In these clinical scenarios, ZAGA Concept recommends to buccally displace the osteotomy with the aim of sinking the implant neck/body as much as possible into the alveolar and lateral maxillary wall bone while maintaining the sinus lining integrity with no membrane perforation at the crest level. This type of osteotomy, not capable of providing a complete covering of the implant mid-body and neck is known as “Canal Osteotomy''. It is a groove made on the coronal alveolar bone, and sometimes also in the lateral maxillary wall and zygomatic buttress. As a waterway or channel; it has a floor, lateral walls with different heights and no roof. When a “Canal Osteotomy” is performed, the maxillary bone is not covering the buccal zygomatic implant mid-part, nor its neck.
This approach belongs to the ZAGA Concept recommendation, and its rational is based on the fact that the implants with minimal crestal bone surrounding their entry point may present bone resorption under function and within time with a subsequent oral-antrum fistula. Indeed, deficient bone to implant contact (BIC) may be jeopardized by different circumstances i.e. periodontal disease history, inadequate oral hygiene, use of water pressure devices at the gingival junction, inadequate use of the dental probe, etc. Moreover, it has been speculated that the lack of crestal bone support would end up in a transversal mobility of the long coronal part of the zygomatic implant facilitating an oral-sinus communication.
Placing the zygoma implant platform partially or outside of the sinus, and with a lateral maxillary bone support/contact; would allow a better prosthetic positioning together with a more conservative approach regarding the sinus integrity preservation. In order to prevent soft tissue dehiscence when placing the implant laterally to the maxillary wall, it is recommended to groove the buccal bone to house the implant body with as much lateral submergence as possible into bone, in such a way that it does not protrude against the mucosal position and does not compress the soft tissue vascularity. The depth limit for the canal digging is the sinus membrane integrity at this level. The use of a channel section implant adapted to this osteotomy type i.e. the Straumann ZAGA Flat, would help the surgeon to prevent soft tissue complications.
The present case report is intended to demonstrate how a bony canal having section in the shape of an arc of circumference, would optimally be sealed by an implant showing a circumferential arc section as well. Each step of the procedure will be illustrated with figures showing the insertion of a flat zygomatic implant section that fits into a channel with a minimal buccal impact against the soft tissue.
Initial situation
A 75-year-old female patient presented to our office with the chief complaint of deficient chewing function and poor aesthetics. Regarding her medical condition, she reported not suffering systemic diseases and not taking any medication.
The clinical assessment in the upper jaw showed the presence of hopeless teeth on positions #13, #12, #11, #21, #22 and #23, with advanced chronic periodontitis and atrophic ridges on the posterior areas. On the other hand, in the lower jaw she presented an implant on position #43 supporting a failing partially removable prosthesis.
The radiographic assessment depicted an extreme bilateral bone loss on both premolar and molar regions at the upper and lower jaws. Furthermore, a horizontal bone loss in the anterior area on both upper and lower arches was presented.
The patient expectations were high, and she requested a short-lasting therapy avoiding large bone augmentations with an immediate fixed prosthesis at her upper and lower jaws.
The decision was done in favor of the extractions of all remaining teeth which were considered hopeless and immediately followed by the complete rehabilitation of the upper and lower jaws a with fixed prosthesis anchored on oral implants.
Treatment planning
The treatment decision-making process was based on impressions and casts from the upper and lower jaws using a SAM dental articulator, the radiographic assessment (X-rays & CBCT) and a digital planning software (Figs. 1- 4).
Following a careful evaluation; it was planned to perform in the upper jaw a Hybrid Zygoma approach (4 dental-implants and 2 zygoma-implants), that included a ZAGA surgery with two ZAGA flat implants of 40 mm length on the right side and 42.5 mm length on the left side (advanced), four conventional dental implants, a periodontal plastic surgery (pediculated connective scarf graft) and an immediate fixed restoration consisted on a screwed retained provisional bridge. Moreover, in the lower jaw five conventional implants with an immediate screw-retained fixed restoration were planned.
According to our standard protocol, the final restorations were delivered six months after surgery.
- Fig. 1 UR 15 Virtual (extra-sinus planning) Radiographic cut on 2 and 3D visions representing a simulation for an extra-sinus path of the right implant. According to the ZAGA Concept, when facing anatomical situations showing less than 4-5 mm of bone at the sinus floor level, a more reliable bone sealing at coronal level is achieved by buccal shifting of the osteotomy. As illustrated, the coronal BIC surface increases from 1,7 to 7 mm. Antrostomy position is apically displaced and sinus lining integrity is respected.
- Fig. 2 UR 15 Virtual (intra-sinus planning) Radiographic cut on 2 and 3D visions representing a simulation for a classic intra-sinus path on the patient of fig 1. An eventual circular “tunnel osteotomy” would reach the sinus through scarcely 2 mm of alveolar bone thickness. ZAGA Concept recommends visualizing the possibility for development of future oral-antral fistula.
- Fig. 3 UL 25 Virtual (extra-sinus planning) The virtual planning of the left side represents a ZAGA type 4 situation. By a lateral displacement of the osteotomy an increased titanium to bone contact is achieved while maintaining sinus lining integrity.
- Fig. 4. UL 25 Virtual (intra-sinus planning) The virtual planning of the same patient and hemimaxilla of the fig. 3, is showing an intra-sinus path. Possibility for late peri-implant bone resorption and oral-antral fistula must be foreseen. Patient related factors like periodontal history or smoking habits must also be considered for decision taking.
Surgical procedure
The whole procedure was conducted under full narcosis. The hopeless teeth were extracted and a mucoperiosteal flap was elevated by means of supracrestal and three vertical incisions in the tuberosity regions and the midline. These incisions enabled the flap mobilization beyond the infraorbital margin.
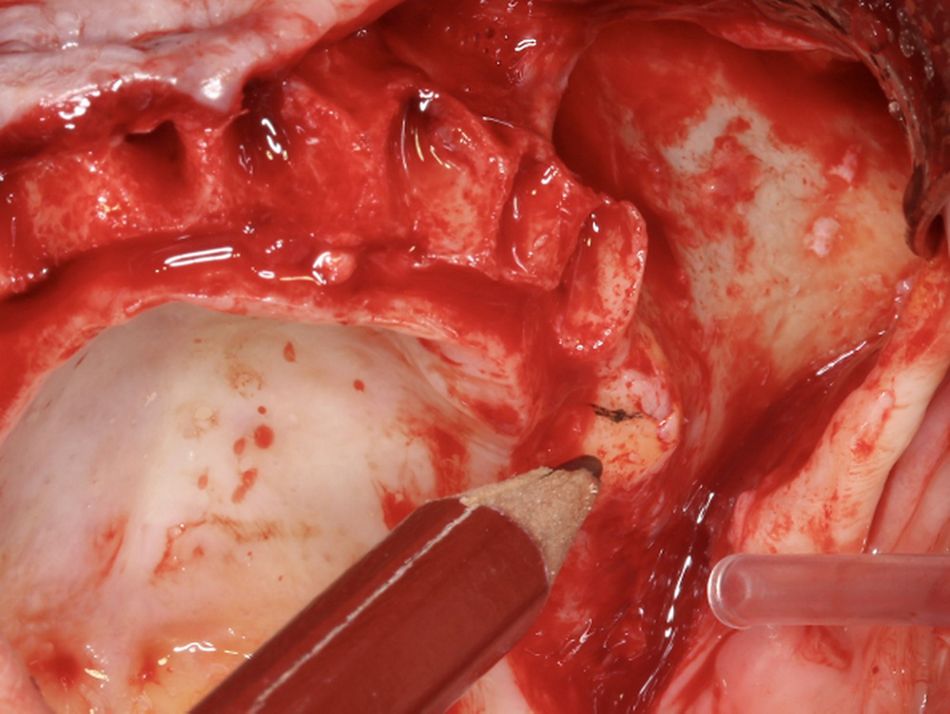
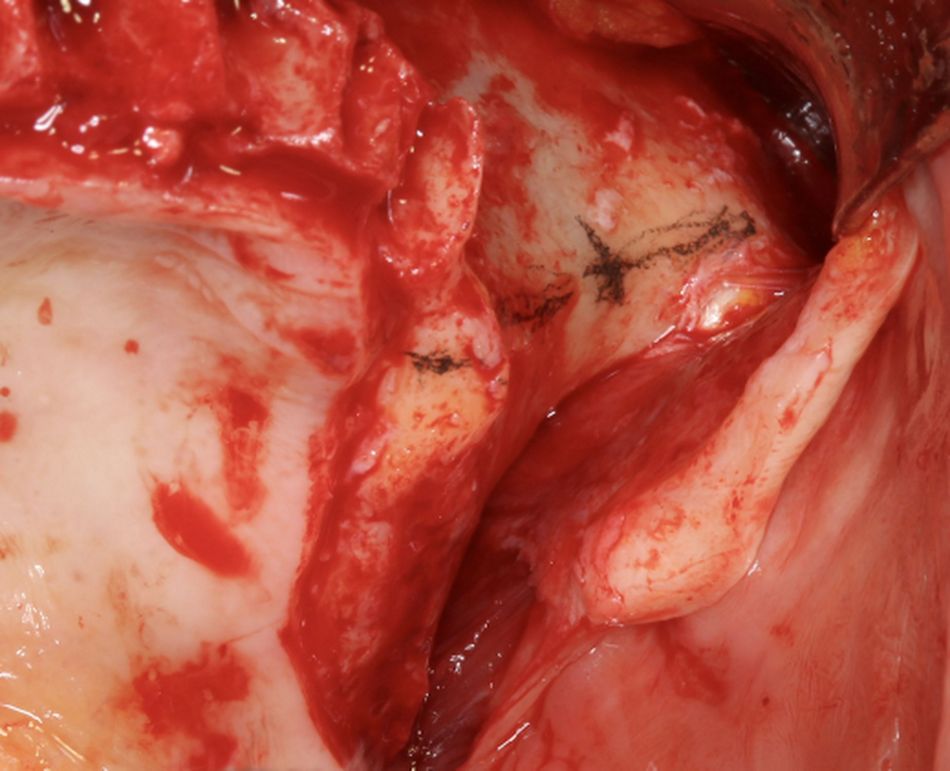
The surgeon’s first act after raising the flap should be to mark with a surgical pencil the reference points for the alveolar and zygomatic bone entrances. Therefore, these coronal and the zygomatic entrance points on the left second premolar/first molar position were pointed according to the virtual planning (Figs. 5 & 6).
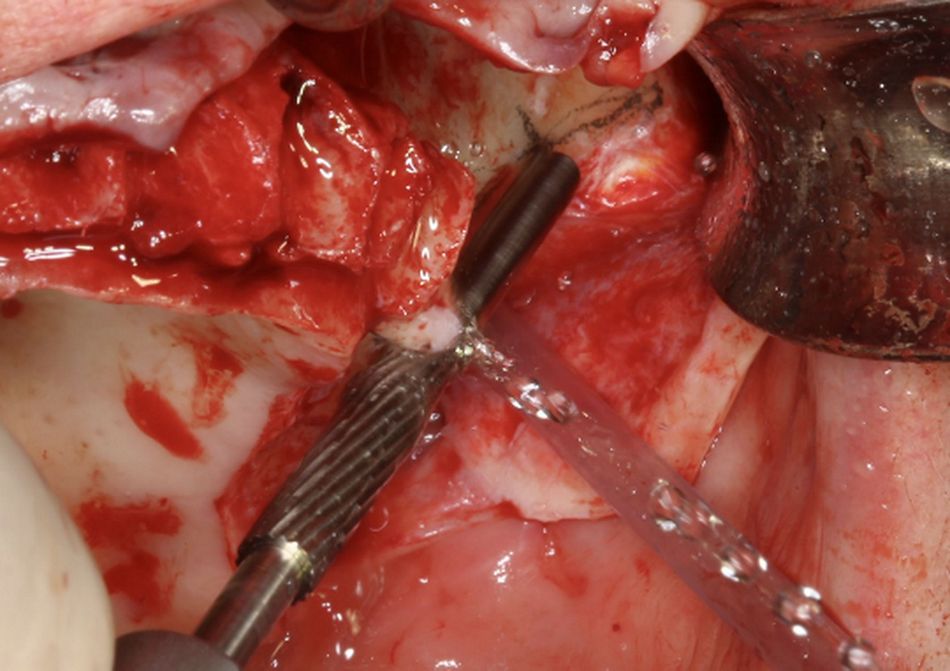
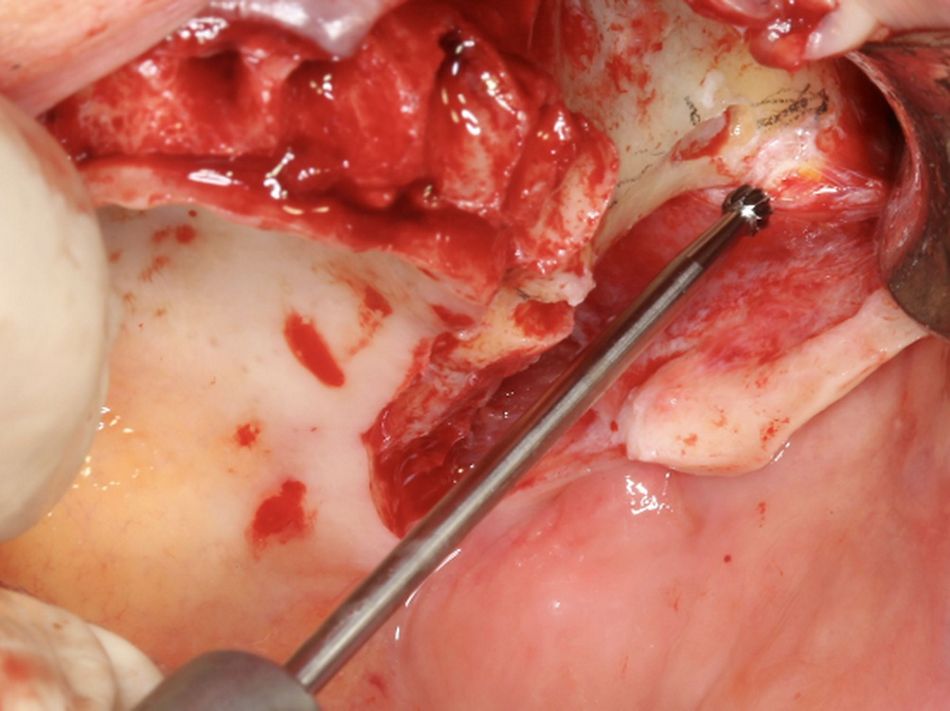
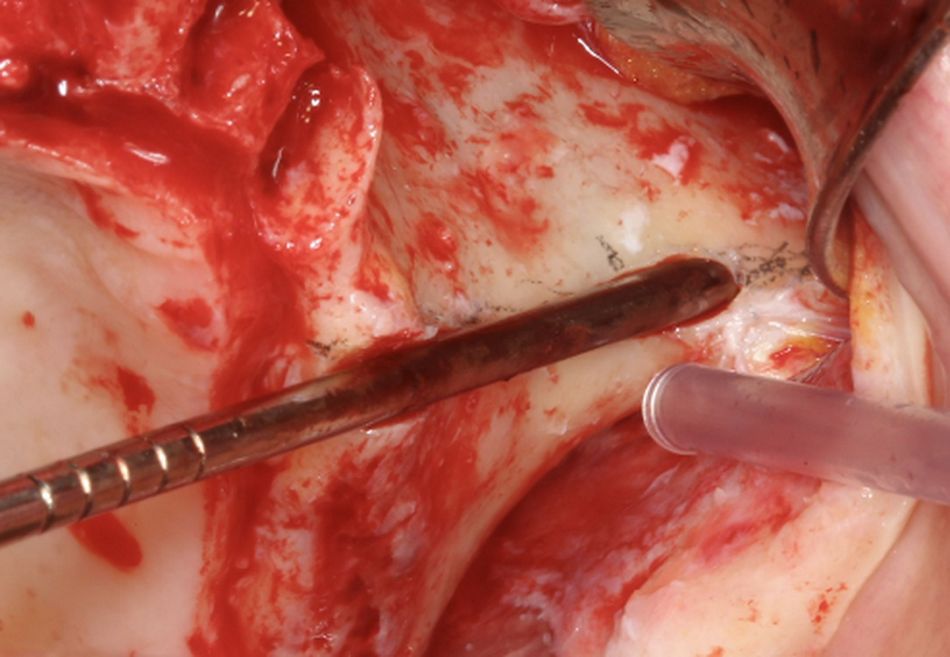
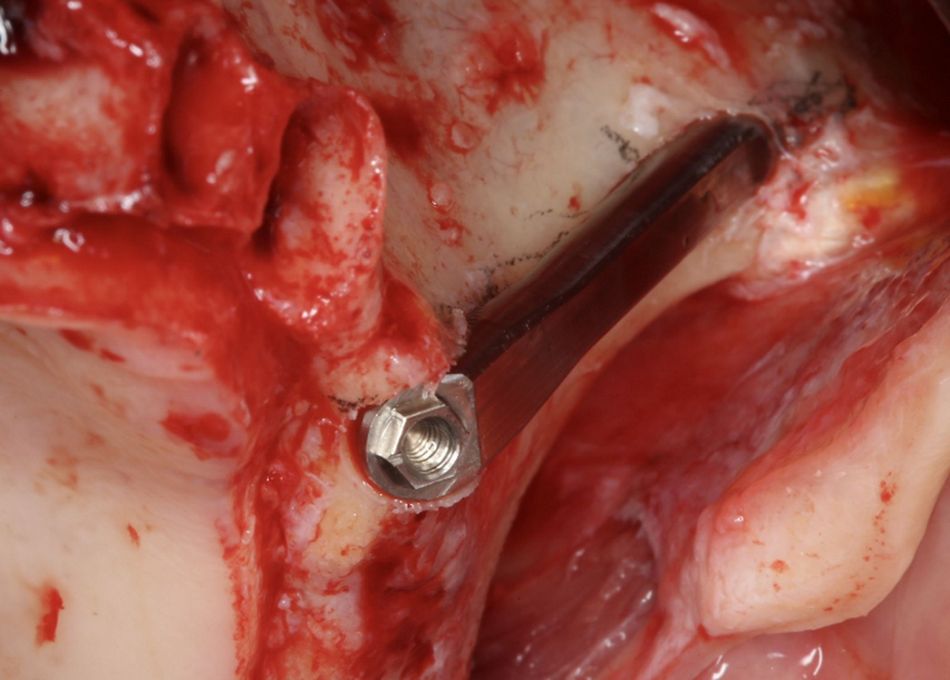
As the alveolar thickness was less than 4 mm, a “tunnel” osteotomy was not recommended. The drilling protocol consisted on the use of the lateral cutting bur help to initiate a canal and where the next drill tail will slide. The canal diameter was still reduced at this stage in order to precisely embrace and guide the next bur tail. It is important to take into consideration that just the first part of the lateral drill is used to initially prepare a channel with a diameter congruent to the round bur tail (Fig. 7).
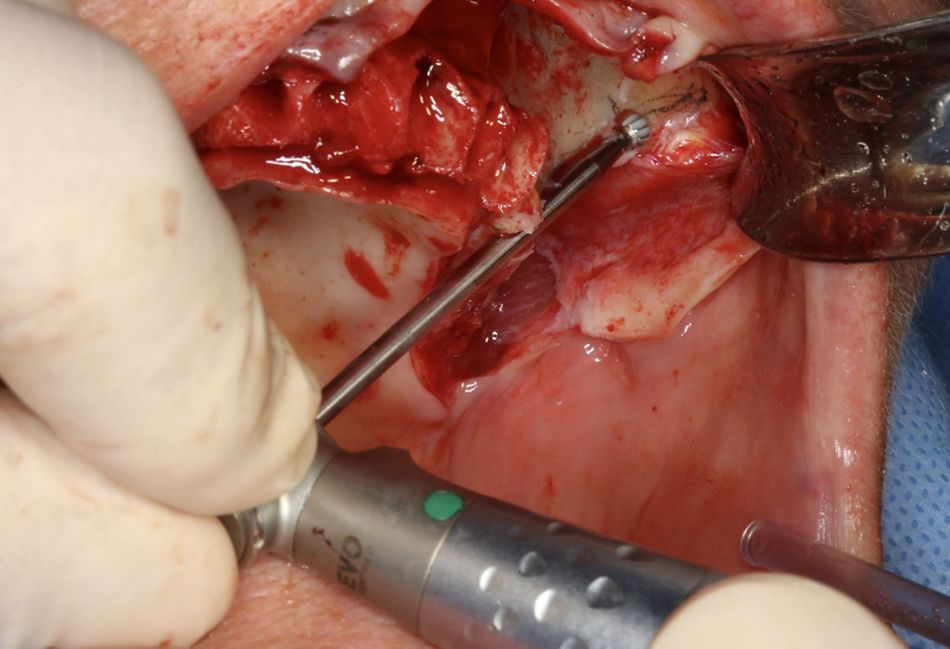
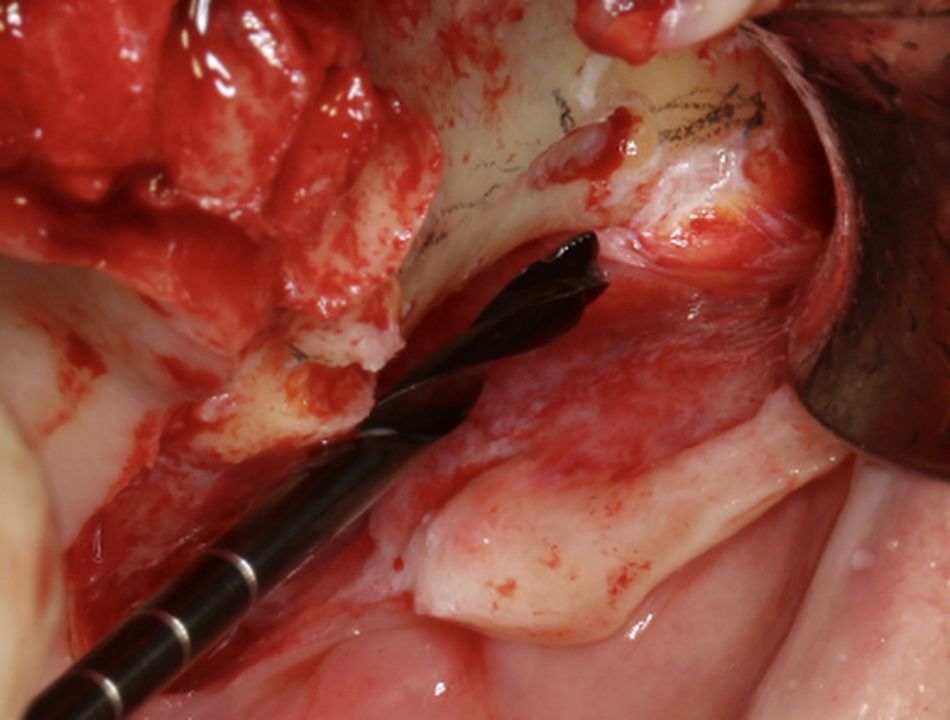
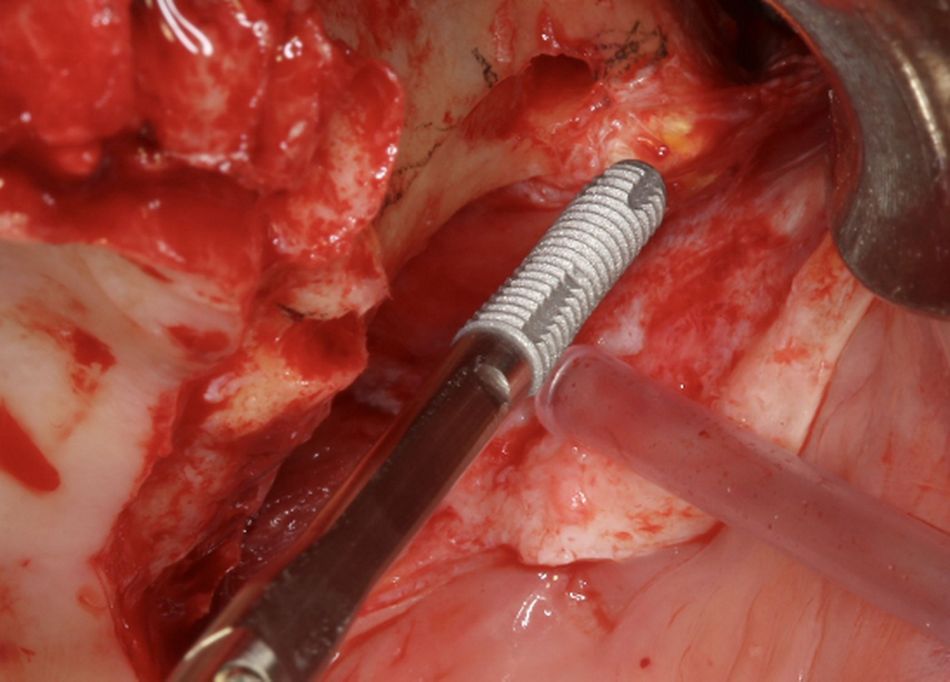
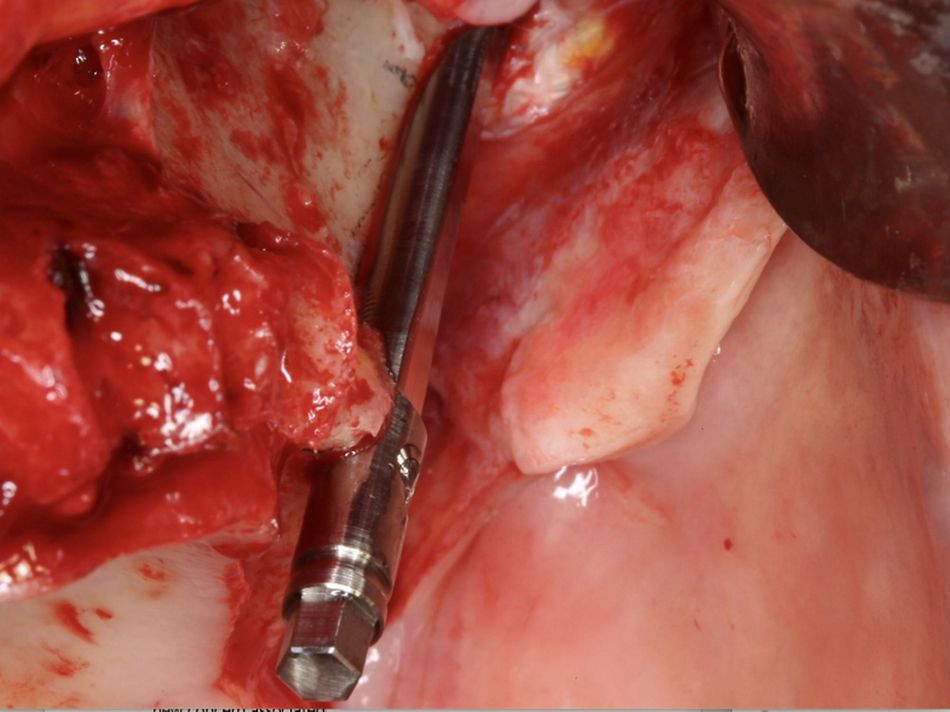
The slight adaptation of the lateral bur allowed the use of a round bur, which was supported by the alveolar channel. In this stage; the direction, depth and the inclination of the future implant trajectory was evaluated. Once the channel showed the desired depth and the floor surface became even, the round bur tail slid up and down gently. The grinding with the round bur becomes more precise by gently touching the bone during the slide down movement and by a “grinding-back” movement the round bur is able to eliminate the channel floor irregularities (Figs. 8 & 9).
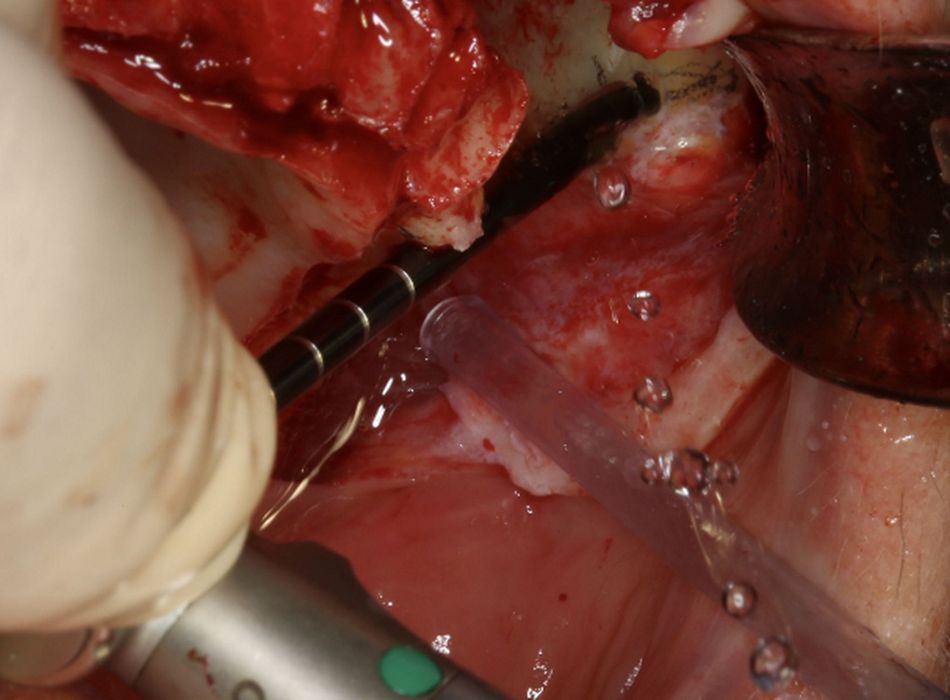
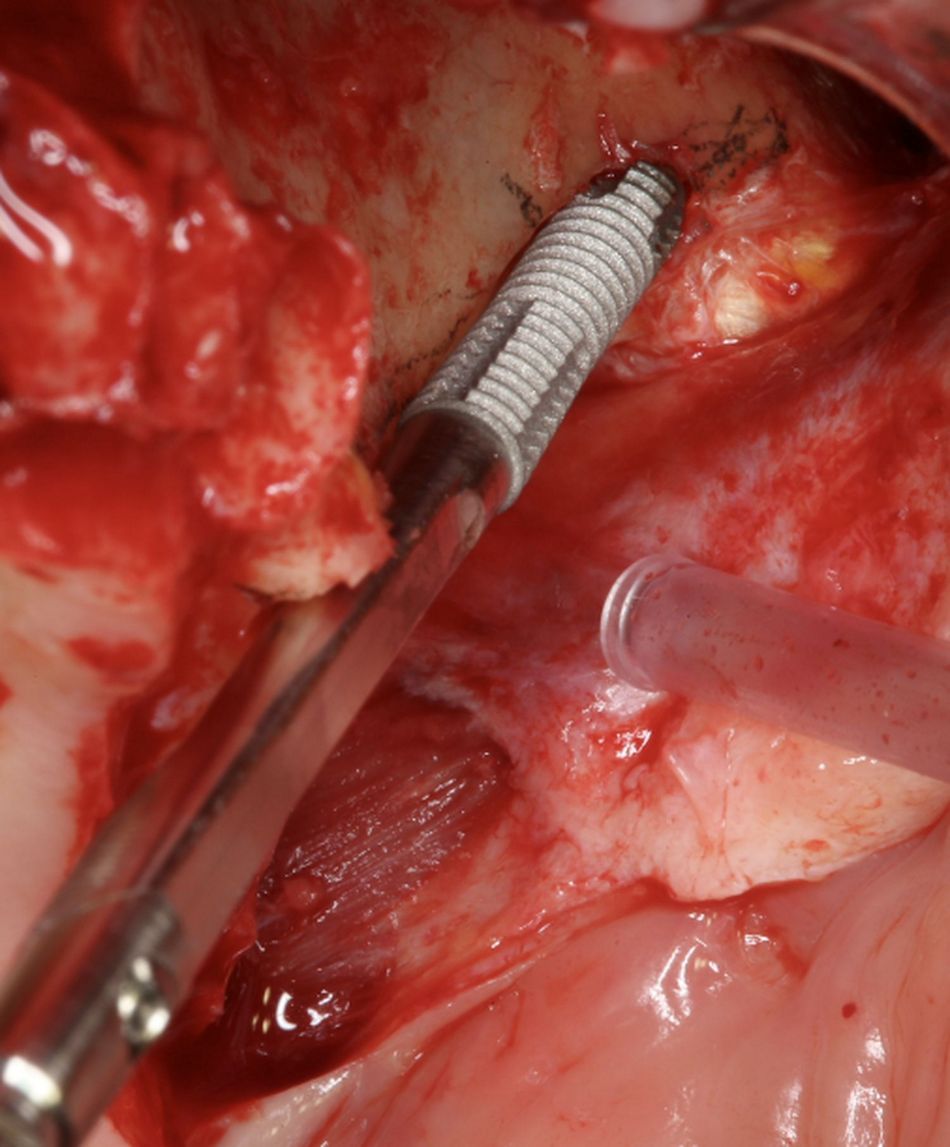
Once a zygomatic notch was prepared; the channel was evaluated in order to ensure a homogeneous floor, desired inclination and depth. For the final drill diameter, a Ø2.9mm twist drill was used with profuse irrigation and with up and down movements, using short pressure periods of about 4 seconds, allowing the saline to clean and cool the drill (Figs. 10 & 11).
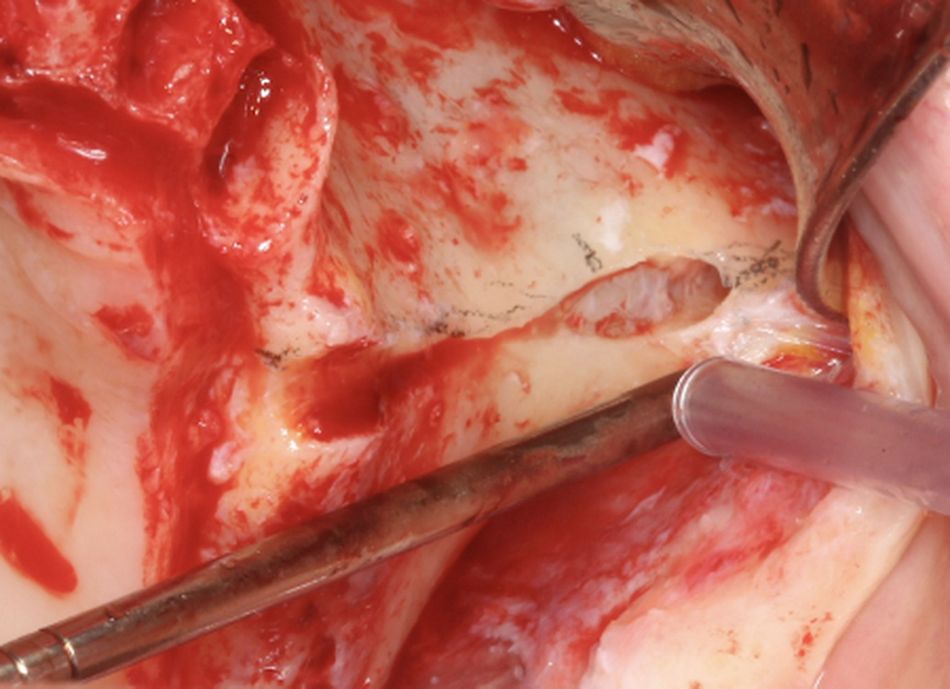
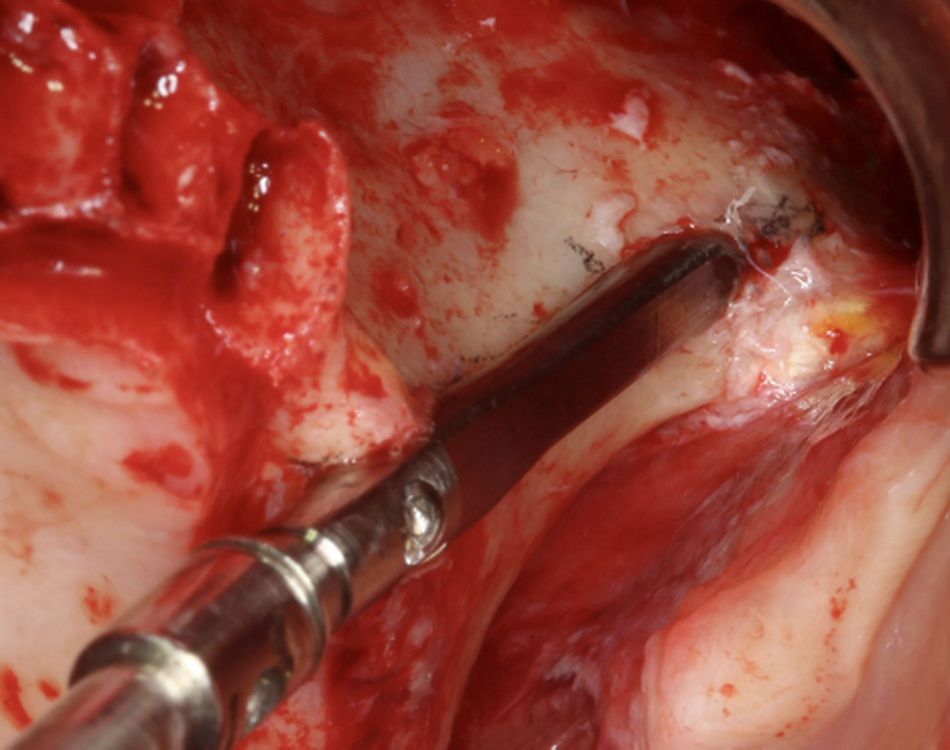
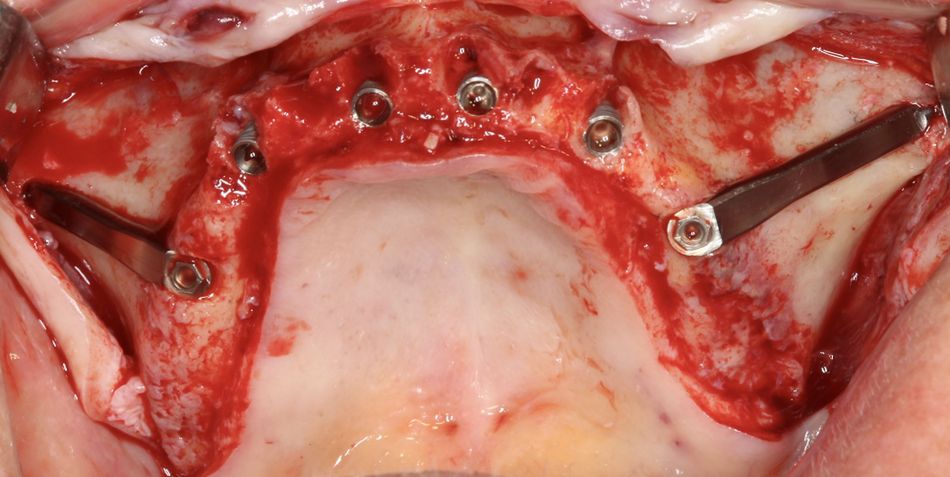
Following the drilling protocol, the ZAGA channel osteotomy prepared according to the virtual planning was appreciated with a minimal destruction of the alveolar bone maxillary wall and zygomatic bone. A precisely congruent to the implant shape maxillary groove was created while maintaining sinus lining integrity (Figs. 12 & 13).
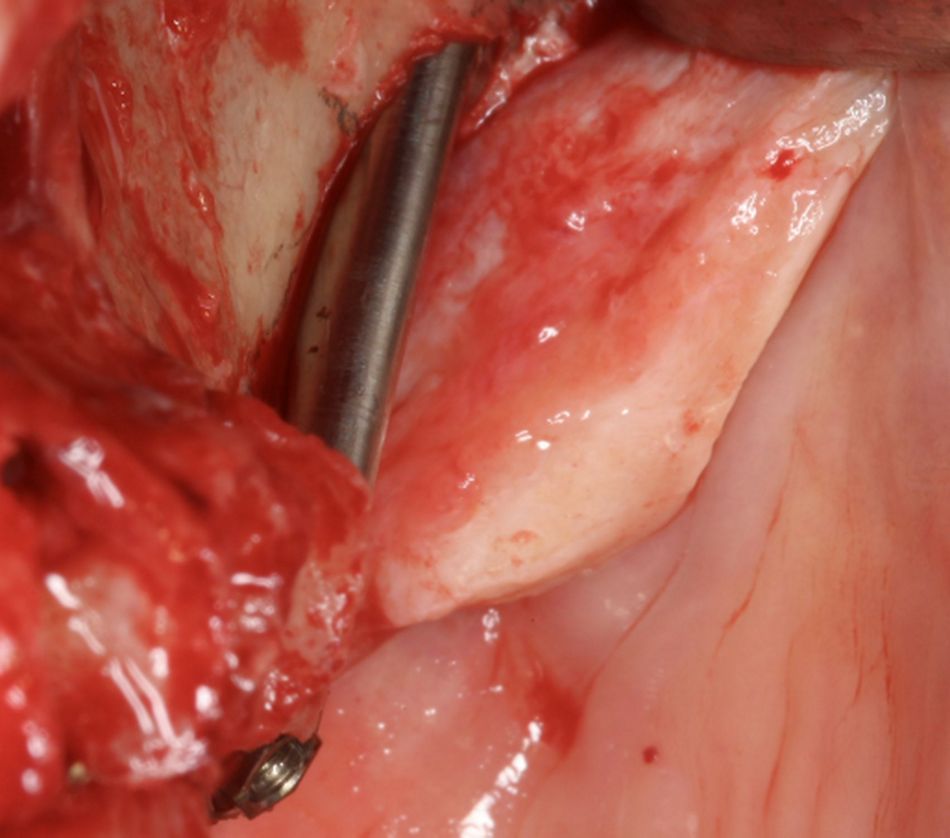
After it was ensured that the implant site was free of soft tissue remnants, the torque control was set at 50Ncm and 15 rpm, and a flat tapered implant design (Straumann Zygomatic Implant ZAGA®-Flat) was inserted at increased torque using the hand piece with the final aid of the manual implant holder. The self-tapping flutes helped this implant design to smoothly penetrate the external cortical of the zygomatic process. Enhanced primary stability was achieved by the implant tapered design and by a conservative final drill-implant diameter difference of 1 mm (Figs. 14 & 15).
Additional remarkable characteristics of this design include the diameter of the implant transport holder which is the same as the implant itself. This feature helps us to easily manage the implant insertion in situations where the implant is inserted close to another implant or into hard bone. As previously planned, the implant (grade 4 titanium) was placed partially outside the bone envelope. Thanks to its flat section, a possible vascular compression of the soft tissues was diminished (Figs. 16-19).
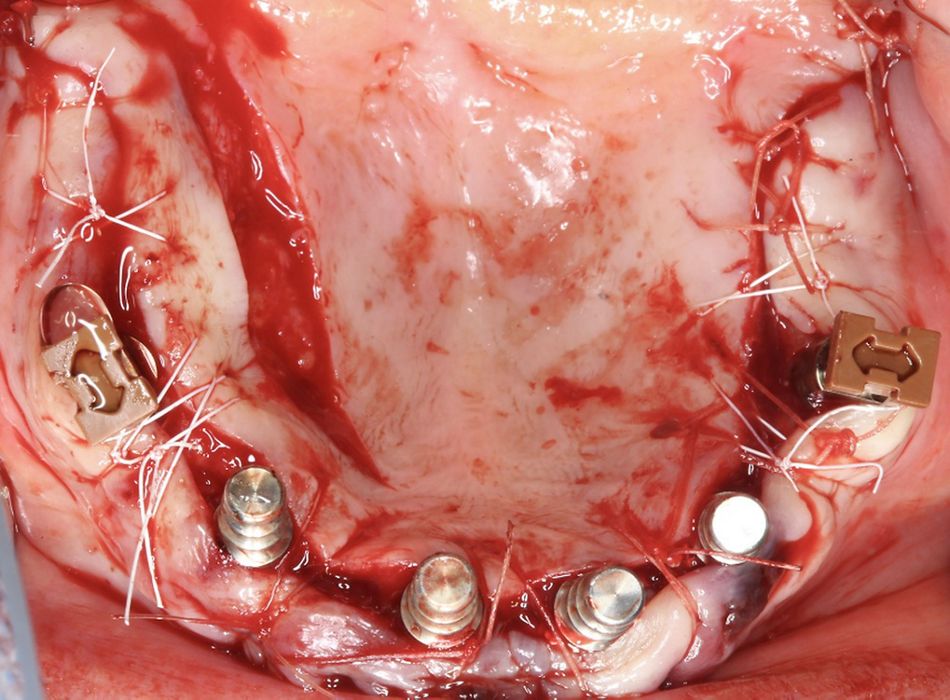
The same procedure was followed on the contralateral side. Additional four conventional implants were placed on the anterior side. To increase the amount of keratinized tissue buccal to the implant, a palatal incision was made. The double pediculate partial flap aimed to make possible a first intention closure of the soft tissue. Finally, a mattress technique with a non-resorbable suture was performed (Figs. 20 & 21).
In the lower jaw, four conventional implants on positions #32, #34, #42 and #44 were placed following the manufacture’s protocol.
- Fig. 5. Pencil Left Surgeon first act after raising the flap should be to mark the reference points for the alveolar and zygomatic bone entrances.
- Fig.6. Pencil Left 2 Clinical picture illustrating how the surgeon is marking the coronal and the zygomatic entrance points on the left second premolar/first molar position according to the virtual planning of Fig. 3.
- Fig.7. Channel left initial lateral cutting bur As the alveolar thickness is less than 4 mm a “tunnel” type osteotomy is not recommended. The lateral cutting bur helps to initiate a canal, were the next drill tail will slide. The canal diameter should still be reduced at this stage to precisely embrace and guide the next bur tail. Please note that just the first part of the drill is used in order to prepare a channel with a diameter congruent to the round bur tail. A slight adaptation of the step 7 allows for the use of a round bur (see steps 8 and 9) to precede the use of the lateral cutting bur. Considering that the hardness of the bone shall guide the decision, the presented sequence is adapted to this particular clinical case.
- Fig.8. Channel left, round bur The round bur tail being supported by the alveolar channel, this is the right time to evaluate the direction, the depth and the inclination of the future implant trajectory. Once the channel showed the desired depth, the floor surface shall become even, the round bur tail shall be able to gently slide up and down. The grinding with the round bur becomes more precise by gently touching the bone during the slide down movement.
- Fig.9. Channel left round bur2 With extreme precision the round bur has previously completed the channel grinding. The picture shows a notch marked at the zygomatic process of the maxillary bone. The round bur, sliding up and down, has penetrated on the zygomatic process of the maxillary bone. By a “grinding-back” movement the round bur would be able to eliminate channel floor irregularities. The goal being to prepare a smooth surface supporting the trajectory for the next drill.
- Fig.10. Channel left twist drill Once the notch is performed the channel would be double checked for uniform floor, desired inclination and depth. A twist drill of 2,9 mm diameter is advised as final drill diameter.
- Fig.11. Channel left twist drill.2 Using profuse irrigation, the twist drill slides up and down, using short pressure periods of about 4 seconds, allowing the saline to clean and cool the drill.
- Fig.12. Left osteotomy Detail of the left ZAGA channel osteotomy prepared accordingly to the virtual planning. Minimal destruction of the alveolar bone and maxillary wall has been performed. Note the enlarged but protective maxillary bone able to integrate with the implant. Note also the achieved sinus lining integrity. The antrostomy site was moved to an apical position on the zygomatic process of the maxillary bone.
- Fig.13. Measuring left osteotomy Implant length is estimated with a 2,9mm diameter gauge
- Fig.14. Left flat implant.1 A flat tapered implant design (Straumann Zygomatic Implant ZAGA®-Flat) is presented and its body compared to the osteotomy size. Note that the tapered apical part of the implant is provided with cutting flutes. The self-tapping flutes are helping the flat implant design (Straumann ZAGA®-Flat) to smoothly penetrate the external cortical of the zygomatic process with enhanced primary stability.
- Fig.15. Left flat implant.2 The clinical picture is pointing out (Straumann Zygomatic Implant ZAGA®-Flat) implant tip features (see implant picture). The benefit in adapting implant and implant-bed dimension and shape corresponds to a final drill -implant diameter difference of 1 mm. That unique tapered design feature on a zygomatic implant together with the use of a ZAGA conservative osteotomy, allows for an increased implant primary stability.
- Fig.16. Left flat implant.3 The clinical picture is showing an implant transport holder having the same diameter as the implant itself. That feature helps the surgeon to easily manage implant insertion in situations where the implant is inserted close to another implant or into hard bone.
- Fig.17. Left flat implant.4 The implant in place is partially outside the bone envelope. To diminish eventual vascular compression of the soft tissues, the implant (Straumann Zygomatic Implant ZAGA®-Flat) has a flat section. To reduce eventual bacterial contamination, the implant body is made of non-threaded turned grade 4 titanium.
- Fig.18. Left flat implant lateral.1 Clinical lateral view of the flat implant (Straumann ZAGA®-Flat) design. Note the difference with the classic round designs in both the amount and the type of surface facing the soft tissue.
- Fig.19. Left flat implant lateral.2 Straumann Zygomatic Implant ZAGA®-Flat implant in place from a lateral view. Note that its flat profile is not protruding out the remaining alveolar bone.
- Fig.20. Occlusal post-surgery Occlusal post-operative view. Two flat design, apically threaded and body turned titanium surface, have been placed. Implant head are in a prosthetically driven position sealing the ZAGA “canal type” osteotomy.
Prosthetic procedure
The prosthetic workflow included the positioning of screw retained abutments (SRAs) and positioning transfers in order to perform an analog impression (Fig. 21).
The delivery of the screw-retained temporary bridge was done in the same day and an X-ray control was taken.
- Fig.21. Occlusal sutured To maximize the amount of keratinized tissue buccal to the implant, a palatal incision was made. To make possible a first intention closure of the soft tissue, double pediculated partial flap was performed. Non resorbable mattress suture was used.
Treatment outcomes
The clinical and radiographic one-year follow-up evaluations showed the outstanding outcomes of combining the use the ZAGA Concept for hard and soft tissue management and an implant design (Straumann Zygomatic implant ZAGA flat) with features adapted to the patient anatomy. Additionally, we could also appreciate the excellent bone and soft tissues stability around Straumann zygomatic abutments that have been achieved. This was also thanks to the anatomic, prosthetically driven position of the implants and the use of straight non-angulated abutments (Figs. 22-25).
At one-year follow-up, the high level of patient satisfaction was maintained as she considered that all her expectations were fulfilled (Fig. 26).
- Fig.22. One year-soft tissue, occlusal The one-year control shows the results of combining the use the ZAGA Concept for hard and soft tissue management and an implant design (Straumann Zygomatic implant ZAGA flat) with features adapted to the patient anatomy. Excellent bone and soft tissues stability around Straumann zygomatic abutments have been achieved.
- Fig.23. One year-prostheses, occlusal One-year occlusal view of the prostheses placed by Drs. Peter and Madalina Simon, ZAGA Center Stuttgart, Germany. Note the anatomic, prosthetically driven, position of the implants achieved with straight, non-angulated, abutments.
- Fig.24. UL post.23/6/2020 (1yr) CBCT oblique 2D cut and correspondent plane on 3D vision showing implant position and sinus status of the left implant at the one-year control. Totally transparency of the maxillary sinus is maintained.
- Fig.25. UR post.23/6/2020 (1yr) CBCT oblique 2D cut and correspondent plane on 3D vision showing implant position and sinus status of the right implant at the one-year control. Totally transparency of the maxillary sinus is maintained.
- Fig.26. Smiling. 23/6/2020 (1yr) Patient satisfaction is showed at one-year control
Acknowledgements
The author particularly appreciated and acknowledge the contribution of Drs. Peter and Madalina Simon, ZAGA Center Stuttgart, Germany for the discussions during the prosthetic-driven implant planning phase and for taking care of the prosthesis manufacturing and placement.

Straumann® Zygomatic Implant System
An anatomically based fixed solution for patients with atrophic maxillae, designed by experts with the patient in mind.

_aparicio.jpg?wid=950)
_aparicio.jpg?wid=950)
_aparicio.jpg?wid=950)
_aparicio.jpg?wid=950)


.2_aparicio.jpg?wid=950)
.2_aparicio.jpg?wid=950)
