Introduction
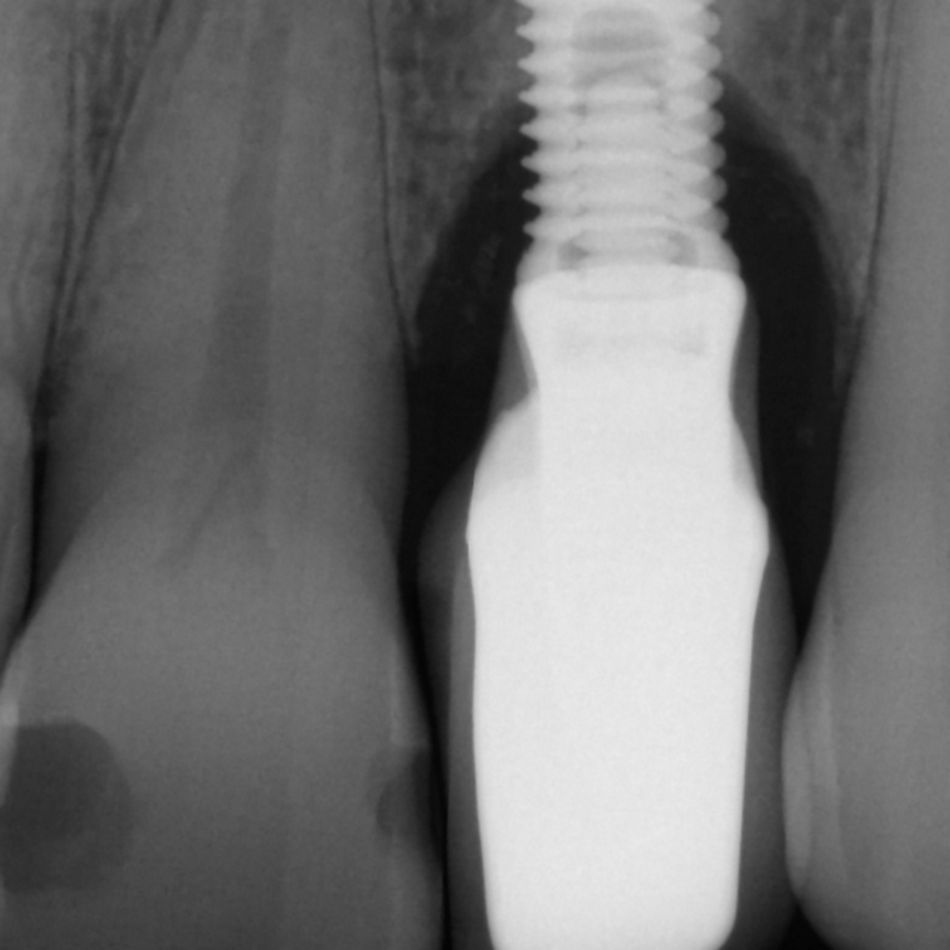
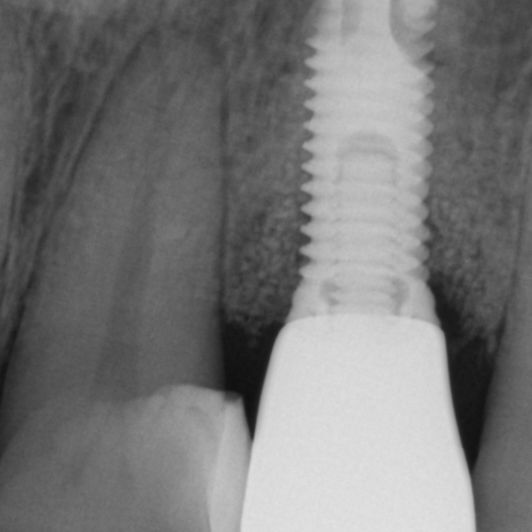
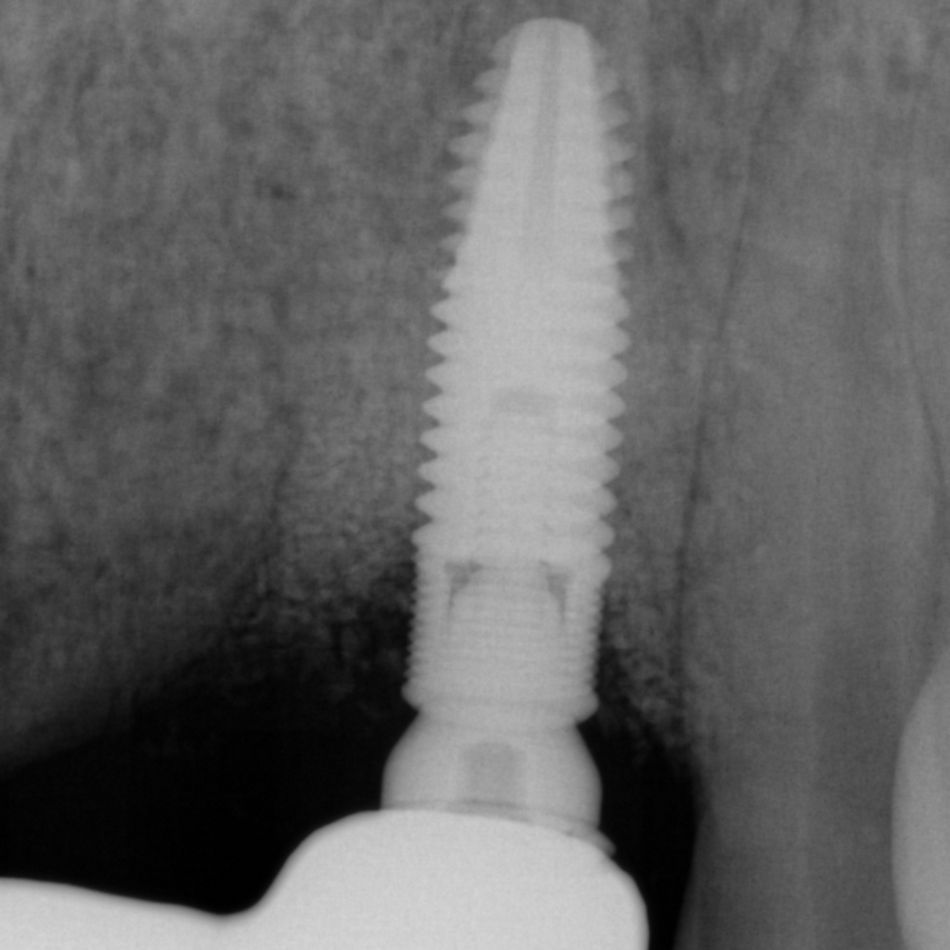
Peri-implantitis is a pathological condition occurring in tissues around dental implants and characterized by inflammation in the peri-implant connective tissue and progressive loss of supporting bone1.
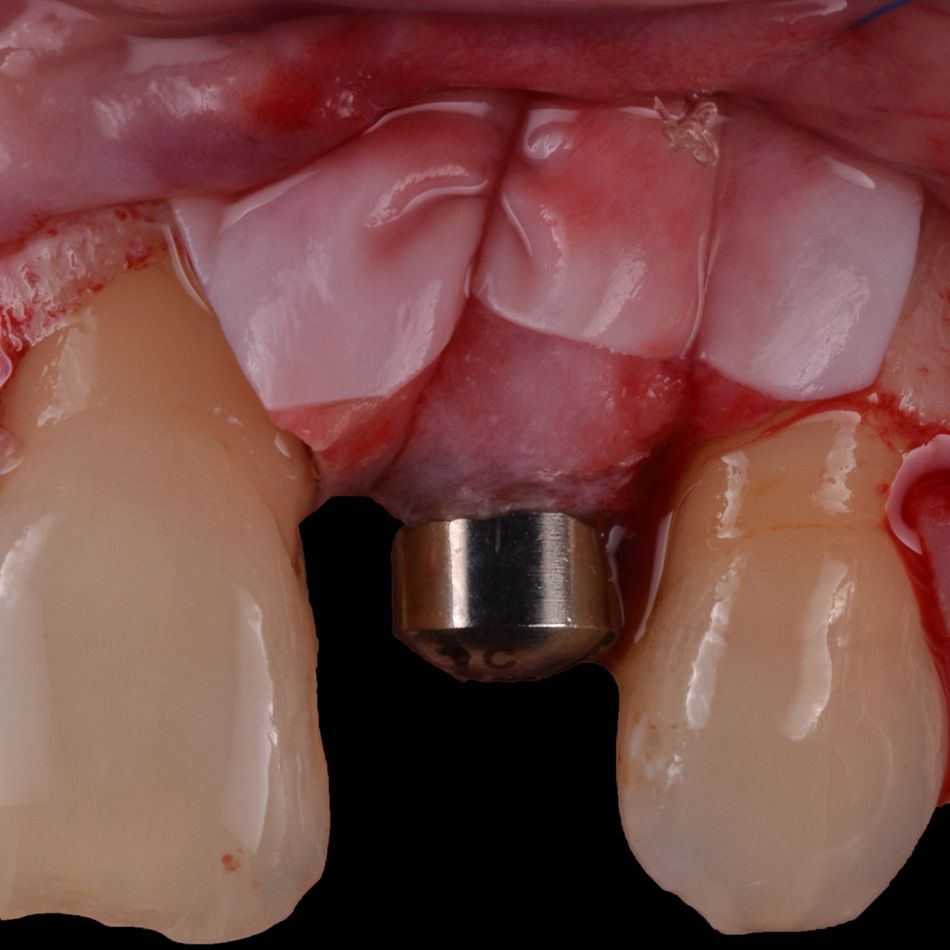
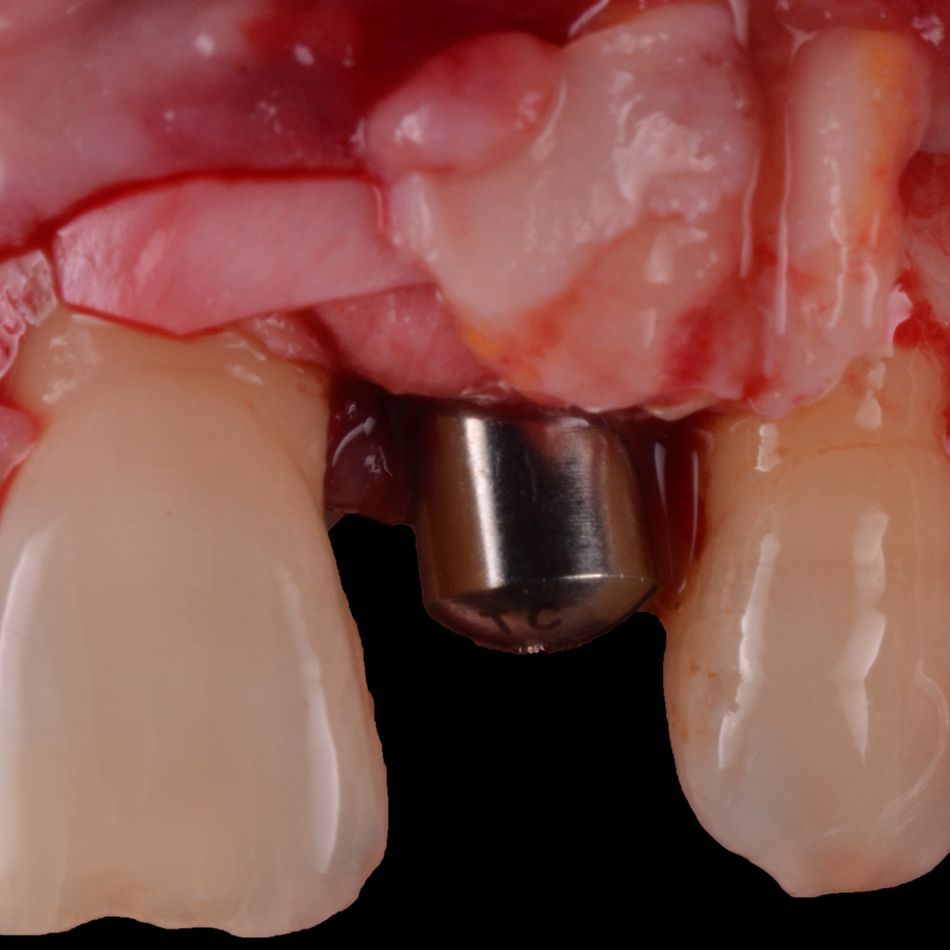
Particularly, peri-implantitis poses a significant clinical challenge in the esthetic zone due to its potential to cause mucosal recession. This condition can lead to visible changes in the appearance of the implant site, impacting overall esthetics. Managing peri-implantitis in such areas requires careful consideration and tailored strategies to prevent or address mucosal recession and preserve the esthetic outcome2.
In treating peri-implantitis, the goal is to reduce inflammation in soft tissues and stop further bone loss. Since nonsurgical methods have their limitations in achieving this goal, surgery is often recommended, and different techniques have been proposed based on factors like bone configuration and soft tissue characteristics3.
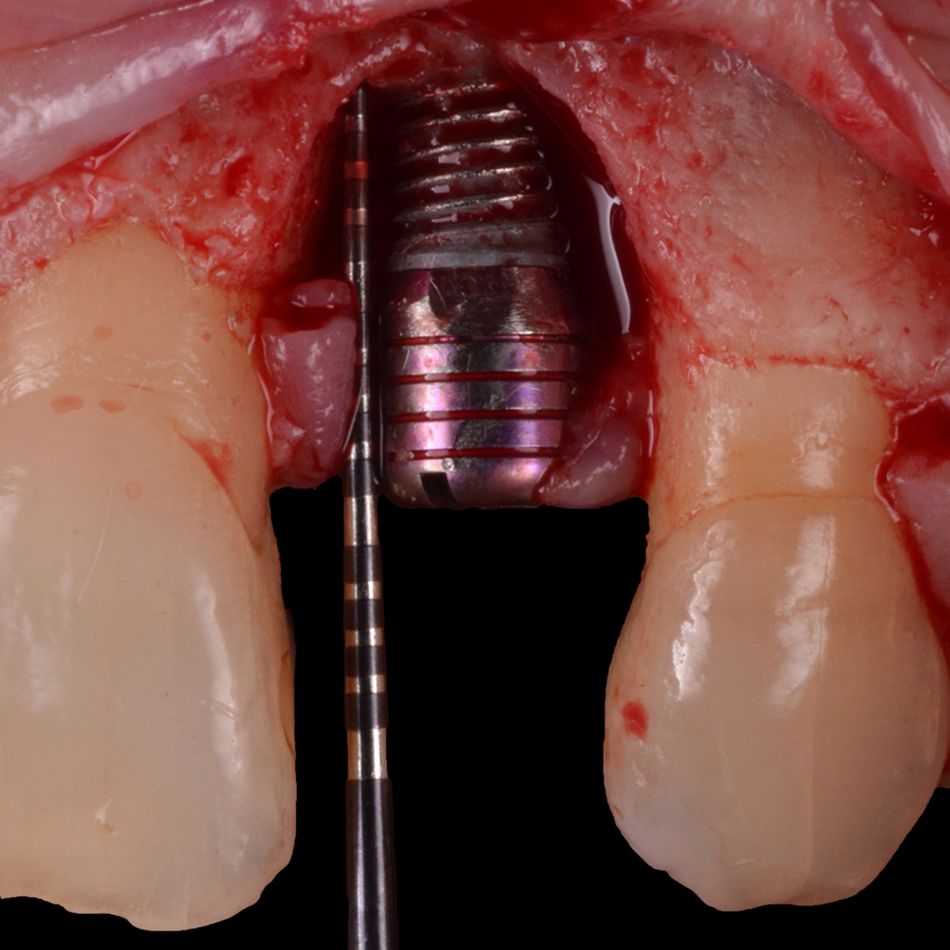
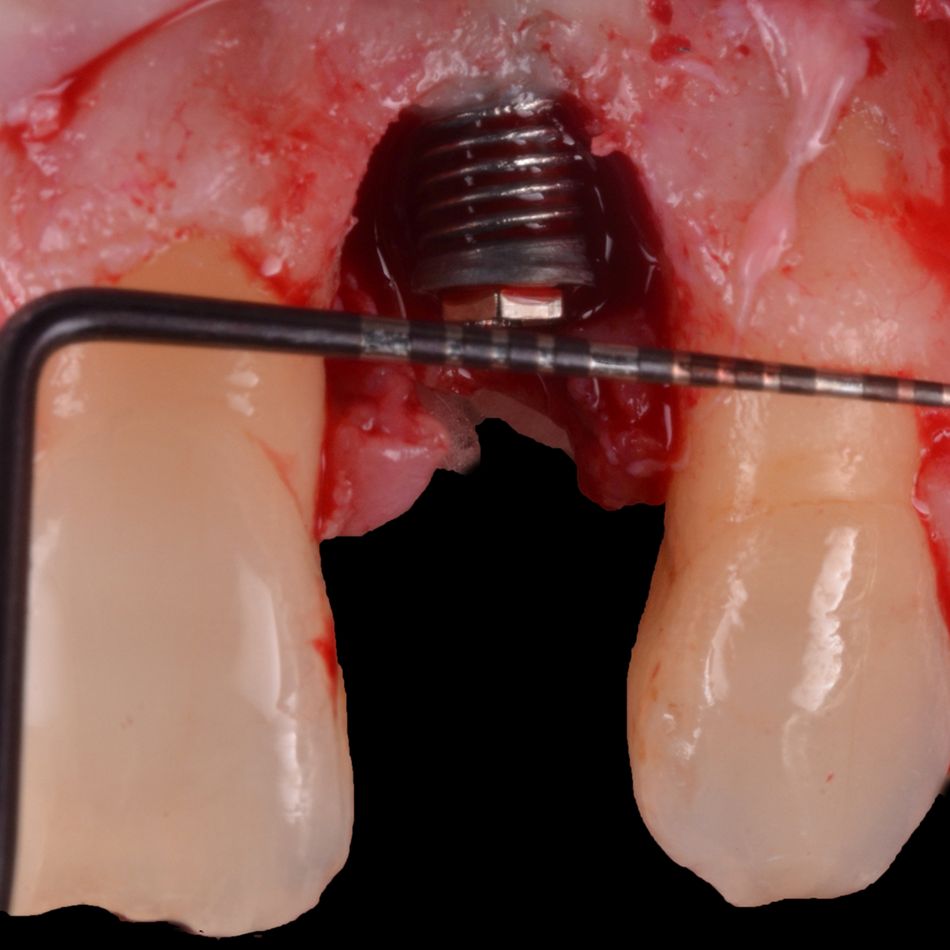
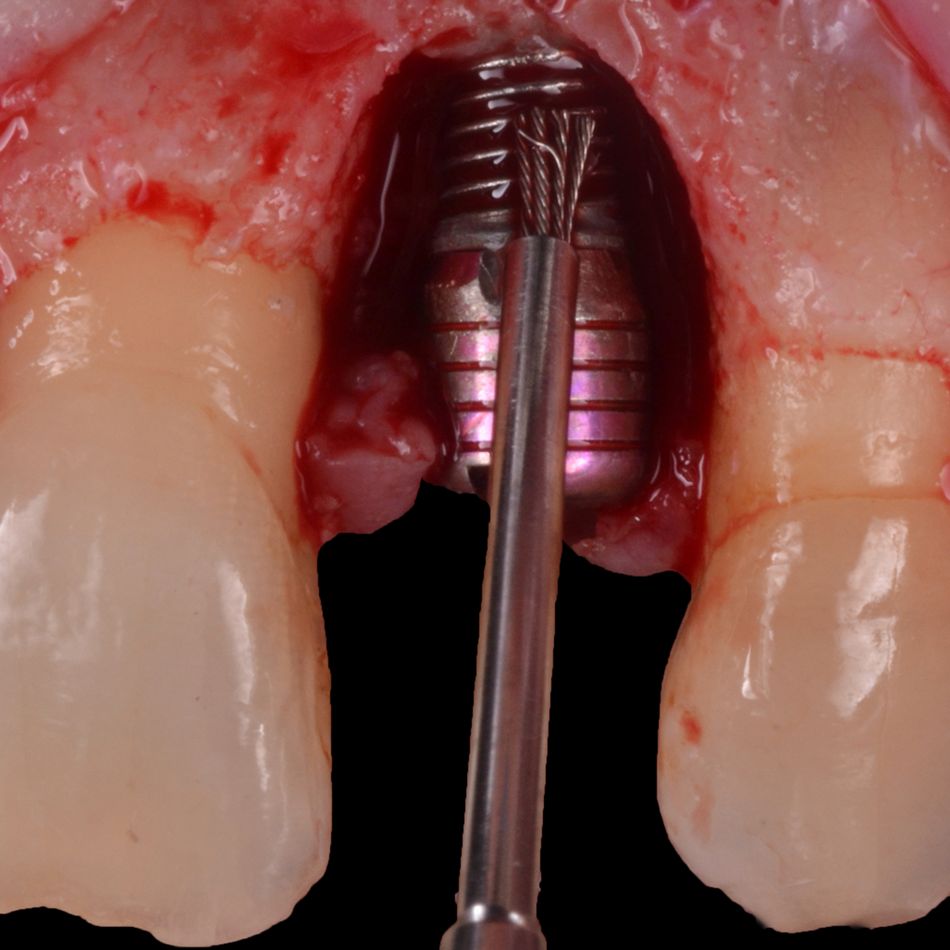
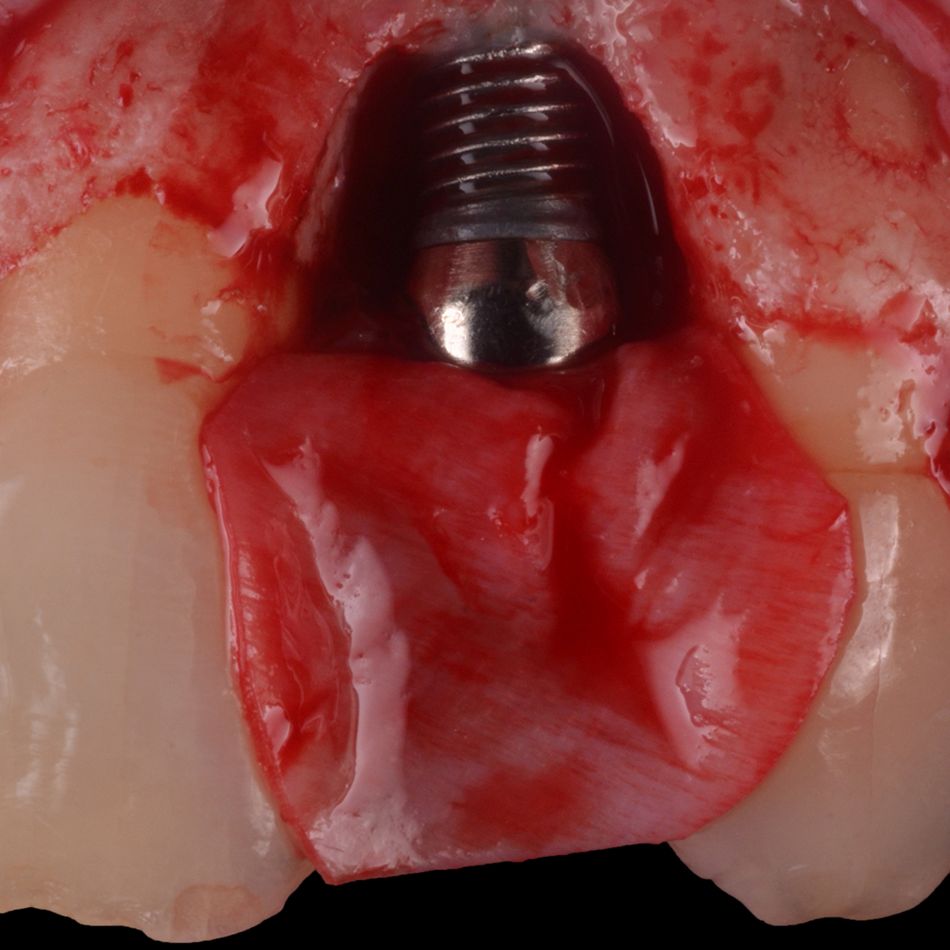
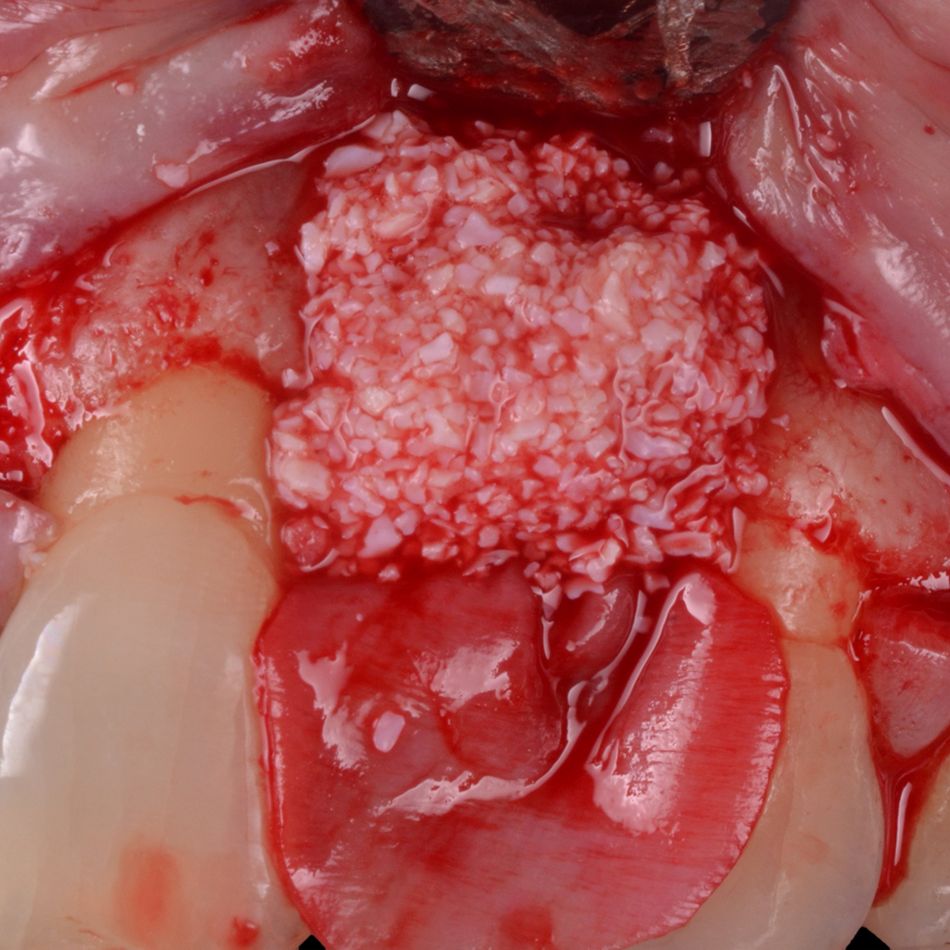
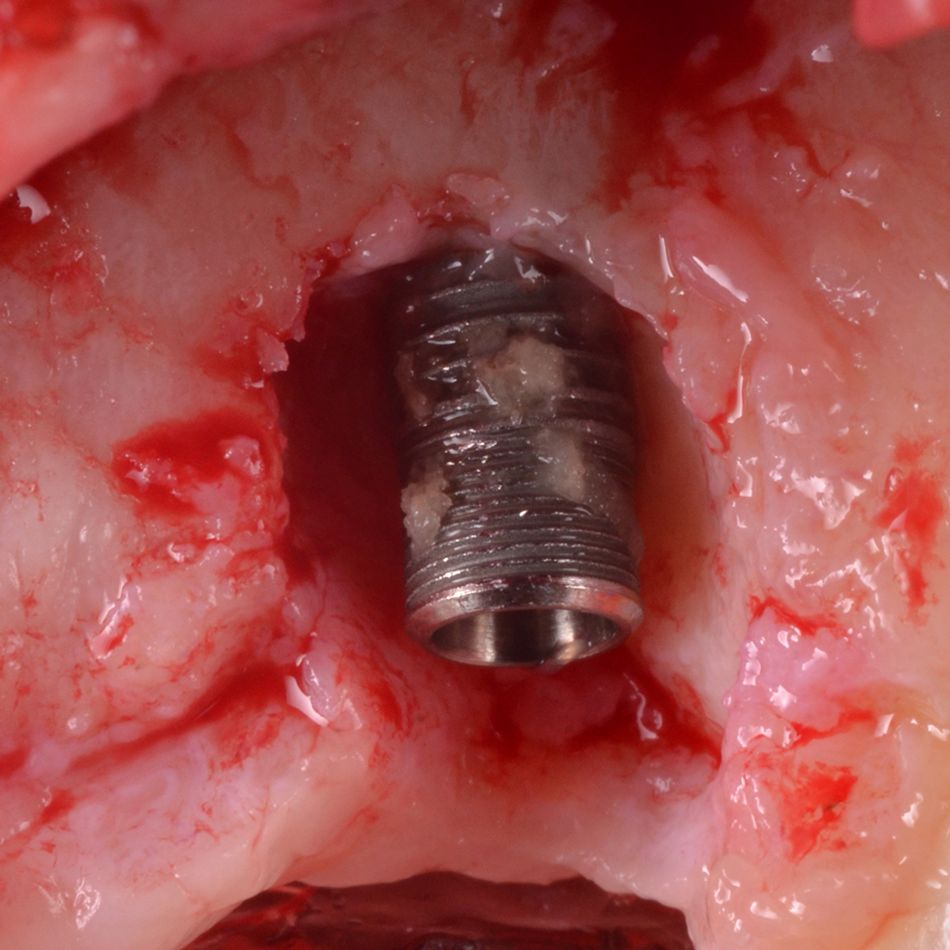
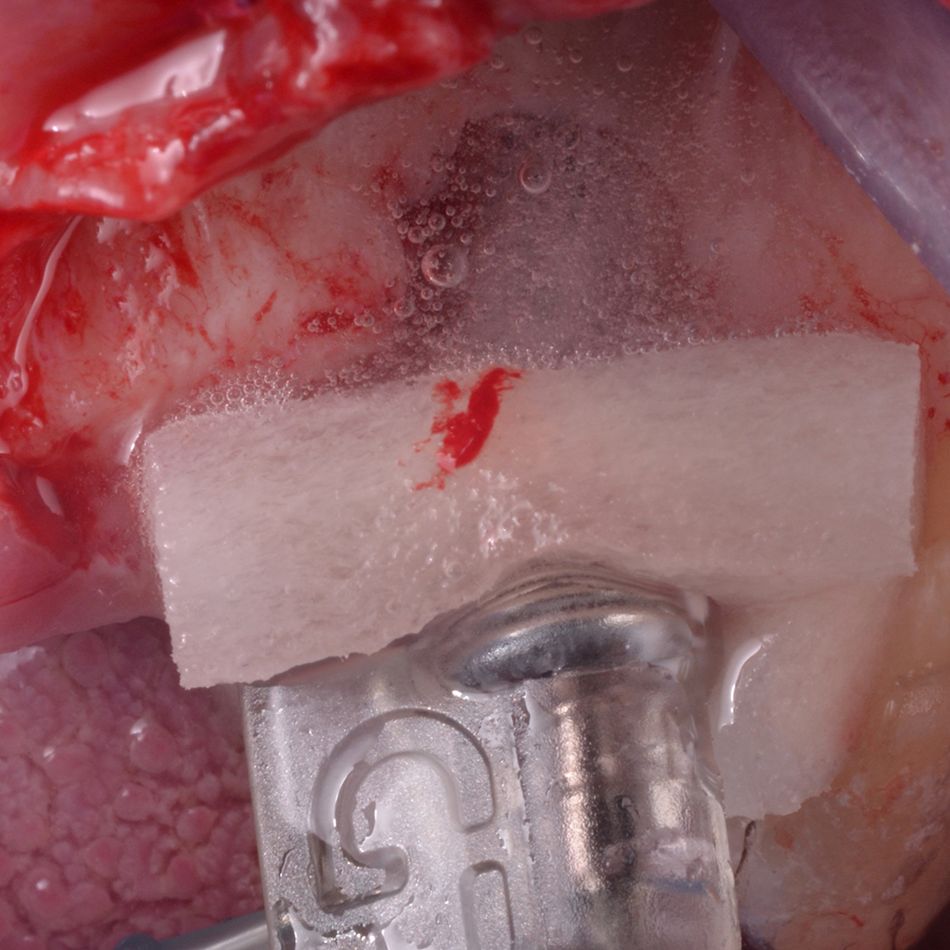
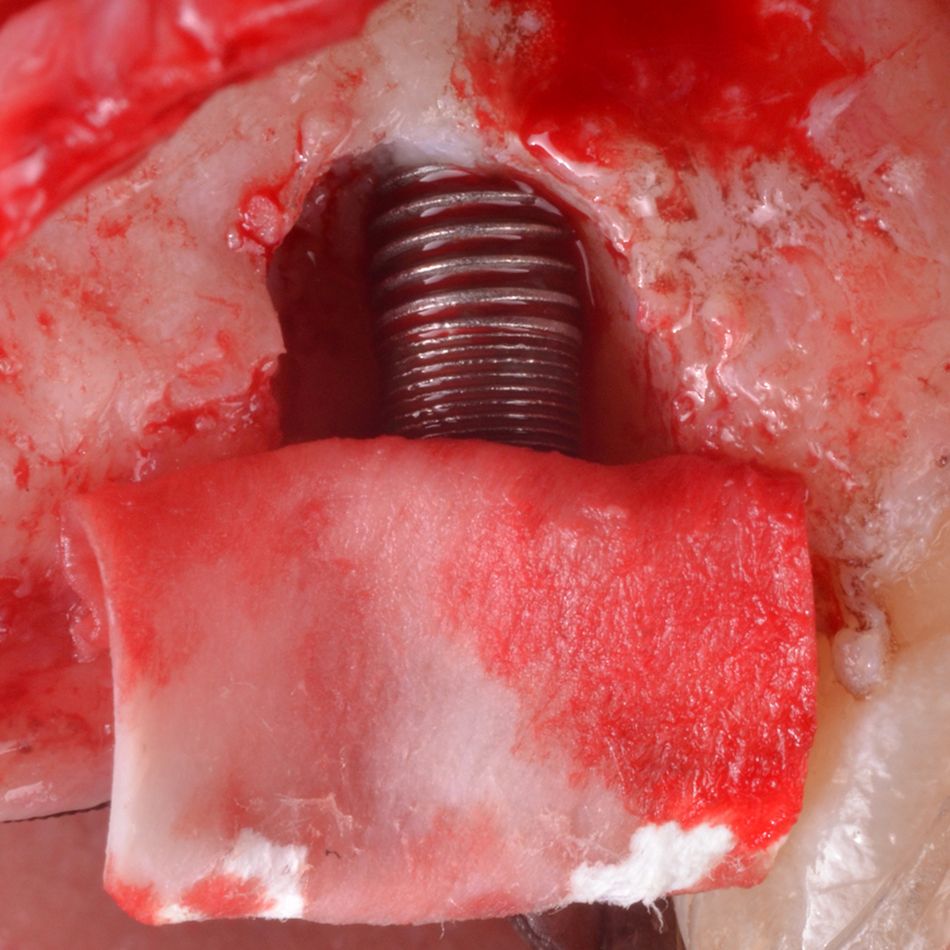
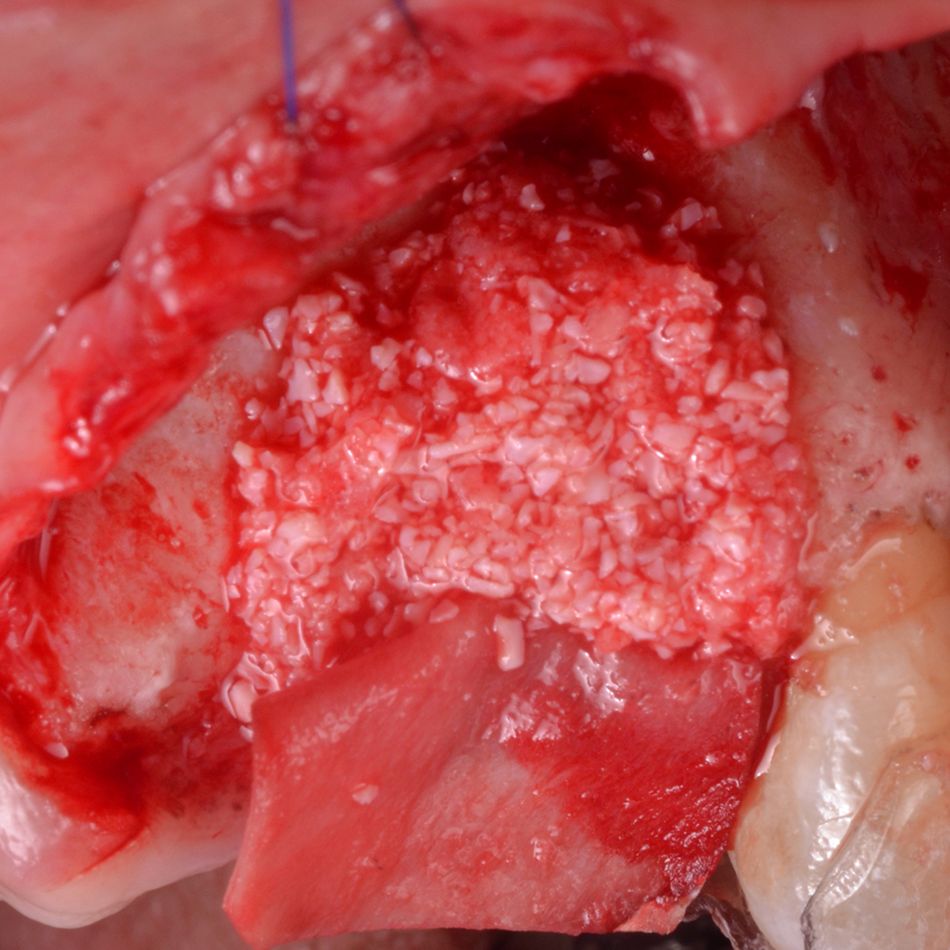
Before initiating any regenerative treatment, it is essential to eliminate biofilm around the dental implant. In recent years, several modalities and innovations have emerged for this purpose. One example is the GalvoSurge®️ Dental Implant Cleaning System, a biofilm-removal technology based on electrolytic cleaning. In just two minutes, GalvoSurge® removes bacterial biofilm from dental implants affected by peri-implantitis, setting the stage for bone grafting procedures.
This report unfolds a narrative of innovation in biofilm control and precision in bone regeneration, showcasing the potential of GalvoSurge®️ in treating peri-implantitis in two patients with affected peri-implant tissues within the esthetic zone4.
Keys for success
- The configuration of the peri-implant defect may play a pivotal role in achieving successful reconstructive outcomes, leading to disease resolution and marginal bone level gain.
- Narrow defect angle (<40 degrees) may further favor the reconstructive outcome.
- In cases where the implant is within the bony housing, the recommended approach involves surface decontamination followed by regeneration.
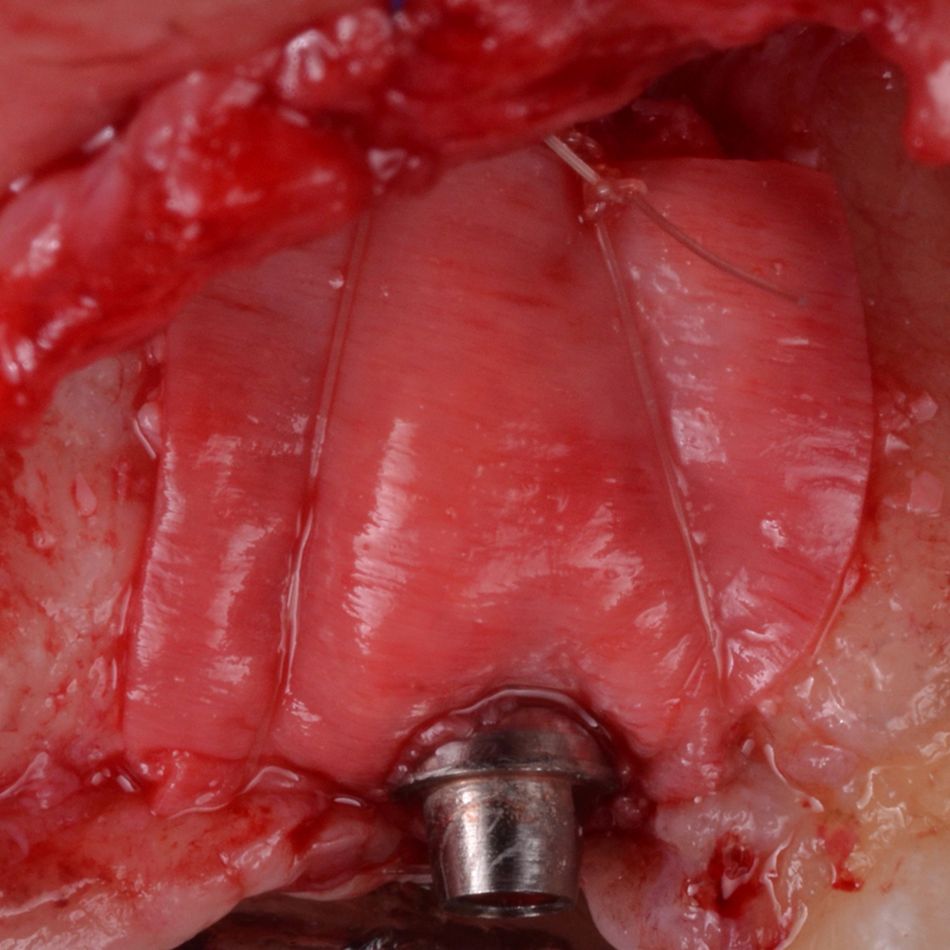
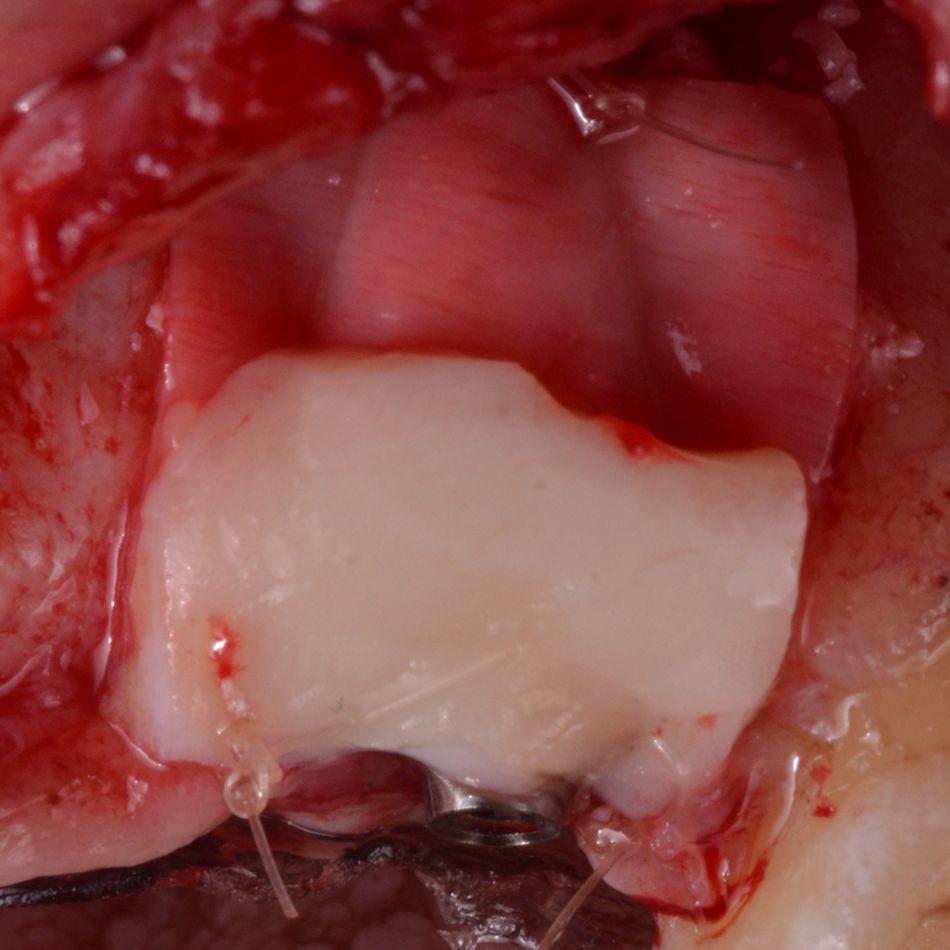
- In cases with a 2-wall defect configuration, the use of a barrier membrane is preferable. Meanwhile, in scenarios involving a well-contained defect configuration, barrier membrane might be optional.
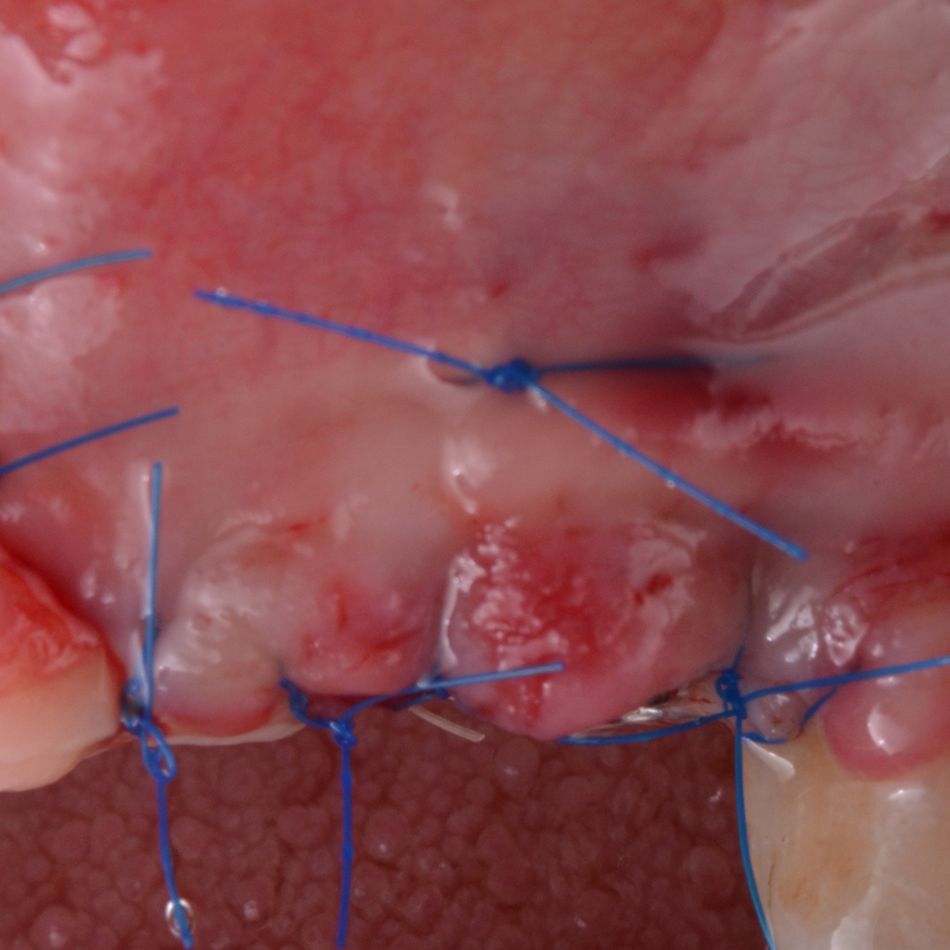
- For enhanced esthetic outcomes, soft tissue grafting using a connective tissue graft is advisable.