Initial situation
Description of the patient:
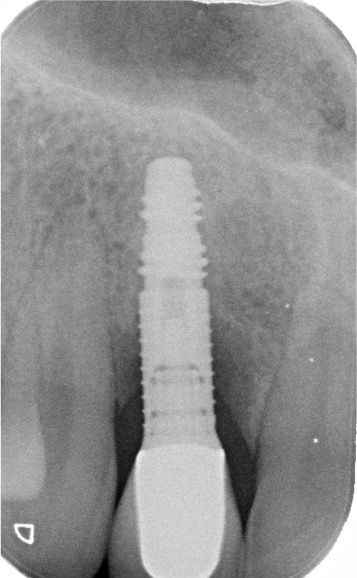
Male, 38 years, implant (Frialit) in region 12 (FDA) seated approximately 20 years ago. The tooth was lost after a trauma. The patient is now referred for treatment of peri-implantitis. The patient's esthetic concern is relatively high, but he has a low smile line. Fully healthy and a non-smoker. No signs of periodontal disease, generally good plaque control but sporadic signs of marginal and papillary gingivitis in the posterior segments. Radiographic and clinical examination demonstrates advanced peri-implant bone loss at implant in region 12 (FDA), with pronounced signs of inflammation. Diagnosis: Localized advanced peri-implantitis.
Treatment planning
Brief description of the treatment plan:
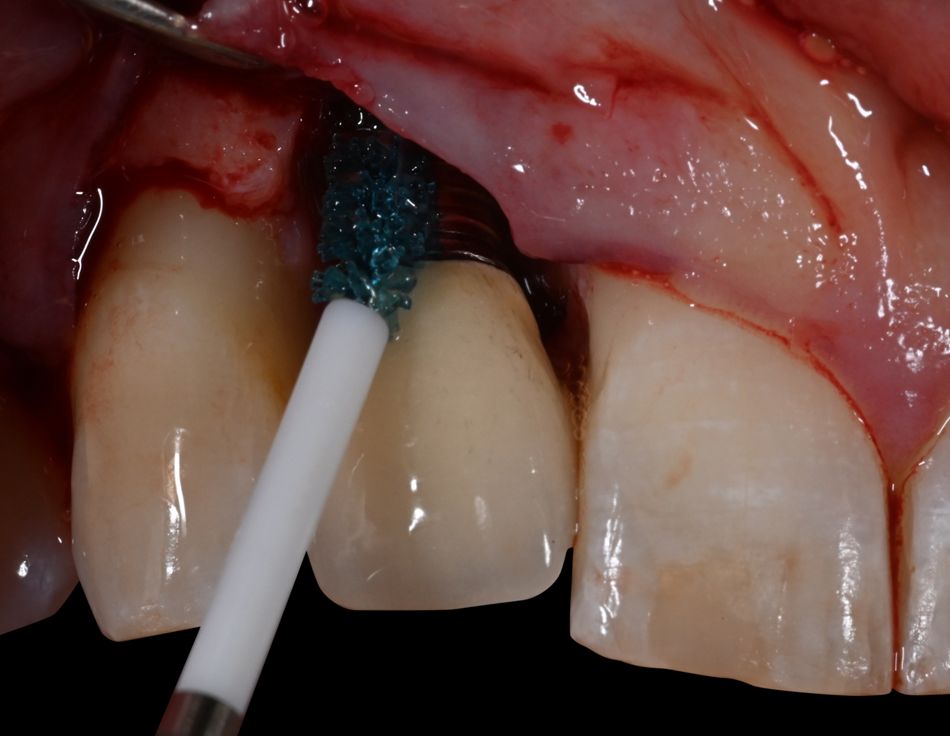
After careful oral hygiene instruction and localized non-surgical treatment with Labrida BioClean™ the patient was scheduled for surgery. Baseline pocket probing depths were 8-9 mm with positive BoP scores. The rationale for the surgical strategy used on this implant with peri-implantitis was to reconstruct the peri-implant osseous defect with bone using a slowly resorbable xenogenic graft, while EMD was to be used to accomplish optimal soft tissue healing in the esthetic zone. The combination of mechanical and chemical decontamination of the implant surface with Labrida BioClean™ and Straumann PrefGel® was to be used to prepare the implant surface for the graft material.
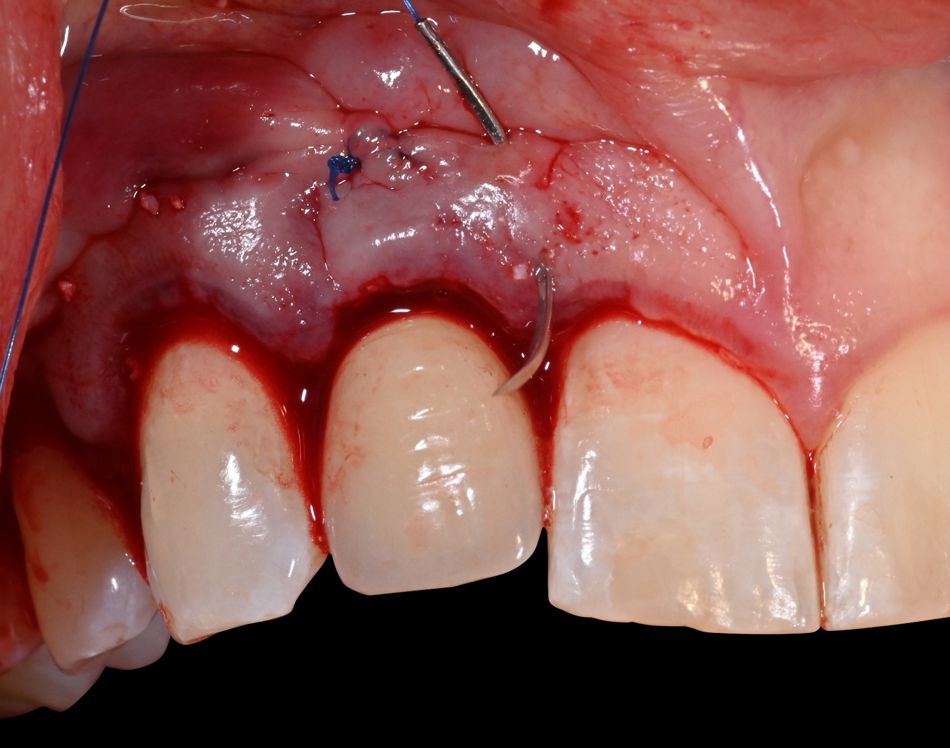
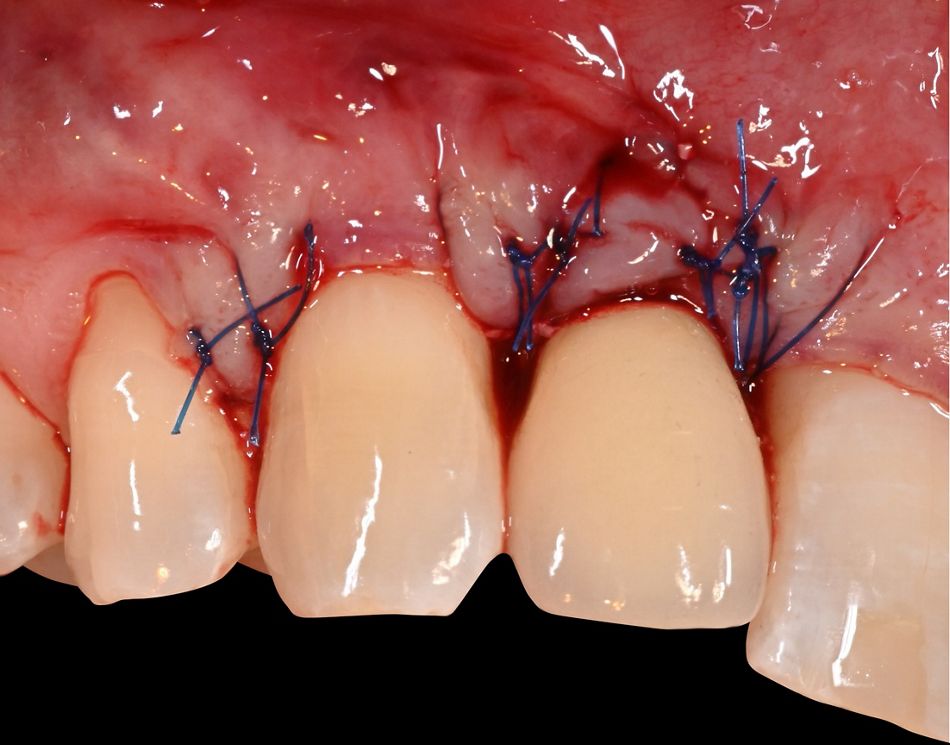
Surgical procedure
Description of surgical procedure:
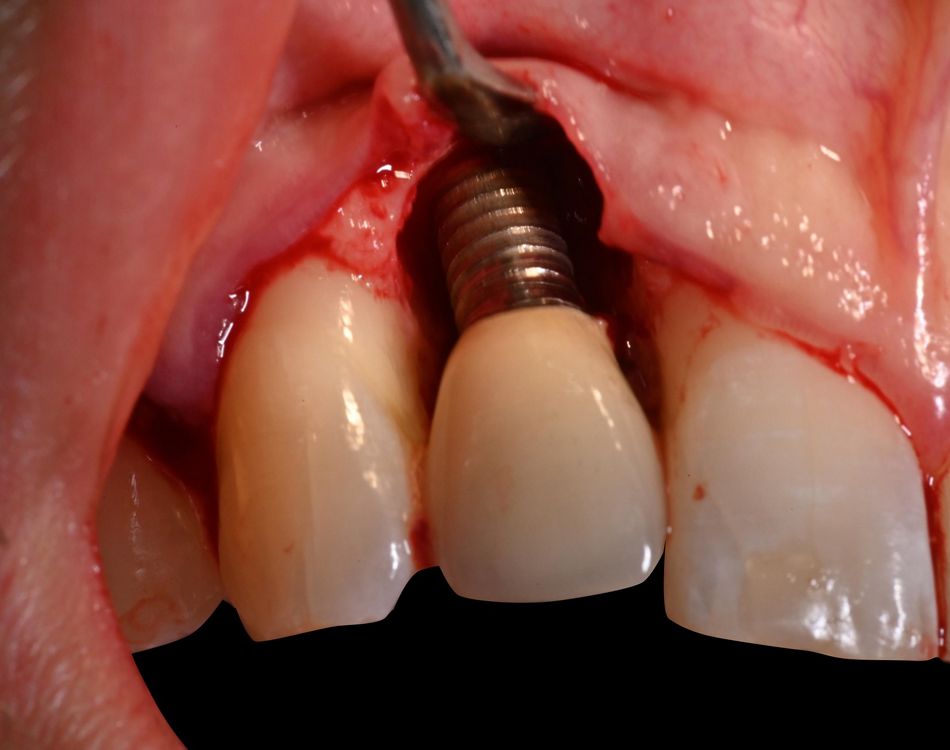
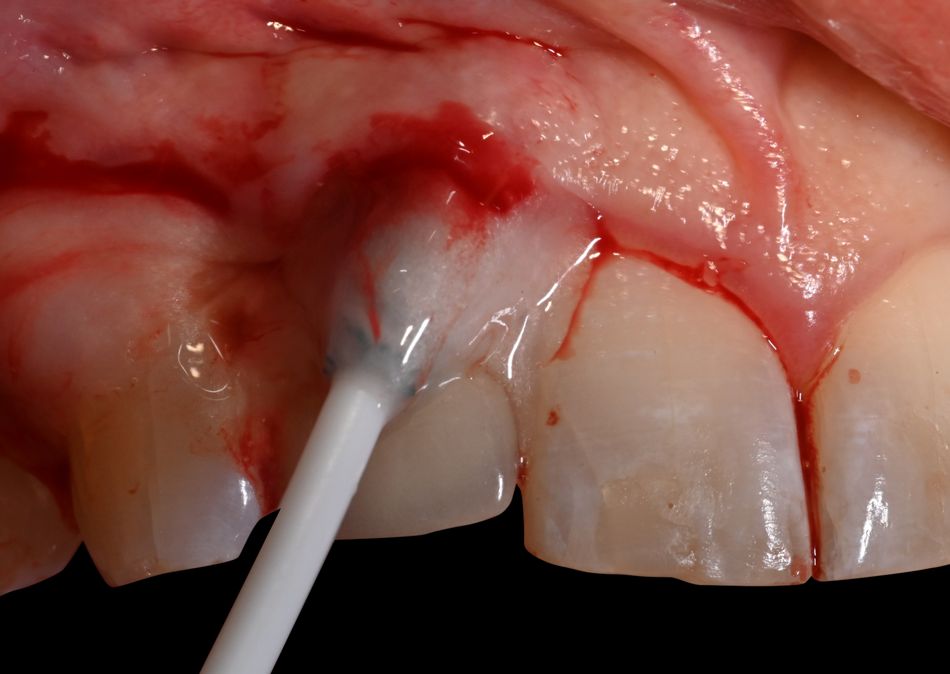
After local anesthesia with Xylocaine Dental Adrenaline (Xylocaine 20 mg/ml + epinephrine 12.5 μg/ml) an intracrevicular incision was placed circumferentially around the implant and papillae and extended to the line angles of tooth 13 and 11. A full-thickness mucoperiosteal flap was raised, and the implant with osseous defect was exposed and examined. Open flap debridement with removal of granulation tissue and calculus on the implant surface was performed with a titanium curette. After irrigation of the defect with sterile saline, the implant was debrided with Labrida BioClean™ soaked in Straumann® PrefGel® for approximately two minutes, followed by irrigation with sterile saline solution and the application of Straumann® EMDOGAIN® starting from the base of the defect.