Authors: Dr. Sergio H. Cacciacane (DDS), Dr. Maximiliano Cacciacane (DDS, MSc), Dr. Cristian Orlando (DDS, MSc), Dr. Frank Ernesto Perez Avila (DDS, MSc), Dr. Eng. Seyed Behnam Taghavi (PhD, MSc, BSc, DT). All: ESIRO Barcelona (Escuela Superior de Implantología y Rehabilitación Oral) (www.esiro.es)
Introduction
Immediate implants in fresh extraction sites were demonstrated to be predictable and successful. However, adherence to clinical protocols and the strict application of case selection criteria remain essential to ensure treatment success4.
With the new BLX implant, Straumann® has recently introduced an optimized implant design, addressing immediate stability - a key requirement for immediate placement in extraction sockets and temporization.5,6 The implant is characterized by a protruding thread geometry, maximizing apical bone engagement and primary implant stability irrespective of bone quality7.
Digitally guided techniques have significant potential in rendering surgical workflows more accurate, predictable and less invasive8. The increasing digitalization and the introduction of novel techniques and materials, like, e.g. digital smile design, have recently also started to transform prosthetic workflows substantially9,10. However, associated steps within the workflow remain platform, data format and site-dependent and may involve significant and laborious adaptation, validation and transfer steps to provide the desired outcomes.
With Smilecloud, a cloud- and AI-based platform has recently become available that significantly improves and facilitates the prosthetic workflows from planning to realization by removing interfaces between individual workflow steps, facilitating team cooperation across sites and optimizing patient communication. Specifically, the AI-assisted prosthetic design algorithm based on biometric libraries allows clinicians and technicians to seamlessly transition digital smile design concepts into prosthetic provisional and final wax-ups in one platform and with a few simple steps.
The presented case illustrates these exciting features of this novel tool for a patient undergoing immediate implantation and restoration in the aesthetic area using Straumann®BLX.
Initial situation
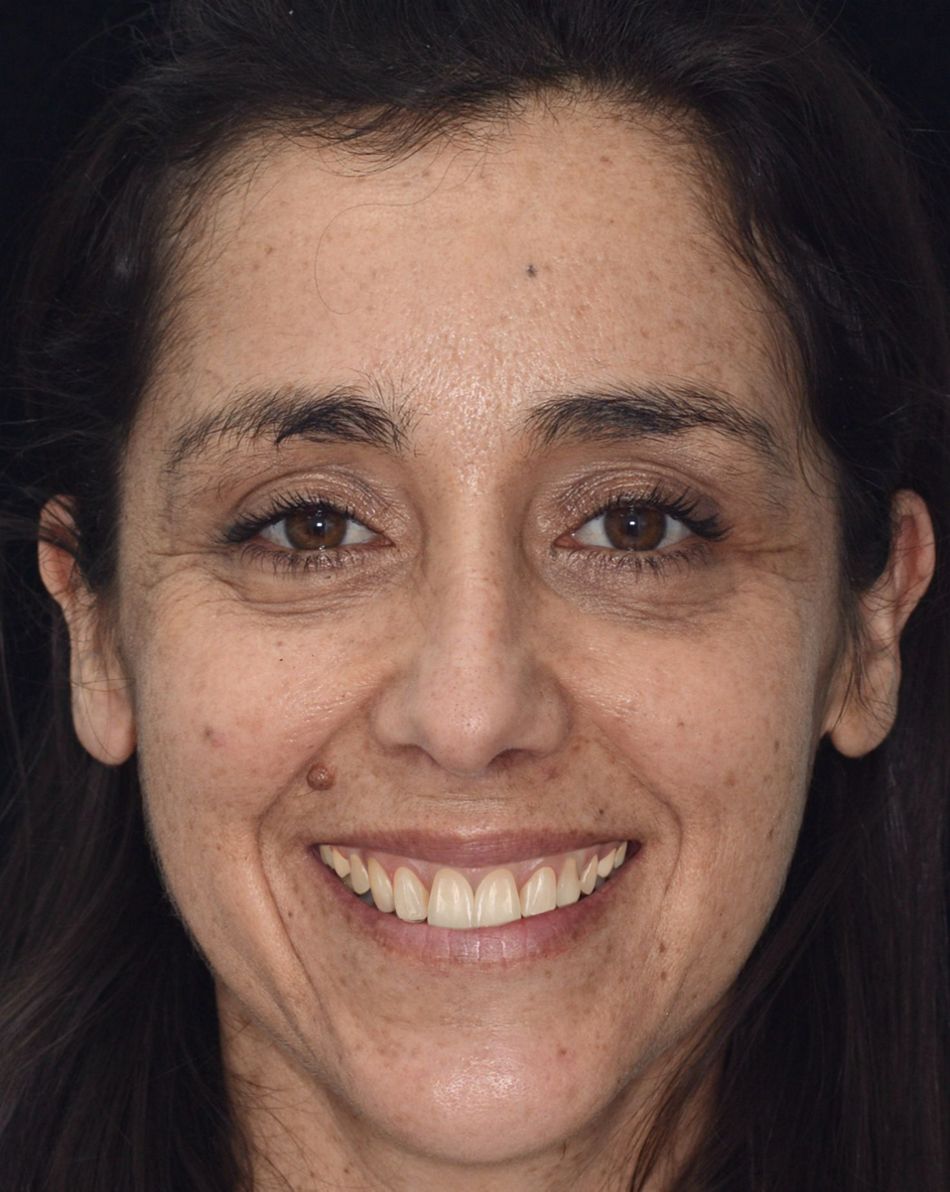
A 42-year-old female patient presented in our office with a chief complaint about a horizontal root fracture and complete crown loss of her upper left first premolar (tooth #14), compromising her aesthetics and masticatory function (Fig. 1). The patient reported to be a non-smoker, in good overall general health and displayed a history of periodontitis. Her periodontal status was assessed as stable after reinforcing hygiene routines and being included in a routine professional prophylaxis program. Oral examination revealed only a mild presence of plaque at free gingival margins and adjacent areas corresponding to a plaque index of 1, according to Silness and Löe11.
The remaining tooth root of tooth #14 was considered hopeless and unrestorable. It did not allow for a reliable and predictable long-term treatment prognosis after assessment of all, i.e., the prosthodontic, periodontal and endodontic dimensions12,13. After consideration of all potential local, site-specific and more general patient-related factors, a recommendation for implant therapy was given and was consented to by the patient.
- Fig 1: Pre-treatment frontal photographs. LEFT: patient's facial and smile esthetics, RIGHT: Close-up of the patient's smile illustrating a high smile line and extended buccal corridors prominently exposing her lost right first premolar.
- Fig 1: Pre-treatment frontal photographs. LEFT: patient's facial and smile esthetics, RIGHT: Close-up of the patient's smile illustrating a high smile line and extended buccal corridors prominently exposing her lost right first premolar.
Treatment planning
The treatment plan was based on replacing tooth #14 with an immediate, i.e. immediately placed and provisionalized implant restoration using a fully digital workflow comprising Straumann® BLX implants. Novel artificial intelligence (AI) assisted design algorithms using Smilecloud were used for restorative planning and waxing. Prosthetically driven planning of the implant restoration was based on combined prosthetic anatomic virtual patient models. The surgical and prosthetic workflows were designed as a guided surgical approach combined with immediate restoration to ensure maximum placement precision and reliability as well as optimal hard tissue healing and soft tissue adaptation, respectively3,14,15. A three-dimensional assessment of the patient's alveolar anatomy revealed adequate buccal wall thickness and confirmed ideal anatomic conditions for immediate implant placement16.
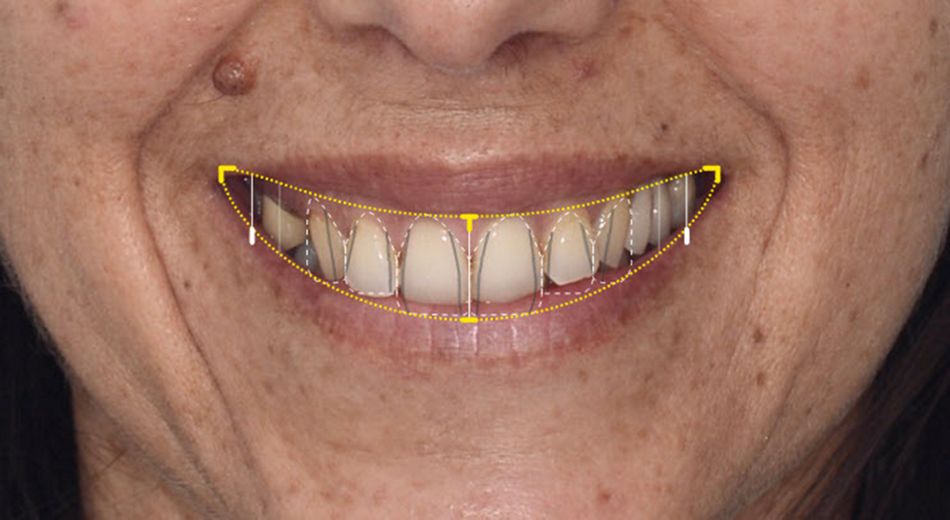
Digital smile design and digital waxing of the provisional wax-ups were obtained using the Smilecloud web-based platform. Figure 2 illustrates the real-time design of a provisional wax-up starting from frontal digital photographs and intraoral scans using Smilecloud's AI algorithms. The full process was intuitive and straightforward and comprised the following steps: First, the AI was instructed on the smile curve and available restorative space (yellow line), midline, and the patient's dento-gingival phenotype comprising tooth shape, proportions, contact points, gingival margins, papilla levels and embrasures (white dotted lines). Based on this input, the AI proposed an appropriate model from the system's biometric library, which was validated using real-time displayed overlays. Finally, the AI's algorithms directly converted the corresponding model into the provisional wax up. Morphed overlays of the patient's image and wax-up were used for patient communication and to illustrate and validate the planned final treatment outcomes.
- Fig 2: Digital smile design within Smilecloud. Left: Close-up image of the patient's smile in Smilecloud used to define the smile line and restorative space (yellow lines) and dento-gingival phenotype (white dotted lines). LEFT: Real-time rendering illustrating the patient's future facial and smile aesthetics after selecting the adequate model from Smilecloud's biometric library.
- Fig 2: Digital smile design within Smilecloud. Left: Close-up image of the patient's smile in Smilecloud used to define the smile line and restorative space (yellow lines) and dento-gingival phenotype (white dotted lines). LEFT: Real-time rendering illustrating the patient's future facial and smile aesthetics after selecting the adequate model from Smilecloud's biometric library.
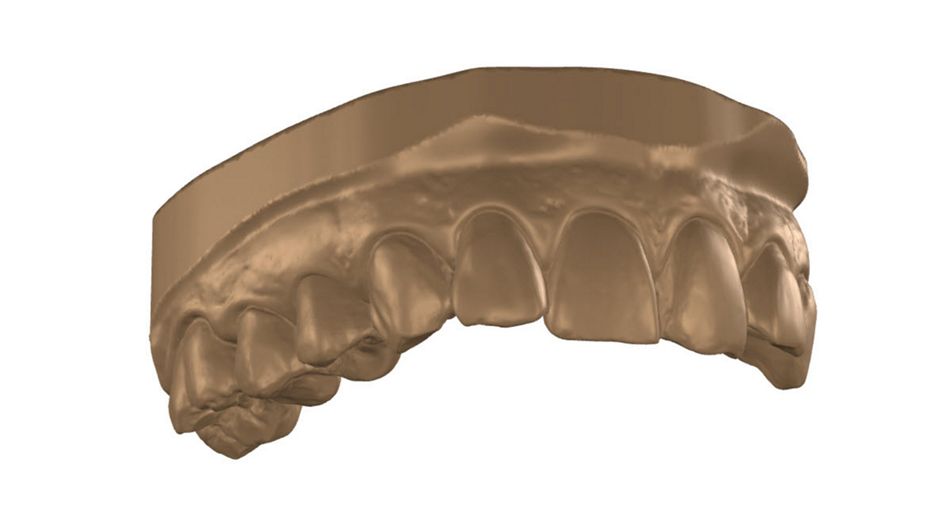
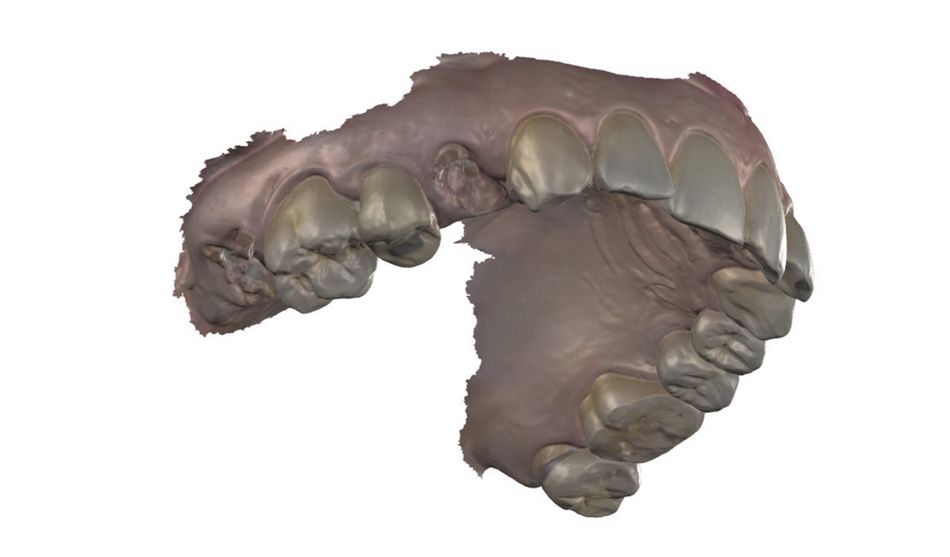
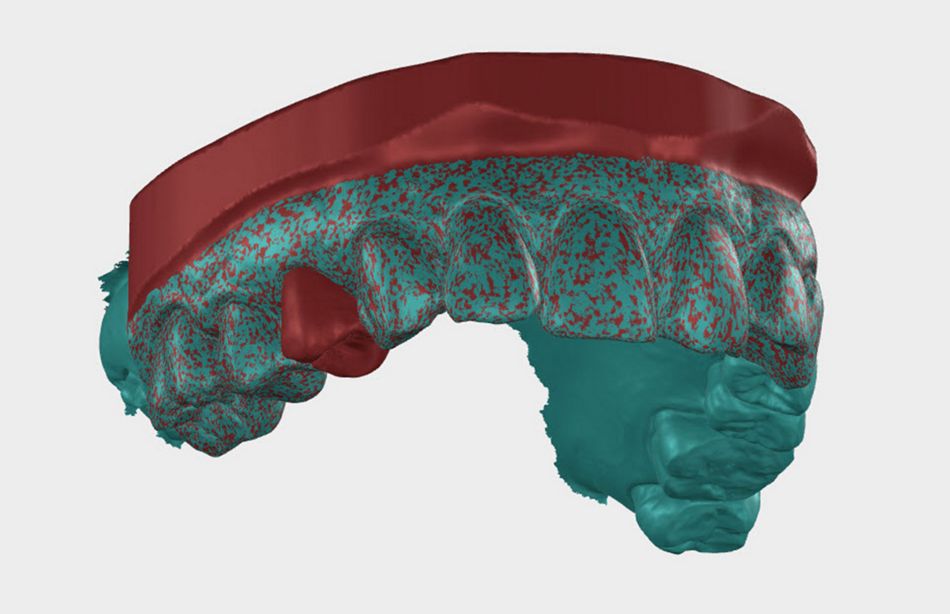
Overlays of the delivered wax-up with intraoral scans indicated a perfect match between both STL data files. Figure 3 illustrates the alignment of the provisional wax-up from Smilecloud's biometric library (left) with the patient's intraoral scan (middle). Overlays indicated high consistency between proposed and existing dental and gingival structures. The design of the planned restorative crown and occlusal surfaces were considered ideal.
- Fig 3: Illustration of the design and validation of digital wax-ups provided by Smilecloud using intraoral scan data. LEFT: Digital wax-up proposed by Smilecloud's AI algorithms and based on Smilecloud's biometric library models. MIDDLE: Intraoral scan of the patient. RIGHT: Superimposed STL files of intraoral scan (green) and Smilecloud-generated digital wax-up (red) confirming an ideal match between models and adequate design of the restorative crown.
- Fig 3: Illustration of the design and validation of digital wax-ups provided by Smilecloud using intraoral scan data. LEFT: Digital wax-up proposed by Smilecloud's AI algorithms and based on Smilecloud's biometric library models. MIDDLE: Intraoral scan of the patient. RIGHT: Superimposed STL files of intraoral scan (green) and Smilecloud-generated digital wax-up (red) confirming an ideal match between models and adequate design of the restorative crown.
- Fig 3: Illustration of the design and validation of digital wax-ups provided by Smilecloud using intraoral scan data. LEFT: Digital wax-up proposed by Smilecloud's AI algorithms and based on Smilecloud's biometric library models. MIDDLE: Intraoral scan of the patient. RIGHT: Superimposed STL files of intraoral scan (green) and Smilecloud-generated digital wax-up (red) confirming an ideal match between models and adequate design of the restorative crown.
STL files of the digital wax-up were next combined with Digital Imaging and Communication in Medicine (DICOM) data from CBCT in coDiagnostix® to result in a virtual anatomic model. This model was used to plan the ideal position of the implant and, importantly, the bucco-palatal orientation and angulation of the implant (Fig. 4).
- Fig. 4: Illustration of the prosthetically driven implant restorative planning based on virtual anatomic models from aligned digital wax-up STL files provided by Smilecloud and 3D alveolar anatomic CBCT DICOM data within coDiagnostix®. Mesiodistal sections illustrate the detailed planning of the bucco-palatal implant position and angulation in relation to the planned restoration.
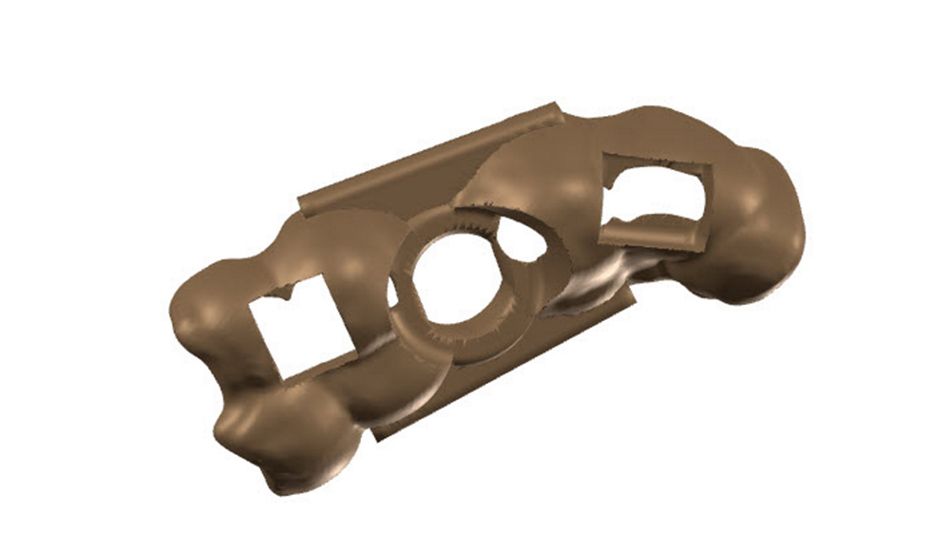
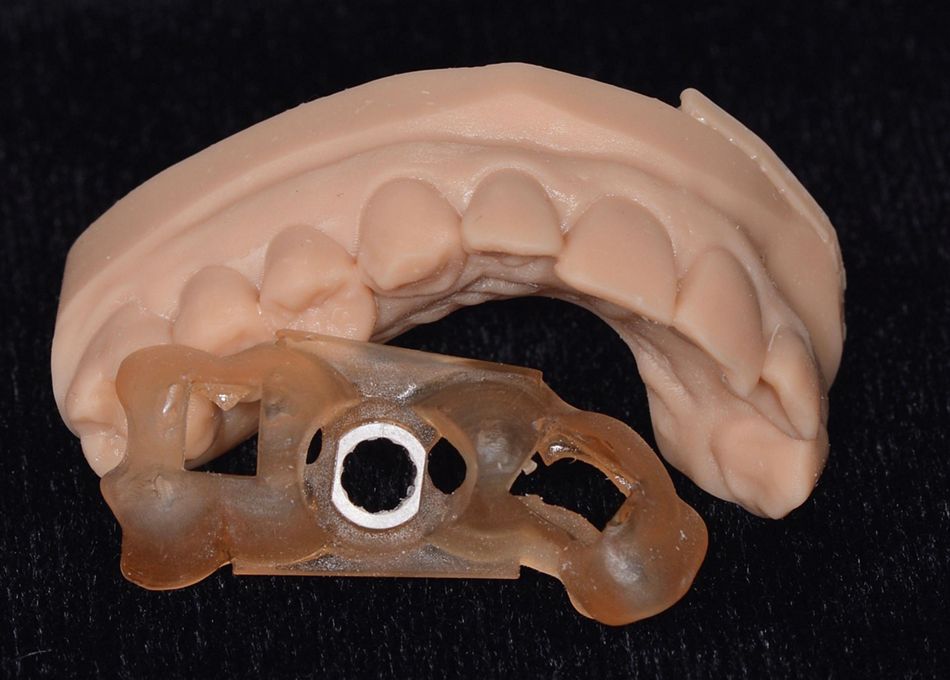
A tooth-born surgical guide was designed within coDiagnostix® and in-house 3D-printed (Cares® P30+) to transfer the virtual plan into the surgical field. The virtual model, the resulting fabricated guide and a printed mock-up model are illustrated in Figure 5. Verification windows were included in the design of the guide to ensure an adequate fit during the procedure.
- Fig. 5: Surgical template. LEFT: 3D model of the tooth-born surgical guide comprising mesial and distal windows for verifying adequate fit. RIGHT: 3D printed surgical guide and mock-up model (RIGHT).
- Fig. 5: Surgical template. LEFT: 3D model of the tooth-born surgical guide comprising mesial and distal windows for verifying adequate fit. RIGHT: 3D printed surgical guide and mock-up model (RIGHT).
Surgical procedure
Surgical procedures were performed under standard infiltration anaesthesia and started by atraumatically extracting the tooth root after sectioning the root in a mesiodistal direction, luxation of the segments using a periosteal elevator, and removal of the root segments using forceps. Visual assessment revealed that the buccal bone wall was entirely preserved after extraction and displayed no to minimal vertical bone loss. The socket morphology was classified as Elian Type I and, consequently, ideal for immediate placement and temporization16,17.
- Fig. 6: Illustration of atraumatic tooth extraction and resulting extraction alveolar anatomy. LEFT: atraumatic tooth extraction after mesiodistal root sectioning. RIGHT: occlusal view on the resulting extraction alveole.
- Fig. 6: Illustration of atraumatic tooth extraction and resulting extraction alveolar anatomy. LEFT: atraumatic tooth extraction after mesiodistal root sectioning. RIGHT: occlusal view on the resulting extraction alveole.
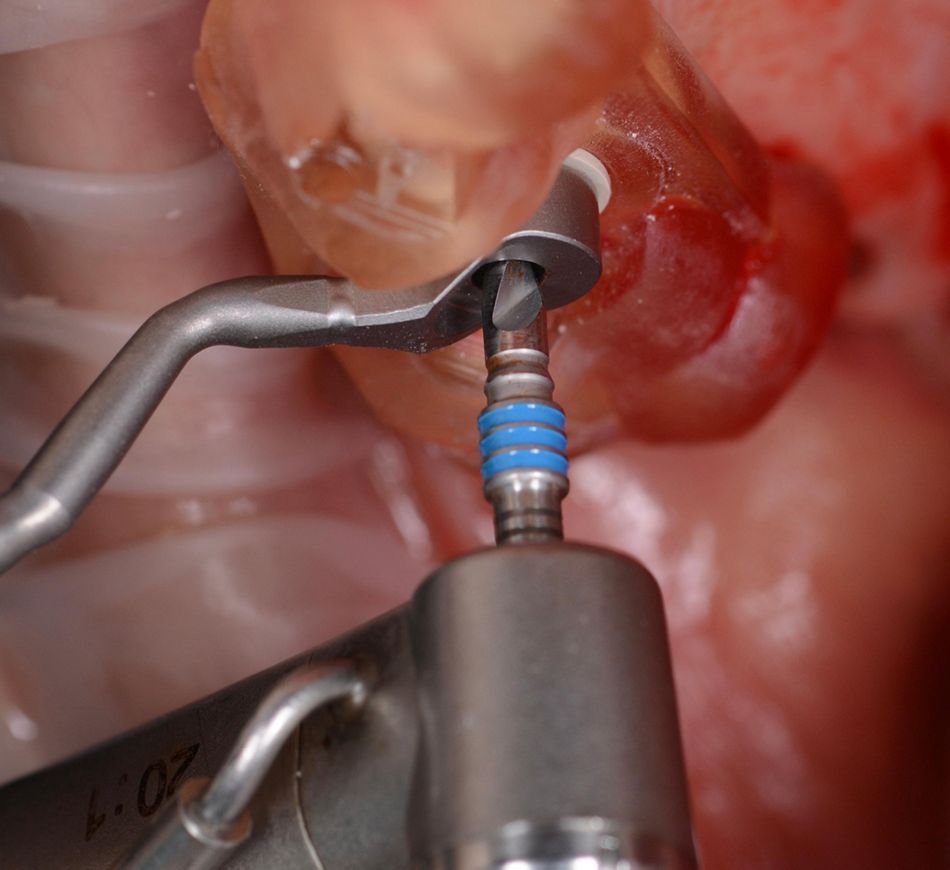
The implant osteotomy was prepared following the manufacturer's instructions by guided drilling using a ∅2.2 mm pilot and ∅2.8 mm final drill (Figure 7). Next, a 3.75 mm x 12 mm BLX (SLActive®, Roxolid®) implant was placed guided using a motor handpiece. The surgical template served as a reference to define placement depth. The immediate primary stability, assessed by an insertion torque of >50 Nm and an ISQ value of 75, was high and adequate for immediate provisionalization.
- Fig. 7: Guided surgery: LEFT: Situation after placement of the surgical guide. MIDDLE: ∅2.2 mm guided pilot drilling. RIGHT: ∅2.8 mm final drill. The axial orientation of the drills was controlled by corresponding drill handles.
- Fig. 7: Guided surgery: LEFT: Situation after placement of the surgical guide. MIDDLE: ∅2.2 mm guided pilot drilling. RIGHT: ∅2.8 mm final drill. The axial orientation of the drills was controlled by corresponding drill handles.
- Fig. 7: Guided surgery: LEFT: Situation after placement of the surgical guide. MIDDLE: ∅2.2 mm guided pilot drilling. RIGHT: ∅2.8 mm final drill. The axial orientation of the drills was controlled by corresponding drill handles.
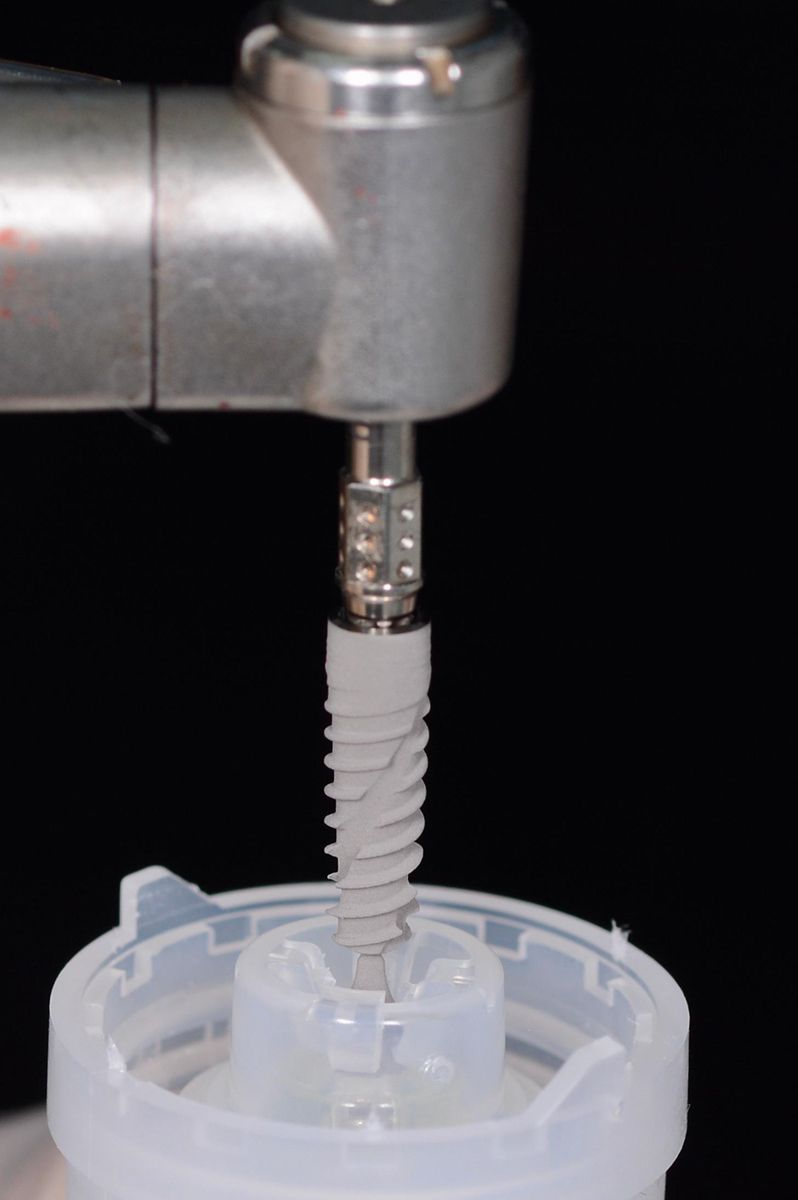
- Fig. 8: Placement of a Ø3.5 x 12 mm BLX (SLActive®, Roxolid®) implant. LEFT: Pick up of the BLX implant from the vial lid. RIGHT: Implant placement using a motor-driven handpiece and the surgical template.
- Fig. 8: Placement of a Ø3.5 x 12 mm BLX (SLActive®, Roxolid®) implant. LEFT: Pick up of the BLX implant from the vial lid. RIGHT: Implant placement using a motor-driven handpiece and the surgical template.
Implant placement resulted in a gap between the implant and buccal bone of ca. 1.5 mm (Fig. 9). To limit buccal contour changes and potentially enhance the thickness of the peri-implant soft tissues coronal to the implant-abutment interface, the gap was filled with a particulate Xenograft (Straumann® Xenograft) that was combined with autologous bone. The latter was obtained by adopting a slow-speed drilling protocol without irrigation, as described by Anitua et al.18,19. Straumann® Xenograft was chosen based on its ability to alter buccal bone healing and potentially improve peri-implant bone volume stability20.
Prosthetic procedure
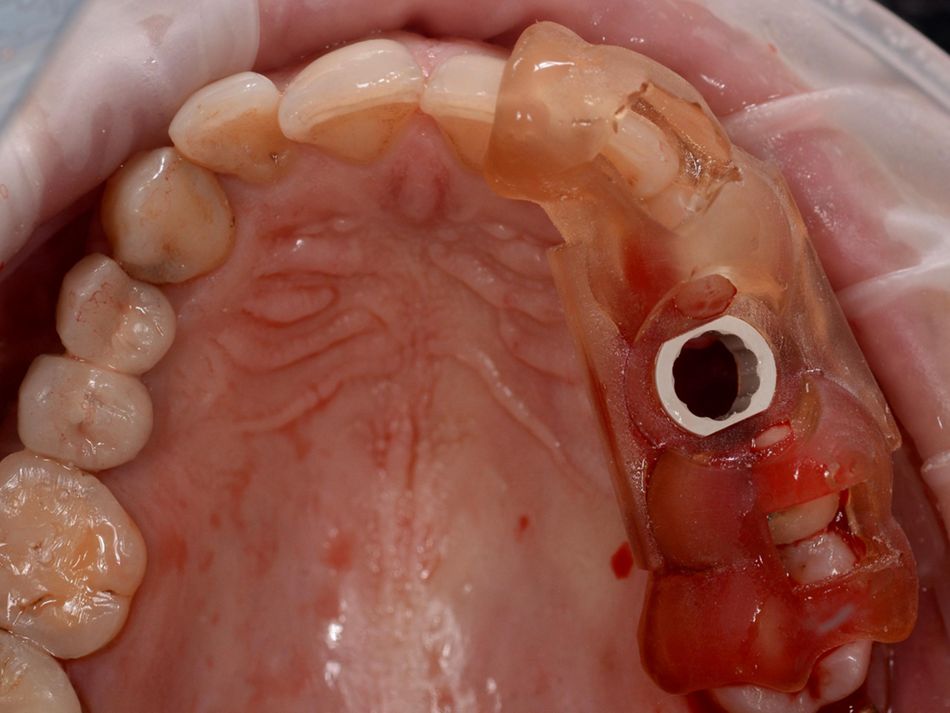
The implant was immediately restored to condition the peri-implant soft tissues to the new restoration and prevent soft tissue collapse until delivery of a CAD/CAM monomer-free PMMA provisional. The latter was prepared from final wax-ups combined from STL files of post-surgical intraoral scans using a CARES scan abutment and the Smilecloud-derived digital wax-up. Final wax-ups were prepared in Straumann® Cares® Visual (Fig. 9).
- Fig. 9: Situation after implant placement and intraoral scan. LEFT: Occlusal view after implant placement illustrating the buccopalatal implant position and extension of the implant gab between the buccal bone and the implant. RIGHT: Intraoral scan with a CARES scan body.
- Fig. 9: Situation after implant placement and intraoral scan. LEFT: Occlusal view after implant placement illustrating the buccopalatal implant position and extension of the implant gab between the buccal bone and the implant. RIGHT: Intraoral scan with a CARES scan body.
Figure 10 illustrates the delivery of the chairside prepared acrylic immediate provisional based on the final wax-up and a screw-retained temporary abutment. The emergence profile's critical and subcritical contours were adapted extraorally to support crestal soft tissue healing optimally.21 Occlusal aspects were modified to reduce initial loading.
- Fig. 10: Delivery of chair-side prepared immediate provisional based on the Smilecloud-derived wax-up and the post-surgical intraoral scans and using a temporary screw-retained abutment.
Treatment outcomes and Conclusions
Figure 11 shows the resulting occlusal situation after immediate provisionalization and the lateral aesthetic appearance. Smilecloud's AI-enhanced digital workflow and biometric library models allowed for an efficient and straightforward design of a provisional wax-up feeding into subsequent surgical planning and prosthetic manufacturing steps. The patient expressed her complete satisfaction with the procedure, both in terms of aesthetics and functionality but also from a pre-treatment outcome visualization point of view.
- Fig. 11: Situation after delivery of the immediate provisional. LEFT: occlusal view during the check of occlusion for contact points. RIGHT: lateral view illustrating the optimal design and soft tissue adaptation to the crown.
- Fig. 11: Situation after delivery of the immediate provisional. LEFT: occlusal view during the check of occlusion for contact points. RIGHT: lateral view illustrating the optimal design and soft tissue adaptation to the crown.
Author's testimonial
Smilecloud was a valuable asset in the whole journey, as we used it to communicate with the patient about the potential outcome and benefits of an immediate restoration after an immediate implant, engage with the patient using Smilecloud and show in real-time how we could update her smile and also the designed provisional, all in the same platform was game-changer for the patient (and also the clinical team).
References:
- Koh RU, Rudek I, Wang H-L. Immediate Implant Placement: Positives and Negatives. Implant Dent. 2010;19(2):98–108
- Buser D, Chappuis V, Belser UC, Chen S. Implant placement post extraction in esthetic single tooth sites: when immediate, when early, when late? Periodontol 2000. 2017;73(1):84–102.
- Covani U, Cornelini R, Calvo-Guirado JL, Tonelli P, Barone A. Bone remodeling around implants placed in fresh extraction sockets. Int J Periodontics Restorative Dent. 2010;30(6):601–607.
- Botticelli D, Renzi A, Lindhe J, Berglundh T. Implants in fresh extraction sockets: a prospective 5-year follow-up clinical study. Clin Oral Implants Res. 2008;19(12):1226–1232.
- Javed F, Ahmed HB, Crespi R, Romanos GE. Role of primary stability for successful osseointegration of dental implants: Factors of influence and evaluation. Interventional Medicine and Applied Science. 2013;5(4):162–167.
- Ophir Fromovich, Karim Dada, Leon Pariente, Marwan Daas. BLX: a new generation of self-drilling implants. Quintessence Special issue. 2019;:7–39.
- Ibrahim A, Heitzer M, Bock A et al. Relationship between Implant Geometry and Primary Stability in Different Bony Defects and Variant Bone Densities: An In Vitro Study. Materials. 2020;13(19):4349.
- Colombo M, Mangano C, Mijiritsky E, Krebs M, Hauschild U, Fortin T. Clinical applications and effectiveness of guided implant surgery: a critical review based on randomized controlled trials. BMC Oral Health. 2017;17(1):150.
- de Oliveira NRC, Pigozzo MN, Sesma N, Laganá DC. Clinical efficiency and patient preference of digital and conventional workflow for single implant crowns using immediate and regular digital impression: A meta‐analysis. Clin Oral Impl Res. 2020;31(8):669–686.
- Wulfman C, Naveau A, Rignon-Bret C. Digital scanning for complete-arch implant-supported restorations: A systematic review. J Prosthet Dent. 2020;124(2):161–167.
- Silness J, Löe H. Periodontal Disease in Pregnancy II. Correlation Between Oral Hygiene and Periodontal Condition. Acta Odontologica Scandinavica. 1964;22(1):121–135.
- Zitzmann NU, Krastl G, Hecker H, Walter C, Weiger R. Endodontics or implants? A review of decisive criteria and guidelines for single tooth restorations and full arch reconstructions. International Endodontic Journal. 2009;42(9):757–774.
- Zitzmann N, Margolin M, Filippi A, Weiger R, Krastl G. Patient assessment and diagnosis in implant treatment. Aust Dental J. 2008;53(s1):S3–S10.
- den Hartog L, Huddleston Slater JJR, Vissink A, Meijer HJA, Raghoebar GM. Treatment outcome of immediate, early and conventional single-tooth implants in the aesthetic zone: a systematic review to survival, bone level, soft-tissue, aesthetics and patient satisfaction. J Clin Periodontol. 2008;35(12):1073–1086.
- Chen ST, Buser D. Clinical and esthetic outcomes of implants placed in postextraction sites. Int J Oral Maxillofac Implants. 2009;24 Suppl:186–217.
- Kan JYK, Roe P, Rungcharassaeng K et al. Classification of sagittal root position in relation to the anterior maxillary osseous housing for immediate implant placement: a cone beam computed tomography study. Int J Oral Maxillofac Implants. 2011;26(4):873–876.
- Elian N, Cho S-C, Froum S, Smith RB, Tarnow DP. A simplified socket classification and repair technique. Pract Proced Aesthet Dent. 2007;19(2):99–104; quiz 106.
- Anitua E, Carda C, Andia I. A Novel Drilling Procedure and Subsequent Bone Autograft Preparation: A Technical Note. Int J Oral Maxillofac Implants. 2007;22(1):138–145.
- Paolantonio M, Dolci M, Scarano A et al. Immediate Implantation in Fresh Extraction Sockets. A Controlled Clinical and Histological Study in Man. Journal of Periodontology. 2001;72(11):1560–1571.
- Araújo MG, Linder E, Lindhe J. Bio-Oss® Collagen in the buccal gap at immediate implants: a 6-month study in the dog: Xenogenic graft and immediate implants. Clinical Oral Implants Research. 2011;22(1):1–8.
- González-Martín O, Lee E, Weisgold A, Veltri M, Su H. Contour Management of Implant Restorations for Optimal Emergence Profiles: Guidelines for Immediate and Delayed Provisional Restorations. Int J Periodontics Restorative Dent. 2019;40(1):61–70.