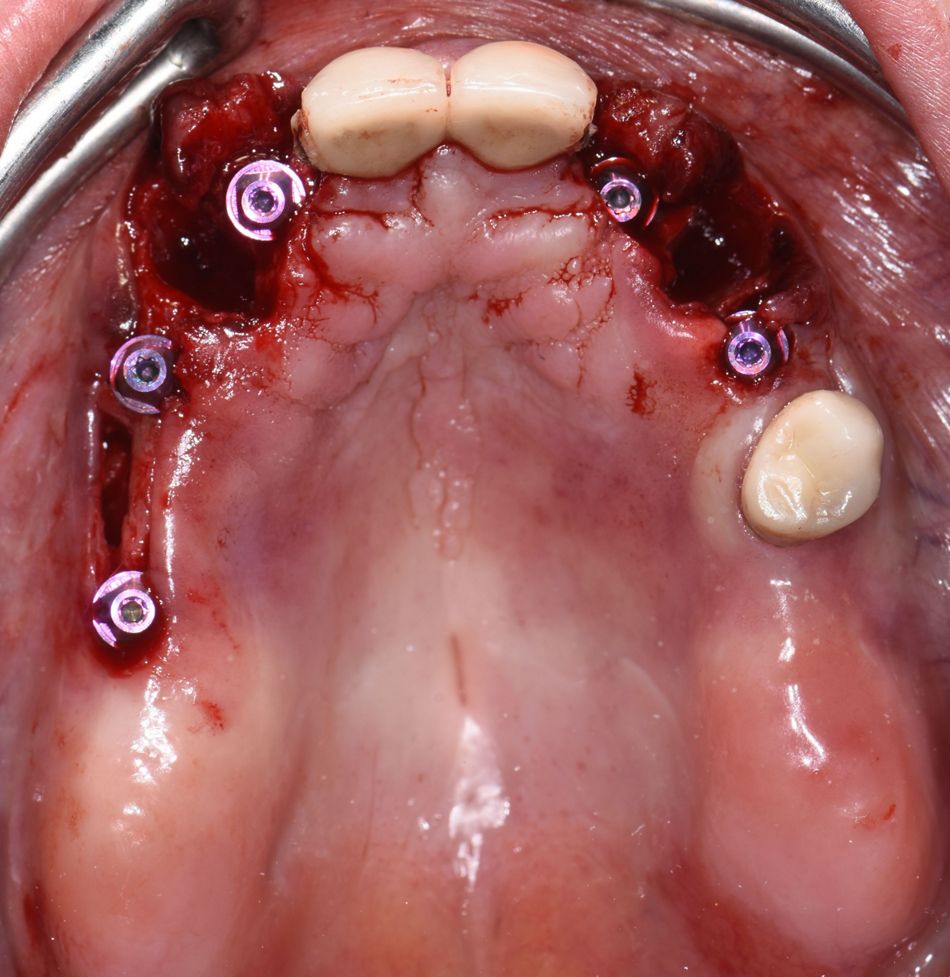
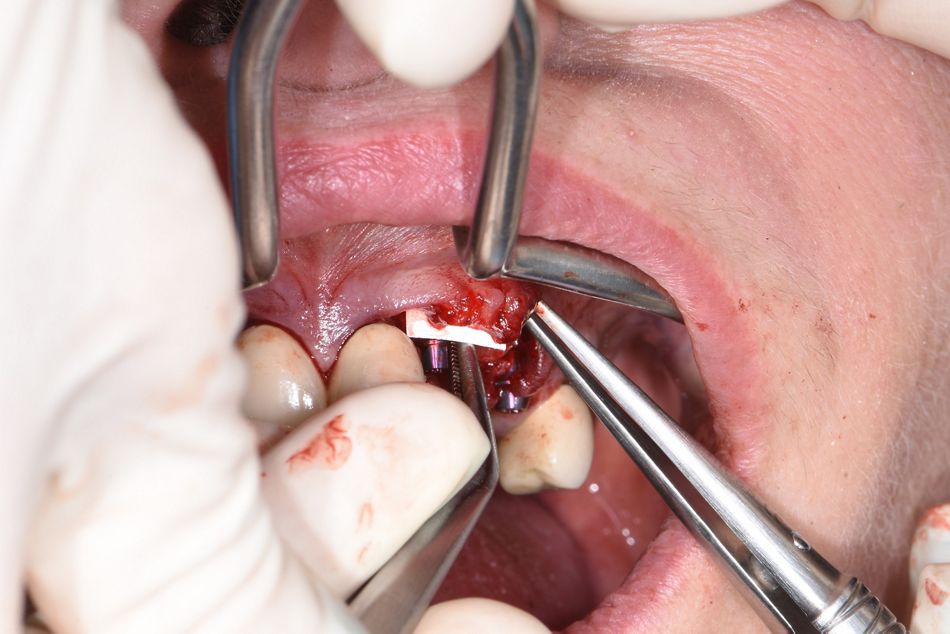
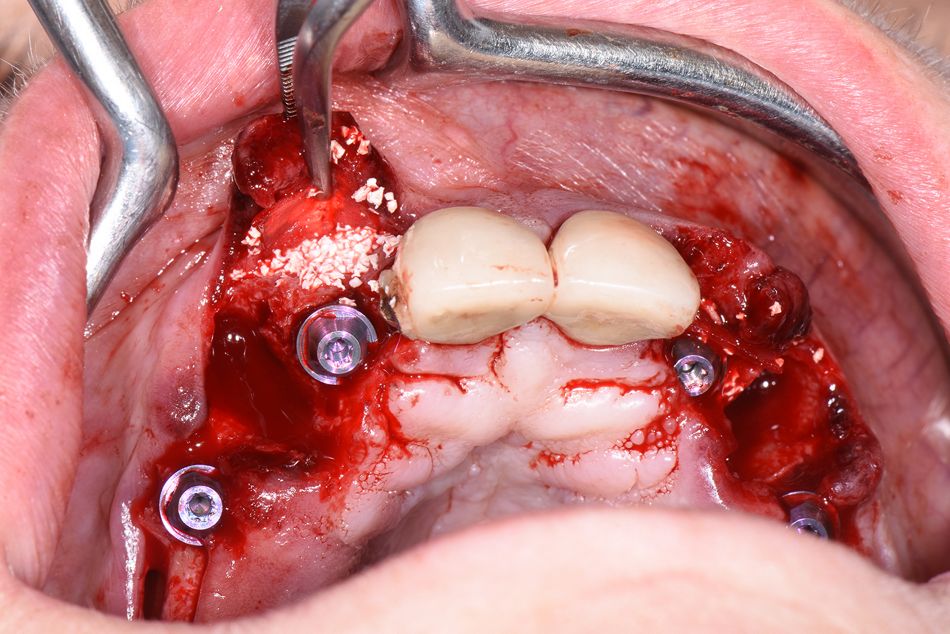
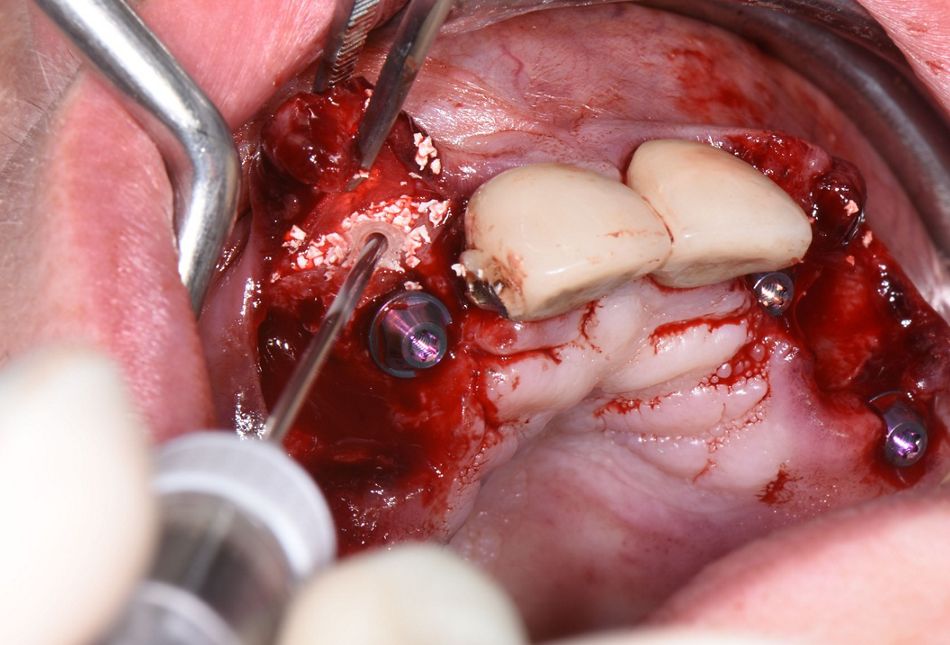
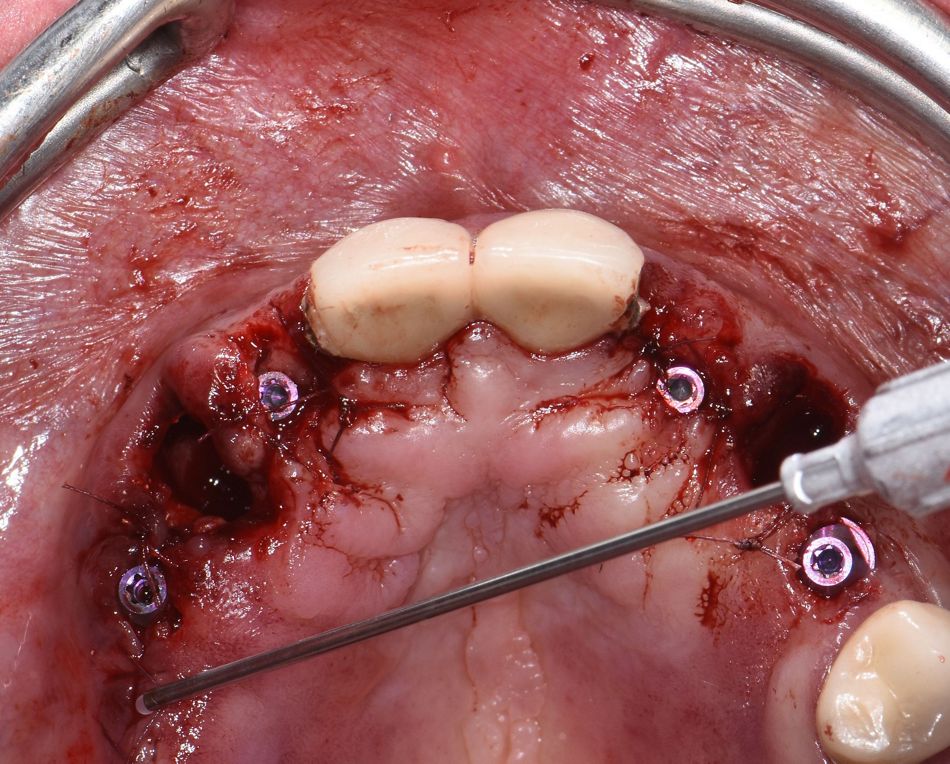
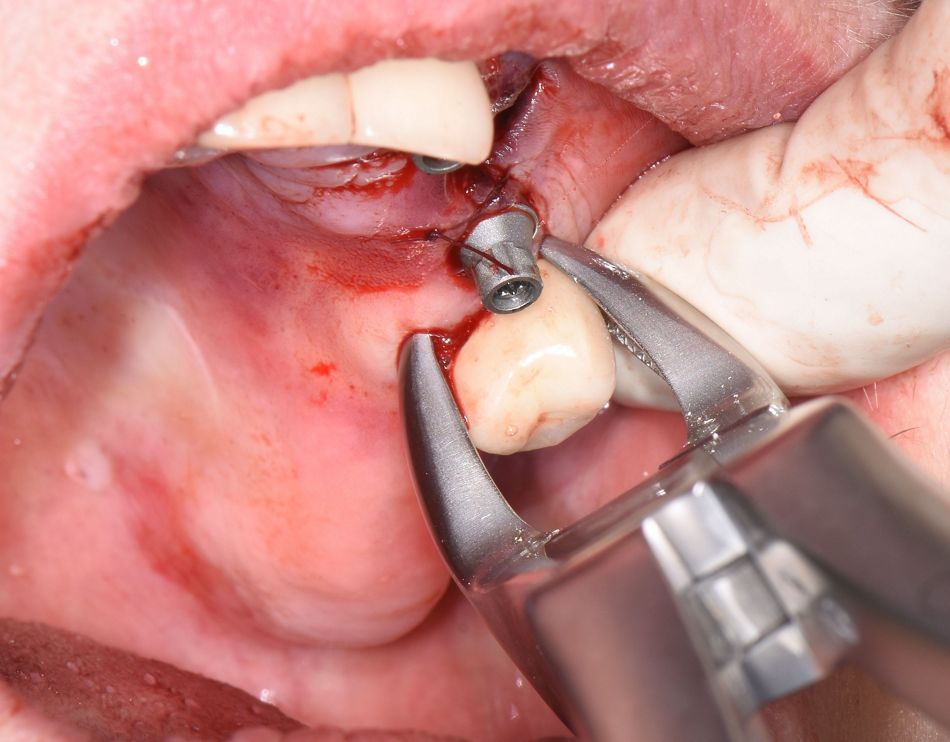
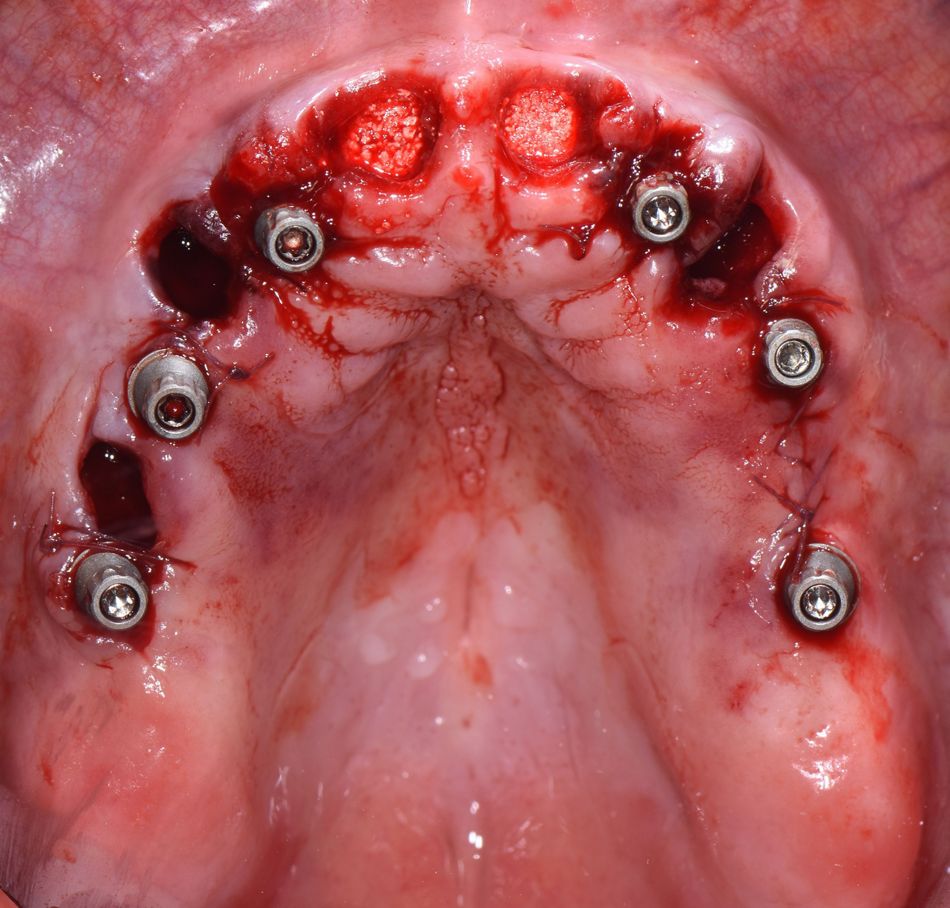
Following the clinical and radiological examination, remaining roots #13, #11, #21, #23 and tooth #25 were diagnosed with secondary caries beneath alveolar socket margin and grade 3 mobility (Fig. 3-4).
In the mandible patient was wearing a partial denture and a PFM bridge from teeth #33 to #44. In radiological examination, an image compatible with a periapical lesion was observed on tooth #44. Moreover, the prosthetic superstructure was unsealed and moving.
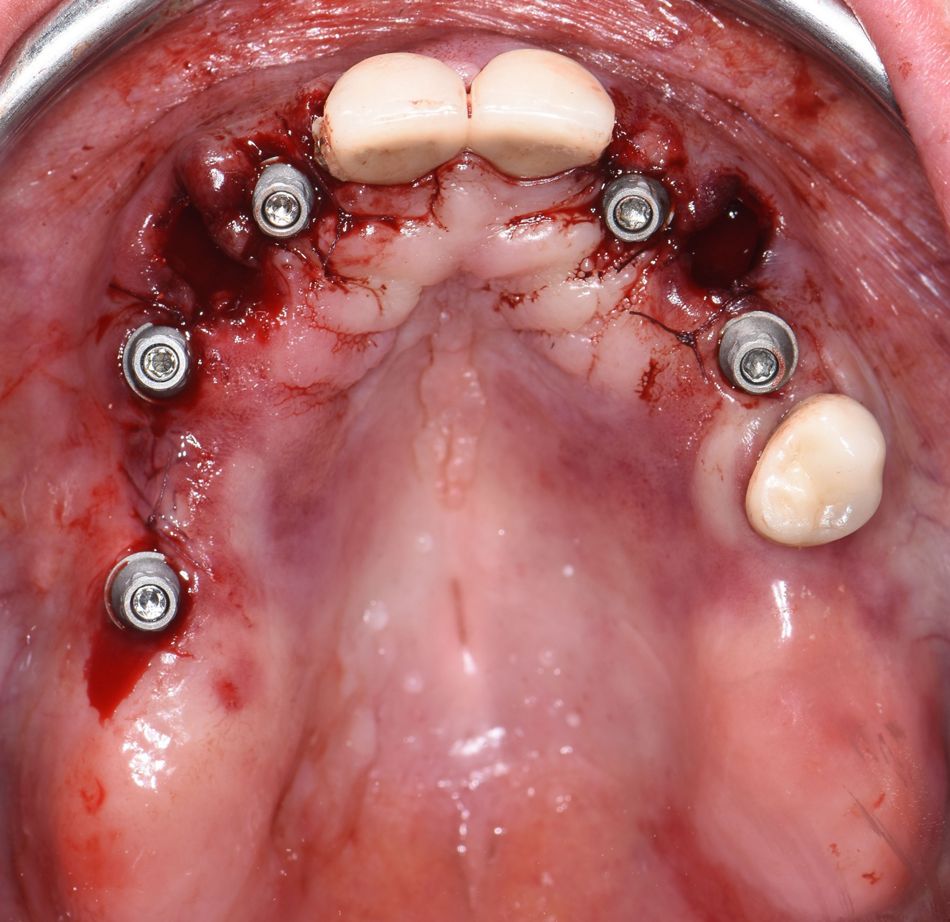
The patient was aware that her remaining teeth needed to be extracted, as she was diagnosed and presented to the different treatment options by the referring dentist. She wanted not only a fixed solution but also to maintain her teeth shape and smile. Furthermore, she highlighted her preference of not having an artificial gingiva in the fixed denture and to have the second incisors concavities refilled, as well as the lip support maintained.
Treatment planning
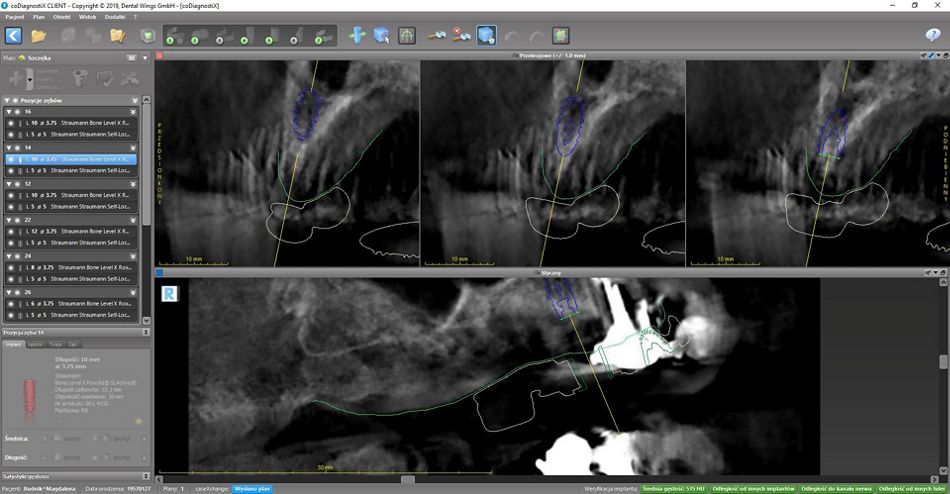
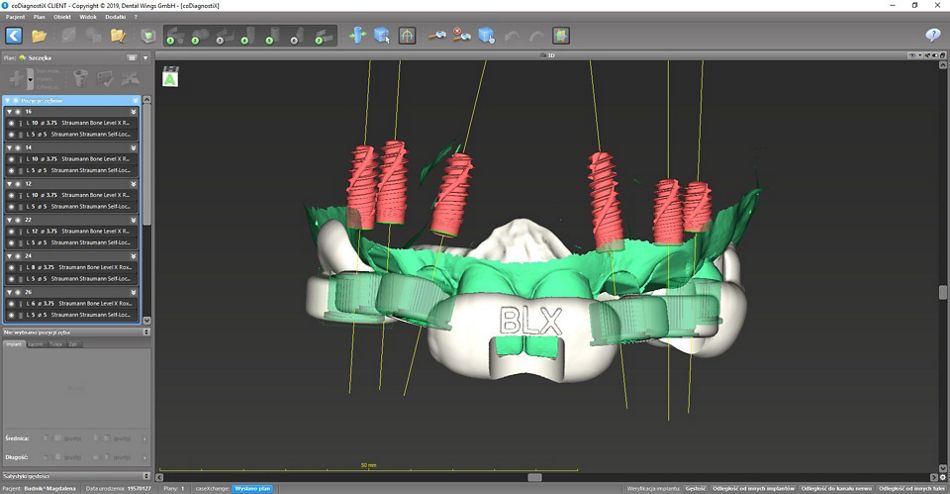
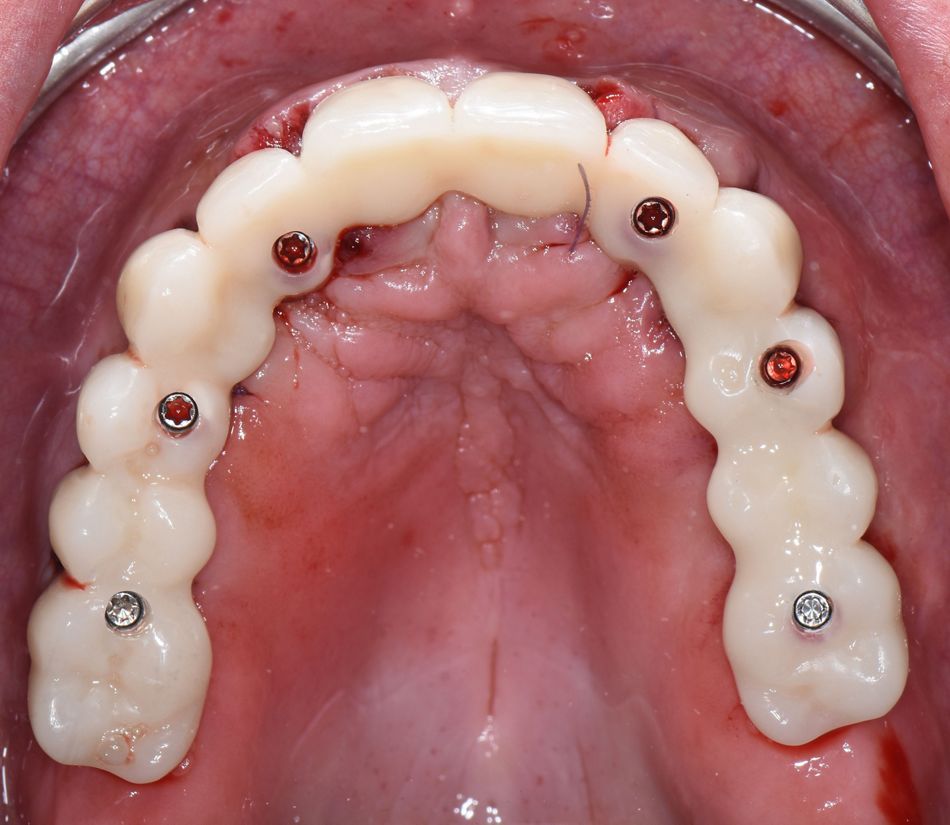
Patient have had cone beam computed tomography (CBCT), intraoral scanning and photo portfolio for digital smile design (DSD) to prepare the treatment planning. CBCT and intraoral scans were used to plan the implants positions with coDiagnostiX® software (Fig. 5-6). The implants positions were planned in optimal prosthetic positions so the implant axes would be either on occlusal or palatal side of the future bridge. Due to reduced bone height in the posterior region, the implant in the site #26 was planned 6mm length and in #16 site 8 mm length. In order to obtain optimal primary stability, Straumann® BLX implants were planned. Moreover, to achieve an ideal mechanical distribution, implants in the positions of second incisors, first premolars and first molars were planned. Following the digital treatment planning in coDiagnostiX®, the surgical guide was 3D printed (Fig. 7).